Phenelzine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Nardil |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682089 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | N06AF03 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Liver |
| Biological half-life | 11.6 hours |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number |
51-71-8 |
| PubChem (CID) | 3675 |
| IUPHAR/BPS | 7266 |
| DrugBank |
DB00780 |
| ChemSpider |
3547 |
| UNII |
O408N561GF |
| KEGG |
D08349 |
| ChEMBL |
CHEMBL1089 |
| ECHA InfoCard | 100.000.108 |
| Chemical and physical data | |
| Formula | C8H12N2 |
| Molar mass | 136.19 g/mol |
| 3D model (Jmol) | Interactive image |
| Boiling point | 74 °C (165 °F) |
| |
| |
| (verify) | |
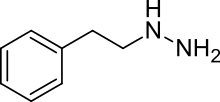
Phenelzine (Nardil, Nardelzine) is a non-selective and irreversible monoamine oxidase inhibitor (MAOI) of the hydrazine class which is used as an antidepressant and anxiolytic. Along with tranylcypromine and isocarboxazid, phenelzine is one of the few non-selective MAOIs still in widespread clinical use. It is typically available in 15 mg tablets and doses usually range from 30–90 mg per day, with 15 mg every day or every other day suggested as a maintenance dose following a successful course of treatment.
Indications
Phenelzine is used primarily in the treatment of major depressive disorder (MDD). Patients with depressive symptomology characterized as "atypical", "nonendogenous", and/or "neurotic" respond particularly well to phenelzine.[1] The medication is also useful in patients who do not respond favorably to first and second-line treatments for depression, or are "treatment-resistant".[2] In addition to being a recognized treatment for major depressive disorder, phenelzine is effective in treating dysthymia,[3] bipolar depression (BD),[4] panic disorder (PD),[5] social anxiety disorder,[6] bulimia,[7] and post-traumatic stress disorder (PTSD).[8]
Pharmacology
Pharmacodynamics
Phenelzine is a non-selective and irreversible inhibitor of the enzyme monoamine oxidase (MAO). It inhibits both of the respective isoforms of MAO, MAO-A and MAO-B, and does so almost equally, with slight preference for the former. By inhibiting MAO, phenelzine prevents the breakdown of the monoamine neurotransmitters serotonin, melatonin, norepinephrine, epinephrine, and dopamine, as well as the trace amine neuromodulators such as phenethylamine, tyramine, octopamine, and tryptamine. This leads to an increase in the extracellular concentrations of these neurochemicals and therefore an alteration in neurochemistry and neurotransmission. This action is thought to be the primary mediator in phenelzine's therapeutic benefits.
Phenelzine and its metabolites also inhibit at least two other enzymes to a lesser extent, of which are alanine transaminase (ALA-T),[9] and γ-Aminobutyric acid transaminase (GABA-T),[10] the latter of which is not caused by phenelzine itself, but by a phenelzine metabolite phenylethylidenehydrazine (PEH). By inhibiting ALA-T and GABA-T, phenelzine causes an increase in the alanine and GABA levels in the brain and body. GABA is the major inhibitory neurotransmitter in the mammalian central nervous system, and is very important for the normal suppression of anxiety, stress, and depression. Phenelzine's action in increasing GABA concentrations may significantly contribute to its antidepressant, and especially, anxiolytic/antipanic properties, the latter of which have been considered superior to those of other antidepressants. As for ALA-T inhibition, though the consequences of disabling this enzyme are currently not well understood, there is some evidence to suggest that it is this action of the hydrazines (including phenelzine) which may be responsible for the occasional incidence of hepatitis and liver failure.
Phenelzine has also been shown to metabolize to phenethylamine (PEA).[11] PEA acts as a releasing agent of norepinephrine and dopamine, and produces effects very similar to those of amphetamine, though with markedly different pharmacokinetics such as a far shorter duration of action. Phenelzine's enhancement of PEA levels may contribute further to its overall antidepressant effects to some degree. In addition, phenethylamine is a substrate for MAO-B, and treatment with MAOIs that inhibit MAO-B such as phenelzine have been shown to consistently and significantly elevate its concentrations.
Like many other antidepressants, phenelzine usually requires several weeks of treatment to achieve full therapeutic effects. The reason for this delay is not fully understood, but it is believed to be due to many factors, including achieving steady-state levels of MAO inhibition and the resulting adaptations in mean neurotransmitter levels, the possibility of necessary desensitization of autoreceptors which normally inhibit the release of neurotransmitters like serotonin and dopamine, and also the upregulation of enzymes such as serotonin N-acetyltransferase. Typically, a therapeutic response to MAOIs is associated with an inhibition of at least 80-85% of monoamine oxidase activity.[12]
Pharmacokinetics

Phenelzine is administered orally in the form of phenelzine sulfate and is rapidly absorbed from the gastrointestinal tract. Time to peak plasma concentration is 43 minutes and half-life is 11.6 hours. Unlike most other drugs, phenelzine irreversibly disables MAO, and as a result, it does not necessarily need to be present in the blood at all times for its effects to be sustained. Because of this, upon phenelzine treatment being ceased, its effects typically do not actually wear off until the body replenishes its enzyme stores, a process which can take as long as 2–3 weeks.
Phenelzine is metabolized primarily in the liver and its metabolites are excreted in the urine. Oxidation is the primary routine of metabolism, and the major metabolites are phenylacetic acid and parahydroxyphenylacetic acid, recovered as about 73% of the excreted dose of phenelzine in the urine over the course of 96 hours after single doses. Acetylation to N2-acetylphenelzine is a minor pathway. Phenelzine may also interact with cytochrome P450 enzymes, inactivating these enzymes through formation of a heme adduct. Two other minor metabolites of phenelzine, as mentioned above, include phenylethylidenehydrazine and phenethylamine.
Adverse effects
Common side effects of phenelzine may include dizziness, blurry vision, dry mouth, headache, lethargy, sedation, somnolence, insomnia, anorexia, weight gain or loss, nausea and vomiting, diarrhea, constipation, urinary retention, mydriasis, muscle tremors, hyperthermia, sweating, hypertension or hypotension, orthostatic hypotension, paresthesia, hepatitis, and sexual dysfunction (consisting of loss of libido and anorgasmia). Rare side effects usually only seen in susceptible individuals may include hypomania or mania, psychosis and acute liver failure, the last of which is usually only seen in people with pre-existing liver damage, old age, alcohol consumption, or viral infection.[13]
Interactions
The MAOIs are infamous for their problematic food restrictions and drug interactions. Hypertensive crisis may result from the overconsumption of tyramine-containing foods. As a result, patients on phenelzine and other MAOIs must avoid excess quantities of certain foods that contain tyramine such as aged cheeses and cured meats, among others. Serotonin syndrome may result from an interaction with certain drugs which increase serotonin activity such as selective serotonin reuptake inhibitors, serotonin releasing agents, and serotonin agonists. Several deaths have been reported due to drug interaction-related serotonin syndrome such as the case of Libby Zion.
As is the case with other MAOIs, there is a concern regarding phenelzine and the use of both local and general anesthetics. Anyone taking phenelzine should inform their psychiatrist before proceeding with dental surgery, and surgery in any other contexts.
Phenelzine has also been linked to vitamin B6 deficiency.[14] Transaminases such as GABA-transaminase have been shown to be dependent upon vitamin B6[15] and may be involved in a potentially related process, since the phenelzine metabolite phenylethylidenehydrazine (PEH) is a GABA transaminase inhibitor. Both phenelzine and vitamin B6 are rendered inactive upon these reactions occurring. For this reason, it may be recommended to supplement with vitamin B6 while taking phenelzine. The pyridoxine form of B6 is recommended for supplementation, since this form has been shown to reduce hydrazine toxicity from phenelzine and, in contrast, the pyridoxal form has been shown to increase the toxicity of hydrazines.[16]
See also
References
- ↑ Parke-Davis Division of Pfizer Inc. (2007). Nardil(R) (Phenelzine sulfate tablets, USP), labeling information. Retrieved December 14, 2009 from the U.S. Food and Drug Administration's Web site: http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/011909s038lbl.pdf
- ↑ Fiedorowicz, J. G.; Swartz, K. L. (2004). "The Role of Monoamine Oxidase Inhibitors in Current Psychiatric Practice". Journal of Psychiatric Practice. 10 (4): 239–248. doi:10.1097/00131746-200407000-00005. PMC 2075358
 . PMID 15552546.
. PMID 15552546. - ↑ Vallejo, J.; Gasto, C.; Catalan, R.; Salamero, M. (1987). "Double-blind study of imipramine versus phenelzine in Melancholias and Dysthymic Disorders". The British Journal of Psychiatry. 151 (5): 639–642. doi:10.1192/bjp.151.5.639. PMID 3446308.
- ↑ Quitkin, F. M.; Mcgrath, P.; Liebowitz, M. R.; Stewart, J.; Howard, A. (1981). "Monoamine oxidase inhibitors in bipolar endogenous depressives". Journal of Clinical Psychopharmacology. 1 (2): 70–74. doi:10.1097/00004714-198103000-00005. PMID 7028797.
- ↑ Buigues, J.; Vallejo, J. (1987). "Therapeutic response to phenelzine in patients with panic disorder and agoraphobia with panic attacks". The Journal of Clinical Psychiatry. 48 (2): 55–59. PMID 3542985.
- ↑ Blanco, C.; Schneier, F.; Schmidt, A.; Blanco-Jerez, C.; Marshall, R.; Sánchez-Lacay, A.; Liebowitz, M. (2003). "Pharmacological treatment of social anxiety disorder: a meta-analysis". Depression and Anxiety. 18 (1): 29–40. doi:10.1002/da.10096. PMID 12900950.
- ↑ Walsh, B. T.; Gladis, M.; Roose, S. P.; Stewart, J. W.; Stetner, F.; Glassman, A. H. (1988). "Phenelzine vs placebo in 50 patients with bulimia". Archives of General Psychiatry. 45 (5): 471–475. doi:10.1001/archpsyc.1988.01800290091011. PMID 3282482.
- ↑ Frank, J. B.; Kosten, T. R.; Giller El, E. L.; Dan, E. (1988). "A randomized clinical trial of phenelzine and imipramine for posttraumatic stress disorder". The American Journal of Psychiatry. 145 (10): 1289–1291. PMID 3048121.
- ↑ Tanay, V. A.; Parent, M. B.; Wong, J. T.; Paslawski, T.; Martin, I. L.; Baker, G. B. (2001). "Effects of the antidepressant/antipanic drug phenelzine on alanine and alanine transaminase in rat brain". Cellular and molecular neurobiology. 21 (4): 325–339. doi:10.1023/A:1012697904299. PMID 11775064.
- ↑ Mckenna, K. F.; Mcmanus, D. J.; Baker, G. B.; Coutts, R. T. (1994). "Chronic administration of the antidepressant phenelzine and its N-acetyl analogue: effects on GABAergic function". Journal of neural transmission. Supplementum. 41: 115–122. doi:10.1007/978-3-7091-9324-2_15. PMID 7931216.
- ↑ Dyck LE, Durden DA, Boulton AA (June 1985). "Formation of beta-phenylethylamine from the antidepressant, beta-phenylethylhydrazine". Biochemical Pharmacology. 34 (11): 1925–9. doi:10.1016/0006-2952(85)90310-7. PMID 4004908.
- ↑ Raft, D.; Davidson, J.; Wasik, J.; Mattox, A. (1981). "Relationship between response to phenelzine and MAO inhibition in a clinical trial of phenelzine, amitriptyline and placebo". Neuropsychobiology. 7 (3): 122–126. doi:10.1159/000117841. PMID 7231652.
- ↑ Gómez-Gil, E.; Salmerón, J. M.; Mas, A. (1996). "Phenelzine-induced fulminant hepatic failure". Annals of Internal Medicine. 124 (7): 692–693. doi:10.7326/0003-4819-124-7-199604010-00014. PMID 8607601.
- ↑ Malcolm, D. E.; Yu, P. H.; Bowen, R. C.; O'Donovan, C.; Hawkes, J.; Hussein, M. (1994). "Phenelzine reduces plasma vitamin B6". Journal of Psychiatry & Neuroscience. 19 (5): 332–334. PMC 1188621
 . PMID 7803366.
. PMID 7803366. - ↑ http://www.rcsb.org/pdb/explore.do?structureId=1ohw
- ↑ Dubnick, B.; Leeson, G. A.; Scott, C. C. (1960). "Effect of forms of vitamin B6 on acute toxicity of hydrazines". Toxicology and applied pharmacology. 2 (4): 403–409. doi:10.1016/0041-008X(60)90007-7. PMID 13818307.