Maprotiline
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682158 |
| Pregnancy category |
|
| Routes of administration | oral, intramuscular, intravenous (infusion) |
| ATC code | N06AA21 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 66–70% |
| Protein binding | 88% |
| Metabolism | hepatic |
| Onset of action | 6 hours |
| Biological half-life | 27–58 hours |
| Excretion | biliar (30%) and urine (57%) as glucuronides, 3–4% as unchanged drug |
| Identifiers | |
| |
| CAS Number |
10262-69-8 |
| PubChem (CID) | 4011 |
| IUPHAR/BPS | 2402 |
| DrugBank |
DB00934 |
| ChemSpider |
23719117 |
| UNII |
2U1W68TROF |
| KEGG |
D02566 |
| ChEMBL |
CHEMBL21731 |
| ECHA InfoCard | 100.030.532 |
| Chemical and physical data | |
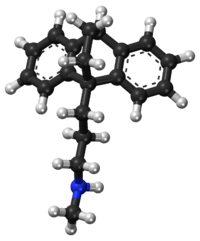
| Formula | C20H23N |
| Molar mass | 277.403 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Maprotiline (sold as Deprilept, Ludiomil, Psymion) is a medication that belongs to tetracyclic antidepressants (TeCA), a specific group of antidepressants.
History
Maprotiline was developed and has been marketed by the Swiss manufacturer Geigy (now operated by Novartis) since the early 1980s under the brand name Ludiomil. Generics are widely available.
Pharmacokinetics
After oral use absorption is good. It binds to plasma proteins 80–90%. Maximal plasma concentration is reached 6 hours after use. The mean time to peak is 12 hours. The half-life of elimination averages 51 hours.
Pharmacodynamics
Activity profile
Maprotiline exhibits strong effects as a norepinephrine reuptake inhibitor with only weak actions the reuptake of serotonin and dopamine.[1][2] It is also a strong antagonist of the H1 receptor, a moderate antagonist of the 5-HT2 and α1-adrenergic receptors, and a weak antagonist of the D2 and maCh receptors.
Maprotiline has also more recently been identified as a potent antagonist of the 5-HT7 receptor, with this action potentially playing an important role in its antidepressant effectiveness.[3]
Discussion
The pharmacological profile of maprotiline explains its antidepressant, sedative, anxiolytic, and sympathomimetic activities. In accordance to the pharmacological characteristics it is used in the treatment of depression, such as depression associated with agitation or anxiety. Additionally, it shows strong antagonism against reserpine-induced effects in animal studies, as do the other 'classical' antidepressants. Although maprotiline behaves in most regards as a 'first-generation antidepressant' it is commonly referred to as 'second-generation antidepressant'.
The postulated mechanism of maprotiline is that it acts primarily by potentiation of central adrenergic synapses by blocking reuptake of norepinephrine at nerve endings. This pharmacological action is thought to be primarily responsible for the drug's antidepressant and anxiolytic effects. It is a strong norepinephrine reuptake inhibitor with only weak effects on serotonin and dopamine reuptake. At higher doses however, maprotiline increases serotonergic transmission and increases the level of serotonin available.[4]
Indications
Maprotiline is used in the treatment of depression, such as depression associated with agitation or anxiety and has similar efficacy to the antidepressant drug moclobemide.[5]
- Treatment of depressions of all forms and severities (endogenous, psychotic, involutional, and neurotic) especially for depression associated with agitation or anxiety
- Panic disorder
- Neuropathic pain
- Treatment of the depressive phase in bipolar depression
- For the symptomatic relief of anxiety, tension or insomnia
The use of maprotiline in the treatment of enuresis in pediatric patients has so far not been systematically explored and its use is not recommended.[2]
Side effects
The side-effect profile is comparable to other tri-/tetracyclic antidepressants and many of the following are due to anticholinergic (which are less prominent than those of most tricyclic antidepressants) and antihistaminergic effects.[2] Most often seen are:
- Dizziness
- Drowsiness
- Somnolence
- fatigue
- Dry mouth (and complications of long-term uncontrolled dry mouth such as dental caries)
- Constipation
- Vertigo
- Nausea (rare, incidence of ~2%) and vomiting
- Increased appetite and weight gain
- Orthostatic hypotension, hypertension, sinus tachycardia, heart-block, arrhythmias and other cardiac effects
- Sexual dysfunction in men: impotence, priapism, delayed ejaculation, anejaculation, decreased libido
- Sexual dysfunction in women: decreased libido, vaginal dryness, painful sexual intercourse, anorgasmia
- Allergic skin reactions such as rash or urticaria (more often than with other antidepressants). Rarely, severe skin reactions such as erythema multiforme can occur.
- Photosensitivity
- Agitation, confusion
- Induction of hypomania or mania in patients suffering from underlying bipolar affective disorder
- Psychotic symptoms
- Tremor
- Extrapyramidal symptoms
- Headache
- Seizures (at high doses)
- Rare haematological complications: leukopenia and agranulocytosis (dangerous fall in white blood cells)
- Fever
- Urinary retention
Maprotiline causes a strong initial sedation (first 2 to 3 weeks of therapy) and is therefore indicated to treat agitated patients or those with suicidal risks. It causes anticholinergic side effects (dry mouth, constipation, confusion, tachycardia) with a lower incidence than amitriptyline. Originally, the manufacturer claimed that maprotiline is better tolerated than other tri-/tetracyclic drugs. However, seizures, leukopenia and skin reactions occur more often with maprotiline than with comparable drugs like amitriptyline.
Drug abuse and dependence
Maprotiline has no known potential for abuse and psychological dependence.
Withdrawal symptoms frequently seen when treatment with maprotiline is stopped abruptly (agitation, anxiety, insomnia, sometimes activation of mania or rebound depression) are not indicative of addiction and can be avoided by reducing the daily dose of maprotiline gradually by approximately 25% each week. If treatment has to be stopped at once due to medical reasons, the use of a benzodiazepine (e.g. lorazepam, clonazepam, or alprazolam) for a maximum of 4 weeks as needed will usually suppress withdrawal symptoms.
Contraindications
Maprotiline may worsen psychotic conditions like schizophrenia and should be given with caution. The antipsychotic treatment should be continued. Patients with bipolar affective disorder should not receive antidepressants whilst in a manic phase, as antidepressants can worsen mania.
Absolute
- Hypersensitivity to maprotiline or to other tri-/tetracyclic antidepressants
- Hypertrophy of the prostate gland with urine hesitancy
- Closed angle glaucoma
Special caution needed
- Concomitant treatment with a MAO-inhibitor
- Serious impairment of liver and kidney function
- Epilepsy and other conditions that lower the seizure threshold (active brain tumors, alcohol withdrawal, other medications)
- Serious cardiovascular conditions (arrhythmias, heart insufficience, state after myocardial infarction etc.)
- Treatment of patients under age 18[6]
Suicidal patients
Same as other antidepressants, maprotiline increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of maprotiline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Maprotiline is not approved for use in pediatric patients.[7]
Special populations
Pregnancy
Reproduction studies have been performed in female laboratory rabbits, mice, and rats at doses up to 1.3, 7, and 9 times the maximum daily human dose respectively and have revealed no evidence of impaired fertility or harm to the fetus due to maprotiline. There are, however, no adequate and well controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing mothers
Maprotiline is excreted in breast milk. At steady-state, the concentrations in milk correspond closely to the concentrations in whole blood. Caution should be exercised when maprotiline hydrochloride is administered to a nursing woman.
Pediatric use
Safety and effectiveness in the pediatric population have not been established. Anyone considering the use of Maprotiline in a child or adolescent must balance the potential risks with the clinical need.
Elderly patients
In general, lower dosages are recommended for patients over 60 years of age. Dosages of 50 mg to 75 mg daily are usually satisfactory as maintenance therapy for elderly patients who do not tolerate higher amounts.[8][9]
Interactions
Maprotiline has a wide range of possible interactions. Some are typical for tri-/tetracyclic antidepressants, others are caused by specific metabolic effects (e.g. high plasma-protein-binding) of maprotiline:
- Irreversible MAO-inhibitors: agitation, delirium, coma, hyperpyrexia (high fever), seizures and severe changes in blood pressure. Treatment-resistant and hospitalized patients may be treated concomitantly with an MAO-inhibitor, if they are closely monitored and if the initial dose of the MAO-Inhibitor is low.
Increased drug actions:
- Other antidepressants, barbiturates, narcotics, sedating antihistaminics, anticonvulsive drugs, alcohol - resulting in increased central depression
- Anticholinergics (antiparkinsonian agents, tri- and tetracyclic antidepressants) - resulting in increased anticholinergic action (dry mouth, constipation etc.)
- Sympathomimetics (also those used in local anesthetics like noradrenaline) : sympathomimetic effects increased (increased blood pressure, pulse rate, paleness of skin etc.)
- Nitrates and antihypertensives (e.g. beta-blockers) - increased antihypertensive action with pronounced fall in blood pressure
Decreased drug actions:
- Guanethidine, Reserpine, Guanfacine : antihypertensive effects decreased
- Clonidine : antihypertensive effects decreased and risk of (massive) rebound hypertension.
Other types of interaction:
- Drugs, which induce certain enzymes in the liver, e.g. barbiturates, phenytoin, carbamazepine and oral anticonceptive drugs, enhance the elimination of maprotiline and decrease its antidepressant effects. Additionally the blood-concentrations of phenytoin or carbamazepine may be increased, leading to a higher incidents of side effects.
- The concomitant use of maprotiline and neuroleptics can lead to increased maprotiline blood-levels and to seizures. Combining maprotiline and thioridazine could induce severe arrhythmias.
- Additionally, increased blood-levels of Maprotiline are possible, if certain beta-blocking agents (e.g. Propranolol) are given concomitantly.
- Maprotiline may amplify the actions of coumarin-type anticogulants (e.g. warfarin, phenprocoumon). The plasma-prothrombin-activity must be assessed closely in order to avoid overt bleedings.
- Maprotiline can increase the actions of oral antidiabetic drugs (sulfonylureas) and Insulin. Diabetic patients should have regular assessments of their blood-glucose-levels.
- The concomitant application with fluoxetine or fluvoxamine may lead to significantly increased plasma-levels of maprotiline with a high incidence of maprotiline side effects. Due to the long half-lives of fluoxetine and fluvoxamine this effect may persist.
Dose forms
- Coated Tablets, 10 mg, 25 mg, 50 mg, and 75 mg
- Injectable concentrate, 25 mg
Brand names
- Ludiomil, Deprilept, Psymion
- Generics
See also
Notes
- ↑ Peng, Wen-Huang; Kuan-Lin Lo; Yi-Hsuen Lee; Tai-Huang Hung; Ying-Chih Lin (2007). "Berberine produces antidepressant-like effects in the forced swim test and in the tail suspension test in mice". Life Sciences. 81 (11): 933–938. doi:10.1016/j.lfs.2007.08.003. PMID 17804020.
- 1 2 3 "DRUGDEX Evaluations - Maprotiline". Retrieved 25 April 2013.
- ↑ Matthys A, Haegeman G, Van Craenenbroeck K, Vanhoenacker P (June 2011). "Role of the 5-HT7 receptor in the central nervous system: from current status to future perspectives". Mol. Neurobiol. 43 (3): 228–53. doi:10.1007/s12035-011-8175-3. PMID 21424680.
- ↑ Miyake K, Fukuchi H, Kitaura T, Kimura M, Kimura Y, Nakahara T (1991). Pharmacokinetics of maprotiline and its demethylated metabolite in serum and specific brain regions of rats after acute and chronic administration of maprotiline. J Pharm Sci.;80(12):1114-8.
- ↑ Delini-Stula A, Mikkelsen H, Angst J (October 1995). "Therapeutic efficacy of antidepressants in agitated anxious depression--a meta-analysis of moclobemide studies". J Affect Disord. 35 (1-2): 21–30. doi:10.1016/0165-0327(95)00034-K. PMID 8557884.
- ↑ Simeon J, Maguire J, Lawrence S (1981). Maprotiline effects in children with enuresis and behavioural disorders. Progress in Neuro-Psychopharmacology 5 ( 5–6), 495–8
- ↑ U.S. National Library of Medicine. Last Reviewed 1 Sept. 2010 Medline Plus entry for Maprotiline
- ↑ http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682158.html. Retrieved 29 September 2013.
- ↑ http://www.drugs.com/pro/maprotiline.html. Retrieved 29 September 2013.
References
- B. Bandelow, S. Bleich, S. Kropp : Handbuch Psychopharmaka (German), 2nd. edition, 2004
- Benkert, Hippius : Kompendium der Psychiatrischen Pharmakotherapie (German), 4th. edition, 2003