Fexofenadine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Allegra, Axodin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697035 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | R06AX26 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 30-41%[1] |
| Protein binding | 60-70%[2] |
| Metabolism | Hepatic (≤5% of dose)[2] |
| Biological half-life | 14.4 hours |
| Excretion | Feces (~80%) and urine (~10%) as unchanged drug[2] |
| Identifiers | |
| |
| CAS Number |
83799-24-0 |
| PubChem (CID) | 3348 |
| IUPHAR/BPS | 4819 |
| DrugBank |
DB00950 |
| ChemSpider |
3231 |
| UNII |
E6582LOH6V |
| KEGG |
D07958 |
| ChEBI |
CHEBI:5050 |
| ChEMBL |
CHEMBL914 |
| ECHA InfoCard | 100.228.648 |
| Chemical and physical data | |
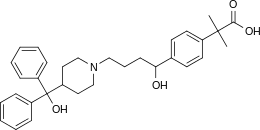
| Formula | C32H39NO4 |
| Molar mass | 501.68 g/mol |
| 3D model (Jmol) | Interactive image |
| Chirality | Racemic mixture |
| |
| |
| | |
Fexofenadine (trade names Allegra, Fexidine, Telfast, Fastofen, Tilfur, Vifas, Telfexo, Allerfexo, Flexofen) is an antihistamine pharmaceutical drug used in the treatment of allergy symptoms, such as hay fever, nasal congestion, and urticaria.[3] Therapeutically, fexofenadine is a selective peripheral H1-blocker.
Fexofenadine is classified as a second-generation antihistamine because it is less able to pass the blood-brain barrier and cause sedation, compared to first-generation antihistamines.[4][5] It has also been called a third-generation antihistamine, although there is some controversy associated with the use of the term.[6]
Fexofenadine has been manufactured in generic form since 2011.[7]
Medical uses
Fexofenadine is used for relief from physical symptoms associated with seasonal allergic rhinitis and for treatment of chronic urticaria.[4] It does not cure but rather prevents the aggravation of allergic rhinitis and chronic idiopathic urticaria and reduces the severity of the symptoms associated with those conditions, providing relief from repeated sneezing, runny nose, itchy eyes or skin, and general body fatigue.
Dosage
Fexofenadine has been demonstrated to be safe and effective for children ages 2–5 years old and 6–11 years old in treatment of seasonal allergic rhinitis.[8][9] Recommended doses of fexofenadine in UK labeling referenced below are: For adults with seasonal allergic rhinitis (hay fever): 60 mg twice daily or 120 mg taken once a day. For children aged 6–12 years with seasonal allergic rhinitis (hay fever): 30 mg taken twice a day, in the morning and evening. For adults with chronic urticaria: 180 mg taken once a day. For adults with chronic nasal congestion.
- Renal Impairment: Due to decreased renal elimination in patients with creatinine clearance of less than 80mL/min, it is recommended that patients with renal impairment are started on a lower dose.[10]
- Hepatic Impairment: Perhaps because only a small percentage of fexofenadine is metabolized in the liver, altered levels of drug are not seen in patients with hepatic impairment and therefore doses do not need to be adjusted in this population.[10]
Side effects
The most common side effect demonstrated in adults was headache, but some also experienced back and muscle pain, miosis or pinpoint pupils, nausea, drowsiness, and menstrual cramps. There have also been rare reports of anxiety and insomnia. The most common side effects demonstrated during clinical trials were cough, upper respiratory tract infection, fever, and otitis media for children ages 6 to 11 and fatigue for children ages 6 months to 5 years.[10]
Additionally, the half-life of fexofenadine is shorter than cetirizine, which could indicate the need for twice daily dosing, although labeling often denotes dosing once a day.[11] However, there is also evidence that cetirizine causes more sleepiness than fexofenadine.[12]
Overdose
The safety profile of fexofenadine is quite favorable, as no cardiovascular or sedative effects have been shown to occur even when taking 10 times the recommended dose.[13] Research on humans ranges from a single 800 mg dose, to a twice-daily 690 mg dose for a month, with no clinically significant adverse effects, when compared to a placebo. No deaths occurred in testing on mice, at 5000 mg/kg body weight, which is one-hundred and ten times (110x) the maximum recommended dose for an adult human.[10] If overdose were to occur, supportive measures are recommended. Theoretically, an overdose could present as dizziness, dry mouth, and/or drowsiness, consistent with an exaggeration of the usual side effects. It does not appear that hemodialysis is an effective mode to remove fexofenadine from the blood.[10]
Mechanism of action
Fexofenadine is a selectively peripheral H1-blocker. Blockage prevents the activation of the H1 receptors by histamine, preventing the symptoms associated with allergies from occurring. Fexofenadine does not readily cross the blood–brain barrier and is therefore less likely to cause drowsiness in comparison to other antihistamines that readily cross the blood-brain barrier (i.e. first-generation antihistamines like diphenhydramine). In general, fexofenadine takes about one hour to take effect, though this may be affected by the choice of dosage form and the presence/absence of certain foods.
Fexofenadine also exhibits no anticholinergic, antidopaminergic, alpha1-adrenergic, or beta-adrenergic-receptor-blocking effects.[10]
Pharmacokinetics
- Absorption: After oral application, maximum plasma concentrations are reached after two to three hours. Fexofenadine should not be taken with a high fat meal, as mean concentrations of fexofenadine in the bloodstream are seen to be reduced from 20-60% depending on form of medication (tablet, ODT, or suspension).[10]
- Distribution: Fexofenadine is 60-70% bound to plasma proteins, mostly albumin.[10]
- Metabolism: Fexofenadine is a substrate of CYP3A4. However, only about 5% is metabolized by the liver, indicating that the role of hepatic metabolism is relatively minor in its clearance from the body.[10]
- Elimination: Most of the substance is eliminated unchanged via the feces (80%) and urine (11–12%).[10]
Interactions
Taking erythromycin or ketoconazole while taking fexofenadine does increase the plasma levels of fexofenadine, but this increase does not influence the QT interval. The reason for this effect is likely due to transport-related effects, specifically involving p-glycoprotein (p-gp).[10] Both erythromcin and ketoconazole are inhibitors of p-gp, a transporter protein involved in preventing the intestinal absorption of fexofenadine. When p-gp is inhibited, fexofendaine may be better absorbed by the body, increasing its plasma concentration by more than what was intended.
Fexofenadine is not to be taken with apple, orange, or grapefruit juice because it could decrease absorption of the drug and should therefore be taken with water.[10] Grapefruit juice can significantly reduce the plasma concentration of fexofenadine.[14]
Antacids containing aluminium or magnesium should not be taken within 15 minutes of fexofenadine as they reduce the absorption of fexofenadine by almost 50%.[10]
Meals with high amounts of fat decrease the absorption of fexofenadine by about 50%.[10]
Special populations
Fexofenadine is a pregnancy category C and should be used if the benefits outweigh the risks.[15]
No studies have been done to evaluate the presence of fexofenadine in breast milk. Therefore, nursing women are urged to take caution while using fexofenadine.[10]
No sufficient studies have been done in patients over age 65. Therefore, it is advised that elderly patients use caution when using fexofenadine, particularly when there is concern for renal impairment.[10]
History
The older antihistaminic agent terfenadine was found to metabolize into the related carboxylic acid, fexofenadine. Fexofenadine was found to retain all of the biological activity of its parent while giving fewer adverse reactions in patients, so terfenadine was replaced in the market by its metabolite.[16] Fexofenadine was originally synthesized in 1993 by Massachusetts-based biotechnology company Sepracor, which then sold the development rights to Hoechst Marion Roussel (now part of Sanofi-Aventis), and was later approved by the Food and Drug Administration (FDA) in 1996. Albany Molecular Research Inc. (AMRI) holds the patents to the intermediates and production of fexofenadine HCl along with Roussel. Since that time, it has achieved blockbuster drug status with global sales of $1.87B USD in 2004 (with $1.49B USD coming from the United States). AMRI received royalty payments from Aventis that enabled the growth of AMRI.
On January 25, 2011, the FDA approved over-the-counter sales of fexofenadine in the United States, and Sanofi-Aventis' version became available on March 4, 2011.[17]
See also
References
- ↑ Lappin G, Shishikura Y, Jochemsen R, Weaver RJ, Gesson C, Houston B, Oosterhuis B, Bjerrum OJ, Rowland M, Garner C (May 2010). "Pharmacokinetics of fexofenadine: evaluation of a microdose and assessment of absolute oral bioavailability". Eur J Pharm Sci. 40 (2): 125–31. doi:10.1016/j.ejps.2010.03.009. PMID 20307657.
- 1 2 3 Smith, SM; Gums, JG (July 2009). "Fexofenadine: biochemical, pharmacokinetic and pharmacodynamic properties and its unique role in allergic disorders.". Expert Opinion on Drug Metabolism & Toxicology. 5 (7): 813–22. doi:10.1517/17425250903044967. PMID 19545214.
- ↑ Bachert, C (May 2009). "A review of the efficacy of desloratadine, fexofenadine, and levocetirizine in the treatment of nasal congestion in patients with allergic rhinitis". Clin Ther. 31 (5): 921–44. doi:10.1016/j.clinthera.2009.05.017. PMID 19539095.
- 1 2 Compalati, E; Baena-Cagnani, R; Penagos, M; Badellino, H; Braido, F; Gómez, RM; Canonica, GW; Baena-Cagnani, CE (2011). "Systematic review on the efficacy of fexofenadine in seasonal allergic rhinitis: a meta-analysis of randomized, double-blind, placebo-controlled clinical trials.". International Archives of Allergy and Immunology. 156 (1): 1–15. doi:10.1159/000321896. PMID 21969990.
- ↑ Dicpinigaitis, P; Gayle, V (2003). "Effect of the second-generation antihistamine, fexofenadine, on cough reflex sensitivity and pulmonary function.". Br J Clin Pharmacol. 56(5): (1): 501–504. doi:10.1046/j.1365-2125.2003.01902.x.
- ↑ Camelo-Nunes, Inês Cristina (November 2006). "Novos anti-histamínicos: uma visão crítica (New antihistamines: a critical view)". Jornal de Pediatria (in Portuguese). 82 (5): S173–80. doi:10.1590/S0021-75572006000700007. ISSN 0021-7557. PMID 17136293.
- ↑ "Dr. Reddy's announces the launch of Over-the-Counter Fexofenadine HCl and Pseudoephedrine HCl extended release tablets". Dr. Reddy’s Laboratories Ltd. 30 August 2011. Retrieved 27 May 2016.
- ↑ Segall, N; Grubbe RE; Levy AL; Maloney MJ; Nayak AS; Kittner B; Quesada JT. (Jul–Aug 2008). "Pharmacokinetics, Safety and Tolerability of an Oral Suspension of Fexofenadine for Children with Allergic Rhinitis". Allergy Asthma Proc. 29 (4): 380–5. doi:10.2500/aap.2008.29.3136. PMID 18702885.
- ↑ Phan, H; Moeller, Nahata (2009). "Treatment of Allergic Rhinitis in Infants and Children: Efficacy and Safety of Second-Generation Antihistamines and the Leukotriene Receptor Antagonist Montelukast". Drugs. 69 (18): 2541–76. doi:10.2165/9884960-000000000-00000. PMID 19943707.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Prescribing Information. Allegra (fexofenadine). Bridgewater, NJ: Sanofi-Aventis, July 2007.
- ↑ Church, Martin; Church, Diana (2013). "Pharmacology of antihistamines". Indian Journal of Dermatology. 58 (3): 219–224. doi:10.4103/0019-5154.110832. PMC 3667286
 . PMID 23723474. Also Church, Martin; Church, Diana (March 2011). "Pharmacology of antihistamines". World Allergy Organ J. 4: S22–7. doi:10.1097/WOX.0b013e3181f385d9. PMC 3666185
. PMID 23723474. Also Church, Martin; Church, Diana (March 2011). "Pharmacology of antihistamines". World Allergy Organ J. 4: S22–7. doi:10.1097/WOX.0b013e3181f385d9. PMC 3666185 . PMID 23282332.
. PMID 23282332. - ↑ Tashiro, M; Sakurada Y; Iwabuchi K; Mochizuki H; Kato M; Aoki M; Funaki Y; Itoh M; Iwata R; Wong DF; Yanai K (Aug 2004). "Central effects of fexofenadine and cetirizine: measurement of psychomotor performance, subjective sleepiness, and brain histamine H1-receptor occupancy using 11C-doxepin positron emission tomography.". J Clin Pharmacol. 44 (8): 890–900. doi:10.1177/0091270004267590. PMID 15286093.
- ↑ Philpot, EE (Jan–Feb 2000). "Safety of second generation antihistamines". Allergy Asthma Proc. 21 (1): 15–20. doi:10.2500/108854100778249033. PMID 10748947.
- ↑ Shirasaka, Y; Mori T; Murata Y; Nakanishi T; Tamai I (Feb 19, 2014). "Substrate- and Dose-Dependent Drug Interactions with Grapefruit Juice Caused by Multiple Binding Sites on OATP2B1". Pharm Res. 31 (8): 2035–2043. doi:10.1007/s11095-014-1305-7. PMID 24549825.
- ↑ Mazzotta, P; Loebstein R; Koren G (Apr 1999). "Treating allergic rhinitis in pregnancy. Safety considerations.". Drug Saf. 20 (4): 361–75. doi:10.2165/00002018-199920040-00005. PMID 10230583.
- ↑ Daniel Lednicer (1999). The Organic Chemistry of Drug Synthesis. 6. New York: Wiley Interscience. pp. 38–40. ISBN 0-471-24510-0.
- ↑ "Allegra | FAQs". Sanofi-Aventis. Retrieved 5 July 2011.
External links
- Fexofenadine (UK patient information leaflet)
- Allegra (Fexofenadine Hydrochloride) label and research information
- "fexofenadine" at medicinenet.com
- Official website for Allegra brand Fexofenadine