Lithium (medication)
 | |
| Clinical data | |
|---|---|
| Trade names | Camcolit, Eskalith, Lithobid, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a681039 |
| Pregnancy category | |
| Routes of administration | Oral, parenteral |
| ATC code | N05AN01 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | depends on formulation |
| Protein binding | None |
| Metabolism | Renal |
| Biological half-life | 24 h, 36 h (elderly)[1] |
| Excretion | >95% renal |
| Identifiers | |
| |
| CAS Number | 7439-93-2 |
| PubChem (CID) | 28486 |
| DrugBank | DB01356 |
| Chemical and physical data | |
| Formula |
Li+ |
| Molar mass | 6.941 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
Lithium compounds, also known as lithium salts, are primarily used as a psychiatric medication. This includes in the treatment of major depressive disorder that does not improve following the use of other antidepressants and bipolar disorder.[1] In these disorders, it reduces the risk of suicide.[2] Lithium is taken by mouth.[1]
Common side effects include increased urination, shakiness of the hands, and increased thirst. Serious side effects include hypothyroidism, diabetes insipidus, and lithium toxicity. Blood level monitoring is recommended to decrease the risk of potential toxicity. If levels become too high, diarrhea, vomiting, poor coordination, sleepiness, and ringing in the ears may occur. If used during pregnancy, lithium can cause problems for the baby.[1] It appears to be safe to use while breastfeeding.[3] Lithium salts are classified as mood stabilizers. How they work is not specifically known.[1]
In the 1800s, lithium was used in people who had gout, epilepsy, and cancer. Its use in the treatment of mental disorder began in 1948 by John Cade in Australia.[4] It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[5] It is available as a generic medication.[1] The wholesale cost in the developing world in 2014 was between 0.12 and 0.20 USD per day.[6] In the United States at usual doses it costs about 0.90 to 1.20 USD per day.[1]
Medical uses
Lithium is used primarily for bipolar disorder.[1] It is sometimes used when other treatments are not effective in a number of other conditions, including major depression, schizophrenia, and some psychiatric disorders in children.[1] In mood disorders, of which bipolar is one, it decreases the risk of suicide.[7] This benefit is not seen with other medications.[8][9]
Bipolar disorder
Lithium carbonate treatment was previously considered to be unsuitable for children; however, more recent studies show its effectiveness for treatment of early-onset bipolar disorder in children as young as eight. The required dosage is slightly less than the toxic level, requiring close monitoring of blood levels of lithium carbonate during treatment.[10] A limited amount of evidence suggests lithium carbonate may contribute to treatment of substance abuse for some people with bipolar disorder.[11][12][13]
Suicide
High levels of naturally occurring lithium in drinking water have been associated with lower rates of suicide.[14][15][16]
Monitoring
Those who use lithium should receive regular serum level tests and should monitor thyroid and kidney function for abnormalities, as it interferes with the regulation of sodium and water levels in the body, and can cause dehydration. Dehydration, which is compounded by heat, can result in increasing lithium levels. The dehydration is due to lithium inhibition of the action of antidiuretic hormone, which normally enables the kidney to reabsorb water from urine. This causes an inability to concentrate urine, leading to consequent loss of body water and thirst.[17]
Lithium concentrations in whole blood, plasma, serum or urine may be measured using instrumental techniques as a guide to therapy, to confirm the diagnosis in potential poisoning victims or to assist in the forensic investigation in a case of fatal overdosage. Serum lithium concentrations are usually in the 0.5–1.3 mmol/l range in well-controlled people, but may increase to 1.8–2.5 mmol/l in those who accumulate the drug over time and to 3–10 mmol/l in acute overdose.[18][19]
Lithium salts have a narrow therapeutic/toxic ratio, so should not be prescribed unless facilities for monitoring plasma concentrations are available. Doses are adjusted to achieve plasma concentrations of 0.4[20][21] to 1.2 mmol Li+
/l (lower end of the range for maintenance therapy and the elderly, higher end for children) on samples taken 12 hours after the preceding dose.
Side effects
Sources for the following lists.[22][23][24][25][26][27][28][29]
- Very Common (>10% incidence) adverse effects of lithium include
- Confusion
- Constipation (usually transient, but can persist in some)
- Decreased memory
- Diarrhea (usually transient, but can persist in some)
- Dry mouth
- EKG changes — usually benign changes in T waves.
- Hand tremor (usually transient, but can persist in some)
- Headache
- Hyperreflexia — overresponsive reflexes.
- Leukocytosis — elevated white blood cell count
- Muscle weakness (usually transient, but can persist in some)
- Myoclonus — muscle twitching.
- Nausea (usually transient, but can persist in some)
- Polydypsia — increased thirst.
- Polyuria — increased urination.
- Renal (kidney) toxicity which may lead to chronic kidney failure
- Vomiting (usually transient, but can persist in some)
- Vertigo
- Weight gain
- Common (1-10%) adverse effects include
- Acne
- Extrapyramidal side effects — movement-related problems such as muscle rigidity, parkinsonism, dystonia, etc.
- Euthyroid goitre — i.e. the formation of a goitre despite normal thyroid functioning.
- Hypothyroidism — a deficiency of thyroid hormone.
- Hair loss/hair thinning
- Rare/Uncommon (<1%) adverse effects include
- Brugada syndrome — a potentially fatal abnormality in the electrical activity of the heart.
- Coma
- Erythema multiforme — a potentially fatal skin reaction
- Hallucinations
- Hypercalcaemia — elevated blood levels of calcium.
- Hypermagnesaemia — elevated blood levels of magnesium.
- Hyperparathyroidism — elevated blood levels of parathyroid hormone.
- Hyperthyroidism — elevated blood concentrations of thyroid hormones.
- Increased intracranial pressure and papilledema
- Myasthenia gravis — an autoimmune condition where the body's own defences attack the neuromuscular junction — the gap across which the nerves communicate with the muscles — leading to muscle weakness.
- Oedema
- Pseudotumor cerebri
- Renal interstitial fibrosis
- Seizure
- Sinus node dysfunction
- Transient reduction in peripheral circulation as a whole
- Unknown frequency adverse effects include
- Abdominal pain
- Albuminuria — protein in the urine, a sign of impaired kidney function.
- Bradycardia — low heart rate.
- Changes in taste
- Decreased creatinine clearance — another sign of impaired kidney function.
- Flatulence
- Gastritis
- Glycosuria — glucose (blood sugar) in the urine.
- Hyperthermia
- Hypotension — low blood pressure.
- Indigestion
- Nystagmus — involuntary eye movements that can interfere with vision.
- Oliguria — low urine output, although excess urine output is more likely.
- Sexual dysfunction including impotence, decreased libido, vaginal dryness, erectile dysfunction, etc.
- Slurred speech
- Somnolence
- Weight loss (gain is more common with prolonged treatment).
Lithium is known to be responsible for 1–2 kg of weight gain.[30] Weight gain may be a source of low self-esteem for the clinically depressed.[31]
In addition to tremors, lithium treatment appears to be a risk factor for development of parkinsonism symptoms, although the causal mechanism remains unknown. [32]
Most side effects of lithium are dose-dependent. The lowest effective dose is used to limit the risk of side effects.
Hypothyroidism
Most patients treated with lithium carbonate show elevated thyroid stimulating hormone levels in response to injections of thyrotropin-releasing hormone.[33] According to an Australian study, "The incidence of hypothyroidism is six-fold higher in people on lithium as compared to the general population. Hypothyroidism in turn increases the likelihood of developing clinical depression."[30]
Because lithium competes with the receptors for the antidiuretic hormone in the kidney, it increases water output into the urine, a condition called nephrogenic diabetes insipidus. Clearance of lithium by the kidneys is usually successful with certain diuretic medications, including amiloride and triamterene.[34] It increases the appetite and thirst ("polydypsia") and reduces the activity of thyroid hormone (hypothyroidism).[35][36][37][38] The latter can be corrected by treatment with thyroxine and does not require the lithium dose to be adjusted. Lithium is also believed to permanently affect renal function, although this does not appear to be common.[39]
Pregnancy and breast feeding
Lithium is a teratogen, causing birth defects in a small number of newborn babies.[40] Case reports and several retrospective studies have demonstrated possible increases in the rate of a congenital heart defect known as Ebstein's anomaly, if taken during a woman's pregnancy.[41] As a consequence, fetal echocardiography is routinely performed in pregnant women taking lithium to exclude the possibility of cardiac anomalies. Lamotrigine seems to be a possible alternative to lithium in pregnant women.[41] Gabapentin[42] and clonazepam[43] are also indicated as antipanic medications during the childbearing years and during pregnancy. Valproic acid and carbamazepine also tend to be associated with teratogenicity.
While it appears to be safe to use while breastfeeding a number of guidelines list it as a contraindication[3] including the British National Formulary.[44]
Dehydration
Dehydration in people taking lithium salts can be very hazardous, especially when combined with lithium-induced nephrogenic diabetes insipidus with polyuria. Such situations include preoperative fluid restrictions, warm weather conditions, sporting events, hiking, or other periods of fluid inaccessibility. Dehydration can result in increased plasma lithium levels due to decreased glomerular filtration rate, which causes lithium retention. Further, in the case of diabetes insipidus, free water is lost in greater proportion to sodium and other electrolytes, artificially raising lithium's concentration in the blood.
Another danger is that if the period of dehydration and diuresis has been prolonged, total body stores of sodium may actually be depleted, despite elevated plasma levels. Thus, rapid hydration with a large volume of plain water may very quickly produce hyponatremia, as total stores of sodium may be insufficient to support normal concentrations at a normal blood volume. Rapid overcorrection of hyponatremia also increases the risk of developing cerebral edema. Hyponatremia can also promote lithium retention by increasing reabsorption in the distal nephron, thus increasing lithium levels.[45]
Kidney damage
Lithium has been associated with several forms of kidney injury.[28][46][47][48] It is estimated that impaired urinary concentrating ability is present in at least 50% of individuals on chronic lithium therapy - lithium-induced nephrogenic diabetes insipidus[48] Continued use of lithium can lead to more serious kidney damage,[49][50] [51] aggravated form of diabetes insipidus.[52][53][54] and chronic kidney failure. CKD found in about one third of people undergoing long-term lithium treatment, according to one study.[29] Some forms of lithium-caused kidney damage may be progressive and lead to end-stage kidney failure.[55]
Interactions
Lithium concentrations are known to be increased with concurrent use of diuretics — especially loop diuretics (such as furosemide) and thiazides — and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.[22] Lithium concentrations can also be increased with concurrent use of ACE inhibitors such as captopril, enalapril, and lisinopril.[56]
Lithium is mainly removed from the body through glomerular function, but some is then reabsorbed together with sodium through the proximal tubule. Its levels are therefore sensitive to water and electrolyte balance.[57] Diuretics act by lowering water and sodium levels; this causes more reabsorption of lithium in the proximal tubules so that the removal of lithium from the body is less, leading to increased levels of lithium.[57][58] ACE inhibitors have also been shown in a retrospective case-control study to increase lithium concentrations. This is likely due to constriction of the afferent arteriole of the glomerulus, resulting in decreased glomerular filtration rate and clearance. Another possible mechanism is that ACE inhibitors can lead to a decrease in sodium and water. This will increase lithium reabsorption and its concentrations in the body.[57]
There are also drugs that can increase the clearance of lithium from the body, which can result in decreased lithium levels in the blood. These drugs include theophylline, caffeine, and acetazolamide. Additionally, increasing dietary sodium intake may also reduce lithium levels by prompting the kidneys to excrete more lithium.[59]
Lithium is also known to be a potential precipitant of serotonin syndrome in people concurrently on serotonergic medications such as antidepressants, buspirone and certain opioids such as pethidine (meperidine), tramadol, oxycodone, fentanyl and others.[22][60] Lithium co-treatment is also a risk factor for neuroleptic malignant syndrome in people on antipsychotics and other antidopaminergic medications.[61]
High doses of haloperidol, fluphenazine, or flupenthixol may be hazardous when used with lithium; irreversible toxic encephalopathy has been reported.[62] Indeed these and other antipsychotics have been associated with increased risk of lithium neurotoxicity, even with low therapeutic lithium doses. [63] [64]
Overdose
Lithium toxicity may occur on an acute basis, in persons taking excessive amounts either accidentally or intentionally, or on a chronic basis, in people who accumulate high levels during ongoing therapy. The manifestations include nausea, emesis, diarrhea, asthenia, ataxia, confusion, lethargy, polyuria, seizures and coma. Other toxic effects of lithium include coarse tremor, muscle twitching, convulsions and renal failure.[65] People who survive a poisoning episode may develop persistent neurotoxicity. Several authors have described a "Syndrome of Irreversible Lithium-Effected Neurotoxicity" (SILENT), associated with episodes of acute lithium toxicity or long-term treatment within the appropriate dosage range. Symptoms are said to include cerebellar dysfunction.[66]
Overdosage, usually with plasma concentrations over 1.5 mmol Li+
/l, may be fatal, and toxic effects include tremor, ataxia, dysarthria, nystagmus, renal impairment, confusion, and convulsions. If these potentially hazardous signs occur, treatment should be stopped, plasma lithium concentrations redetermined, and steps taken to reverse lithium toxicity.
Lithium toxicity is compounded by sodium depletion. Concurrent use of diuretics that inhibit the uptake of sodium by the distal tubule (e.g. thiazides) is hazardous and should be avoided because this can cause increased resorption of lithium in the proximal convoluted tubule, leading to elevated, potentially toxic levels. In mild cases, withdrawal of lithium and administration of generous amounts of sodium and fluid will reverse the toxicity. Plasma concentrations in excess of 2.5 mmol Li+
/l are usually associated with serious toxicity requiring emergency treatment. When toxic concentrations are reached, there may be a delay of one or two days before maximum toxicity occurs.
In long-term use, therapeutic concentrations of lithium have been thought to cause histological and functional changes in the kidney. The significance of such changes is not clear, but is of sufficient concern to discourage long-term use of lithium unless it is definitely indicated. Doctors may change a bipolar patient's medication from lithium to another mood-stabilizing drug, such as valproate (Depakote), if problems with the kidneys arise. An important potential consequence of long-term lithium use is the development of renal diabetes insipidus (inability to concentrate urine). Patients should therefore be maintained on lithium treatment after three to five years only if, on assessment, benefit persists. Conventional and sustained-release tablets are available. Preparations vary widely in bioavailability, and a change in the formulation used requires the same precautions as initiation of treatment. There are few reasons to prefer any one simple salt of lithium; the carbonate has been the more widely used, but the citrate is also available.
Mechanism of action
The specific biochemical mechanism of lithium action in stabilizing mood is unknown.[1]
Upon ingestion, lithium becomes widely distributed in the central nervous system and interacts with a number of neurotransmitters and receptors, decreasing norepinephrine release and increasing serotonin synthesis.[67]
Unlike many other psychoactive drugs, Li+
typically produces no obvious psychotropic effects (such as euphoria) in normal individuals at therapeutic concentrations.[67]
Lithium may also increase the release of serotonin by neurons in the brain.[68] In vitro studies performed on serotonergic neurons from rat raphe nuclei have shown that when these neurons are treated with lithium, serotonin release is enhanced during a depolarization compared to no lithium treatment and the same depolarization.[69]
Several authors proposed that pAp-phosphatase could be one of the therapeutic targets of lithium.[70][71] This hypothesis was supported by the low Ki of lithium for human pAp-phosphatase compatible within the range of therapeutic concentrations of lithium in the plasma of people (0.8–1 mM). Importantly, the Ki of human pAp-phosphatase is ten times lower than that of GSK3β (glycogen synthase kinase 3β). Inhibition of pAp-phosphatase by lithium leads to increased levels of pAp (3′-5′ phosphoadenosine phosphate), which was shown to inhibit PARP-1[72]
Another mechanism proposed in 2007 is that lithium may interact with nitric oxide (NO) signalling pathway in the central nervous system, which plays a crucial role in the neural plasticity. The NO system could be involved in the antidepressant effect of lithium in the Porsolt forced swimming test in mice.[73][74] It was also reported that NMDA receptor blockage augments antidepressant-like effects of lithium in the mouse forced swimming test,[75] indicating the possible involvement of NMDA receptor/NO signaling in the action of lithium in this animal model of learned helplessness.
Lithium possesses neuroprotective properties by preventing apoptosis and increasing cell longevity.[76]
Oxidative metabolism
Evidence suggests that mitochondrial dysfunction is present in patients with bipolar disorder.[76] Oxidative stress and reduced levels of anti-oxidants (such as glutathione) lead to cell death. Lithium may protect against oxidative stress by up-regulating complex I and II of the mitochondrial electron transport chain.[76]
Dopamine and G-protein coupling
During mania, there is an increase in neurotransmission of dopamine that causes a secondary homeostatic down-regulation, resulting in decreased neurotransmission of dopamine, which can cause depression.[76] Additionally, the post-synaptic actions of dopamine are mediated through G-protein coupled receptors. Once dopamine is coupled to the G-protein receptors, it stimulates other secondary messenger systems that modulate neurotransmission. Studies found that in autopsies (which do not necessarily reflect living people), people with bipolar disorder had increased G-protein coupling compared to people without bipolar disorder.[76] Lithium treatment alters the function of certain subunits of the dopamine associated G-protein, which may be part of its mechanism of action.[76]
Glutamate and NMDA receptors
Glutamate levels are observed to be elevated during mania. Lithium is thought to provide long-term mood stabilization and have anti-manic properties by modulating glutamate levels.[76] It is proposed that lithium competes with magnesium for binding to NMDA glutamate receptor, increasing the availability of glutamate in post-synaptic neurons.[76] The NMDA receptor is also affected by other neurotransmitters such as serotonin and dopamine. Effects observed appear exclusive to lithium and have not been observed by other monovalent ions such as rubidium and caesium.[76]
GABA receptors
GABA is an inhibitory neurotransmitter that plays an important role in regulating dopamine and glutamate neurotransmission.[76] It was found that patients with bipolar disorder had lower GABA levels, which results in excitotoxicity and can cause apoptosis (cell loss). Lithium counteracts these degrading processes by decreasing pro-apoptotic proteins and stimulating release of neuroprotective proteins.[76]
Cyclic AMP secondary messengers
The cyclic AMP secondary messenger system is shown to be modulated by lithium. Lithium was found to increase the basal levels of cyclic AMP but impair receptor coupled stimulation of cyclic AMP production.[76] It is hypothesized that the dual effects of lithium are due the inhibition of G-proteins that then mediate cyclic AMP production.[76] Over a long period of lithium treatment, cyclic AMP and adenylate cyclase levels are further changed by gene transcription factors.[76]
Inositol depletion hypothesis
Lithium treatment has been found to inhibit the enzyme inositol monophosphatase, involved in degrading inositol monophosphate to inositol required in PIP2 synthesis. This leads to lower levels of inositol triphosphate, created by decomposition of PIP2.[77] This effect has been suggested to be further enhanced with an inositol triphosphate reuptake inhibitor. Inositol disruptions have been linked to memory impairment and depression. It is known with good certainty that signals from the receptors coupled to the phosphoinositide signal transduction is effected by lithium.[78] myo-inositol is also regulated by the high affinity sodium mI transport system (SMIT). Lithium is hypothesized to inhibit mI entering the cells and mitigating the function of SMIT.[76] Reductions of cellular levels of myo-inositol results in the inhibition of the phosphoinositide cycle[76]
Intracellular calcium
In 2014, it was proposed that lithium treatment works by affecting calcium signaling by blocking excitotoxic processes[76] such as antagonizing NMDA receptors and inhibiting inositol monophosphatase (IMPase).[79]
History
Lithium was first used in the 19th century as a treatment for gout after scientists discovered that, at least in the laboratory, lithium could dissolve uric acid crystals isolated from the kidneys. The levels of lithium needed to dissolve urate in the body, however, were toxic.[80] Because of prevalent theories linking excess uric acid to a range of disorders, including depressive and manic disorders, Carl Lange in Denmark[81] and William Alexander Hammond in New York City[82] used lithium to treat mania from the 1870s onwards. By the turn of the 20th century, as theory regarding mood disorders evolved and so-called "brain gout" disappeared as a medical entity, the use of lithium in psychiatry was largely abandoned. Some suggest that the pharmaceutical industry was reluctant to invest in a drug that could not be patented,[83] however a number of lithium preparations were yet produced for the control of renal calculi and ‘‘uric acid diathesis’’.[84] As accumulating knowledge indicated a role for excess sodium intake in hypertension and heart disease, lithium salts were prescribed to patients for use as a replacement for dietary table salt (sodium chloride). This practice and the sale of lithium itself were both banned in 1949, following publication of reports detailing side effects and deaths.[80]
Also in 1949, the Australian psychiatrist John Cade rediscovered the usefulness of lithium salts in treating mania. Cade was injecting rodents with urine extracts taken from schizophrenic patients in an attempt to isolate a metabolic compound which might be causing mental symptoms. Since uric acid in gout was known to be psychoactive, (adenosine receptors on neurons are stimulated by it; caffeine blocks them), Cade needed soluble urate for a control. He used lithium urate, already known to be the most soluble urate compound, and observed that it caused the rodents to become tranquil. Cade traced the effect to the lithium ion itself, and so proposed lithium salts as tranquilizers. He soon succeeded in controlling mania in chronically hospitalized patients with them. This was one of the first successful applications of a drug to treat mental illness, and it opened the door for the development of medicines for other mental problems in the next decades.[85]
The rest of the world was slow to adopt this treatment, largely because of deaths which resulted from even relatively minor overdosing, including those reported from use of lithium chloride as a substitute for table salt. Largely through the research and other efforts of Denmark's Mogens Schou and Paul Baastrup in Europe,[80] and Samuel Gershon and Baron Shopsin in the U.S., this resistance was slowly overcome. The application of lithium in manic illness was approved by the United States Food and Drug Administration in 1970.[86] In 1974, this application was extended to its use as a preventive agent for manic-depressive illness.
Ronald R. Fieve, who had opened the first lithium clinic in North America in 1966, helped popularize the psychiatric use of lithium through his national TV appearances and his bestselling book, Moodswing. In addition, Fieve and David L. Dunner developed the concept of 'rapid cycling' Bipolar Disorder based on non-response to lithium.
Lithium has now become a part of Western popular culture. Characters in Pi, Premonition, Stardust Memories, American Psycho, Garden State, and An Unmarried Woman all take lithium. Sirius XM Satellite Radio in North America has a 1990s alternative rock station called Lithium, and several songs refer to the use of lithium as a mood stabilizer. These include: "Equilibrium met Lithium" by South African artist Koos Kombuis, "Lithium" by Evanescence, "Lithium" by Nirvana, "Lithium and a Lover" by Sirenia, "Lithium Sunset", from the album Mercury Falling by Sting,[87] and "Lithium" by Thin White Rope.
7 Up
As with cocaine in Coca-Cola, lithium was widely marketed as one of a number of patent medicine products popular in the late-19th and early-20th centuries, and was the medicinal ingredient of a refreshment beverage. Charles Leiper Grigg, who launched his St. Louis-based company The Howdy Corporation, invented a formula for a lemon-lime soft drink in 1920. The product, originally named "Bib-Label Lithiated Lemon-Lime Soda", was launched two weeks before the Wall Street Crash of 1929.[88] It contained the mood stabilizer lithium citrate, and was one of a number of patent medicine products popular in the late-19th and early-20th centuries.[89] Its name was soon changed to 7 Up. All American beverage makers were forced to remove lithium in 1948. Despite the 1948 ban, in 1950 the Painesville Telegraph still carried an advertisement for a lithiated lemon beverage.[90]
Names
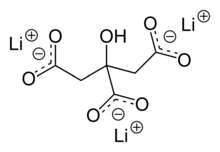
Lithium carbonate (Li
2CO
3), sold under several trade names, is the most commonly prescribed, while lithium citrate (Li
3C
6H
5O
7) is also used in conventional pharmacological treatments. Lithium orotate (C
5H
3LiN
2O
4), has been presented as an alternative.[91] Lithium bromide and lithium chloride have been used in the past as table salt; however, they fell out of use in the 1940s, when it was discovered they were toxic in those large doses. Many other lithium salts and compounds exist, such as lithium fluoride and lithium iodide, but they are presumed to be toxic as well and have never been evaluated for pharmacological effects.
Brand names include Camcolit (UK), Eskalith (US), Li-Liquid (UK), Liskonum (UK), Lithicarb (Australia), Lithobid (US), Priadel (UK), Quilonum (Australia), and Lithosun (India).
Research
Lithium may protect the brain and encourage the growth of gray matter in the cerebral cortex and prevent and slow the progression of Alzheimer's disease, senile dementia and Parkinson's disease.[92]
However, for the amyotrophic lateral sclerosis (ALS), lithium has failed to produce positive results.[93]
See also
References
- 1 2 3 4 5 6 7 8 9 10 "Lithium Salts". The American Society of Health-System Pharmacists. Retrieved Dec 1, 2015.
- ↑ Baldessarini, Ross J; Tondo, Leonardo; Davis, Paula; Pompili, Maurizio; Goodwin, Frederick K; Hennen, John (2006). "Decreased risk of suicides and attempts during long-term lithium treatment: A meta-analytic review". Bipolar Disorders. 8 (5p2): 625–39. doi:10.1111/j.1399-5618.2006.00344.x. PMID 17042835.
- 1 2 "Lithium use while Breastfeeding". LactMed. 2015-03-10. Retrieved 1 December 2015.
- ↑ Sneader, Walter (2005). Drug discovery : a history (Rev. and updated ed.). Chichester: Wiley. p. 63. ISBN 9780471899792.
- ↑ "WHO Model List of Essential Medicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ "Lithium Carbonate". International Drug Price Indicator Guide. Retrieved 1 December 2015.
- ↑ Cipriani, A.; Hawton, K.; Stockton, S.; Geddes, JR. (2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis.". BMJ. 346: f3646. doi:10.1136/bmj.f3646. PMID 23814104.
- ↑ Müller-Oerlinghausen, B; Berghöfer, A; Ahrens, B (2003). "The Antisuicidal and Mortality-Reducing Effect of Lithium Prophylaxis: Consequences for Guidelines in Clinical Psychiatry". Canadian Journal of Psychiatry. 48 (7): 433–9. PMID 12971012.
- ↑ Kovacsics, Colleen E.; Gottesman, Irving I.; Gould, Todd D. (2009). "Lithium's Antisuicidal Efficacy: Elucidation of Neurobiological Targets Using Endophenotype Strategies". Annual Review of Pharmacology and Toxicology. 49: 175–198. doi:10.1146/annurev.pharmtox.011008.145557. PMID 18834309.
- ↑ Semple, David "Oxford Hand Book of Psychiatry" Oxford Press. 2005.
- ↑ Rosenberg, J.; Salzman, C. (2007). "Update: New uses for lithium and anticonvulsants". CNS spectrums. 12 (11): 831–841. PMID 17984856.
- ↑ Frye, M. A.; Salloum, I. M. (2006). "Bipolar disorder and comorbid alcoholism: Prevalence rate and treatment considerations". Bipolar Disorders. 8 (6): 677–685. doi:10.1111/j.1399-5618.2006.00370.x. PMID 17156154.
- ↑ Vornik, L.; Brown, E. (2006). "Management of comorbid bipolar disorder and substance abuse". The Journal of Clinical Psychiatry. 67 Suppl 7: 24–30. PMID 16961421.
- ↑ Ohgami, H; Terao, T; Shiotsuki, I; Ishii, N; Iwata, N (2009). "Lithium levels in drinking water and risk of suicide". The British Journal of Psychiatry. 194 (5): 464–5; discussion 446. doi:10.1192/bjp.bp.108.055798. PMID 19407280.
- ↑ Gonzalez, R; Bernstein, I; Suppes, T (2008). "An investigation of water lithium concentrations and rates of violent acts in 11 Texas counties: Can an association be easily shown?". The Journal of Clinical Psychiatry. 69 (2): 325–6. doi:10.4088/jcp.v69n0221a. PMID 18363457.
- ↑ Kapusta, ND; Mossaheb, N; Etzersdorfer, E; Hlavin, G; Thau, K; Willeit, M; Praschak-Rieder, N; Sonneck, G; Leithner-Dziubas, K (2011). "Lithium in drinking water and suicide mortality". The British Journal of Psychiatry. 198 (5): 346–350. doi:10.1192/bjp.bp.110.091041. PMID 21525518.
- ↑ Healy D. 2005. Psychiatric Drugs Explained. 4th ed. Churchhill Livingstone: London.
- ↑ Amdisen A. (1978). "Clinical and serum level monitoring in lithium therapy and lithium intoxication". J. Anal. Toxicol. 2: 193–202. doi:10.1093/jat/2.5.193.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 851–854.
- ↑ The UK Electronic Medical Compendium recommends 0.4–0.8 mmol/l plasma lithium level in adults for prophylaxis of recurrent affective bipolar manic-depressive illness Camcolit 250 mg Lithium Carbonate Revision 2 December 2010, Retrieved 5 May 2011
- ↑ One study (Solomon, D.; Ristow, W.; Keller, M.; Kane, J.; Gelenberg, A.; Rosenbaum, J.; Warshaw, M. (1996). "Serum lithium levels and psychosocial function in patients with bipolar I disorder". The American Journal of Psychiatry. 153 (10): 1301–1307. PMID 8831438.) concluded a "low" dose of 0.4–0.6 mmol/L serum lithium treatment for patients with bipolar 1 disorder had less side effects, but a higher rate of relapse, than a "standard" dose of 0.8–1.0 mmol/l. However, a reanalysis of the same experimental data (Perlis, R.; Sachs, G.; Lafer, B.; Otto, M.; Faraone, S.; Kane, J.; Rosenbaum, J. (2002). "Effect of abrupt change from standard to low serum levels of lithium: A reanalysis of double-blind lithium maintenance data". The American Journal of Psychiatry. 159 (7): 1155–1159. doi:10.1176/appi.ajp.159.7.1155. PMID 12091193.) concluded the higher rate of relapse for the "low" dose was due to abrupt changes in the lithium serum levels
- 1 2 3 Truven Health Analytics, Inc. DrugPoint® System (Internet) [cited 7 October 2013]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- ↑ Australian Medicines Handbook. Adelaide: Australian Medicines Handbook Pty Ltd. 2013. ISBN 9780980579086.
- ↑ Joint Formulary Committee (2013). British National Formulary (BNF) 65. London: Pharmaceutical Press. pp. 240–242. ISBN 9780857110848.
- ↑ "lithium (Rx) - Eskalith, Lithobid". Medscape. WebMD. Retrieved 7 October 2013.
- ↑ "LITHOBID (lithium carbonate) tablet, film coated, extended release [NOVEN THERAPEUTICS, LLC]". DailyMed. National Library of Medicine. Retrieved 7 October 2013.
- ↑ "PRODUCT INFORMATION LITHICARB Lithium carbonate". TGA eBusiness Services. Aspen Pharmacare Australia Pty Ltd. Retrieved 7 October 2013.
- 1 2 Bedford, JJ; Weggery, S; Ellis, G; McDonald, FJ; Joyce, PR; Leader, JP; Walker, RJ (Sep 2008). "Lithium-induced Nephrogenic Diabetes Insipidus: Renal Effects of Amiloride". Clin J Am Soc Nephrol. 3: 1324–1331. doi:10.2215/CJN.01640408.
- 1 2 Aiff, H; Attman, P-O; Aurel, M; Bendz, H; Ramsauer, B; Schon, S; Svedlund, J (May 2015). "Effects of 10 to 30 years of lithium treatment on kidney function". J Psychopharmacol. 29: 608–614. doi:10.1177/0269881115573808.
- 1 2 Safe and effective use of lithium Australian Prescriber
- ↑ Sperner-Unterweger, Barbara; W. Wolfgang Fleischhacker; Wolfgang P. Kaschka (2001). Psychoneuroimmunology. Karger Publishers. p. 22. ISBN 3-8055-7262-X.
- ↑ Silver, M; Factor, S (2015). "Chapter 12: VPA, lithium, amiodarone, and other non-DA". In Friedman, J. Medication-Induced Movement Disorders. Cambridge University Press. pp. 131–140. ISBN 978-1-107-06600-7.
- ↑ "Effect of lithium on hypothalamic-pituitary-thyroid function in patients with affective disorders.". Br Med J. 3: 623–6. 1975. doi:10.1136/bmj.3.5984.623. PMC 1674449
 . PMID 809083.
. PMID 809083. - ↑ Wetzels, JF; Van Bergeijk, JD; Hoitsma, AJ; Huysmans, FT; Koene, RA (1989). "Triamterene increases lithium excretion in healthy subjects: Evidence for lithium transport in the cortical collecting tubule". Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 4 (11): 939–42. PMID 2516883.
- ↑ Keshavan, Matcheri S.; John S. Kennedy (2001). Drug-induced dysfunction in psychiatry. Taylor & Francis. p. 305. ISBN 0-89116-961-X.
- ↑ Side Effects – Lithium / Various Brand Names – Bipolar Disorder Medications
- ↑ Nutrition Articles – The Relationship between Weight Gain and Medications for Depression and Seizures
- ↑ Safer lithium therapy. NHS National Patient Safety Agency. Issue date: 1 December 2009
- ↑ Bendz, Hans; Schön, Staffan; Attman, Per-Ola; Aurell, Mattias (1 February 2010). "Renal failure occurs in chronic lithium treatment but is uncommon". Kidney International. 77 (3): 219–24. doi:10.1038/ki.2009.433. PMID 19940841.
- ↑ Shepard, TH.; Brent, RL.; Friedman, JM.; Jones, KL.; Miller, RK.; Moore, CA.; Polifka, JE. (2002). "Update on new developments in the study of human teratogens". Teratology. 65 (4): 153–61. doi:10.1002/tera.10032. PMID 11948561.
- 1 2 Yacobi, S; Ornoy, A (2008). "Is lithium a real teratogen? What can we conclude from the prospective versus retrospective studies? A review". The Israel Journal of Psychiatry and Related Sciences. 45 (2): 95–106. PMID 18982835.
- ↑ Montouris, G (2003). "Gabapentin exposure in human pregnancy: Results from the Gabapentin Pregnancy Registry". Epilepsy & behavior : E&B. 4 (3): 310–7. doi:10.1016/S1525-5050(03)00110-0. PMID 12791334.
- ↑ Weinstock, L; Cohen, LS; Bailey, JW; Blatman, R; Rosenbaum, JF (2001). "Obstetrical and neonatal outcome following clonazepam use during pregnancy: A case series". Psychotherapy and psychosomatics. 70 (3): 158–62. doi:10.1159/000056242. PMID 11340418.
- ↑ https://www.evidence.nhs.uk/formulary/bnf/current/4-central-nervous-system/42-drugs-used-in-psychoses-and-related-disorders/423-drugs-used-for-mania-and-hypomania/lithium/lithium-carbonate
- ↑ Thomsen, Klaus; Shirley, David G. (2006-04-01). "A hypothesis linking sodium and lithium reabsorption in the distal nephron". Nephrology Dialysis Transplantation. 21 (4): 869–880. doi:10.1093/ndt/gfk029. ISSN 0931-0509. PMID 16410274.
- ↑ Gitlin, M (Mar 1999). "Lithium and the kidney: an updated review.". Drug Saf. 20: 231–243. PMID 10221853.
- ↑ Nielsen, J; Kwon, TH; Christensen, BM; Frokiaer, J; Nielsen, S (May 2008). "Dysregulation of renal aquaporins and epithelial sodium channel in lithium-induced nephrogenic diabetes insipidus". Semin. Nephrol. 28: 227–244. doi:10.1016/j.semnephrol.2008.03.002.
- 1 2 Alexander, MP; Farag, YM; Mittal, BV; Rennke, HG; Singh, AK (Jan 2008). "Lithium toxicity: a double-edged sword". Kidney Int. 73: 233–237. doi:10.1038/sj.ki.5002578.
- ↑ Boton, R; Gaviria, M; Battlle, DC (Nov 1987). "Prevalence, pathogenesis, and treatment of renal dysfunction associated with chronic lithium therapy". Am J Kidney Dis. 10: 329–345. PMID 3314489.
- ↑ Timmer, RT; Sands, JM (Mar 1999). "Lithium intoxication". J Am Soc Nephrol. 10: 666–674. PMID 10073618.
- ↑ Sands, JM; Bichet, DG (Feb 2006). "Nephrogenic diabetes insipidus". Ann Intern Med. 144: 186–194. PMID 16461963.
- ↑ Thompson, CJ; France, AJ; Baylis, PH (Feb 1997). "Persistent nephrogenic diabetes insipidus following lithium therapy". Scott Med J. 42: 16–17. PMID 9226773.
- ↑ Stone, KA (Jan 1999). "Lithium-induced nephrogenic diabetes insipidus". J Am Board Fam Pract. 12: 43–47. PMID 10050642.
- ↑ Garofeanu, CG; Weir, M; Rosas-Arellano, MP; Garg, AX; Clark, WF (Apr 2005). "Causes of reversible nephrogenic diabetes insipidus: a systematic review". Am J Kidney Dis. 45: 626–637. PMID 15806465.
- ↑ Presne, C; Fakhouri, F; Noel, L-H; Stengel, B; Even, C; Kreis, H; Mignon, F; Grunfeld, J-P (Aug 2003). "Lithium-induced nephropathy: Rate of progression and prognostic factors". Kidney Int. 64: 585–592. doi:10.1046/j.1523-1755.2003.00096.x.
- ↑ "Lithium". WebMD. Retrieved 1 November 2014.
- 1 2 3 Finley, PR (February 1996). "Lithium and angiotensin-converting enzyme inhibitors: evaluation of a potential interaction". J Clin Psychopharmacol. 16 (1): 68–71. doi:10.1097/00004714-199602000-00011. PMID 8834421.
- ↑ Oruch, R (October 5, 2014). "Lithium: a review of pharmacology, clinical uses, and toxicity". Eur J Pharmacol. 740 (740): 464–73. doi:10.1016/j.ejphar.2014.06.042. PMID 24991789.
- ↑ al.], edited by Brian K. Alldredge ... [et (2013). Applied therapeutics : the clinical use of drugs. (10th ed.). Baltimore: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1991. ISBN 978-1609137137.
- ↑ Boyer, EW. "Serotonin syndrome". UpToDate. Wolters Kluwer. Retrieved 8 October 2013.
- ↑ Wijdicks, EFM. "Neuroleptic malignant syndrome". UpToDate. Wolters Kluwer. Retrieved 8 October 2013.
- ↑ Case reports: (Sandyk, R.; Hurwitz, M. D. (1983). "Toxic irreversible encephalopathy induced by lithium carbonate and haloperidol. A report of 2 cases". South African medical journal. 64 (22): 875–876. PMID 6415823.)(Gille, M.; Ghariani, S.; Piéret, F.; Delbecq, J.; Depré, A.; Saussu, F.; De Barsy, T. (1997). "Acute encephalomyopathy and persistent cerebellar syndrome after lithium salt and haloperidol poisoning". Revue neurologique. 153 (4): 268–270. PMID 9296146.)
- ↑ Emilien, G; Maloteaux, J (1996). "Lithium neurotoxicity at low therapeutic doses". Acta Neurol Belg. 96: 281–293. PMID 9008777.
- ↑ Netto, I; Phutane, V (2012). "Reversible lithium neurotoxicity: review of the literature". Prim Care Companion CNS Disord. 14 (1). doi:10.4088/PCC.11r01197.
- ↑ Gelder, M., Mayou, R. and Geddes, J. 2005. Psychiatry. 3rd ed. New York: Oxford. pp249.
- ↑ Adityanjee; Munshi, Thampy (2005). "The syndrome of irreversible lithium-effectuated neurotoxicity.". Clinical Neuropharmacology. 28 (1): 38–49. doi:10.1097/01.wnf.0000150871.52253.b7. PMID 15714160.
- 1 2 Brunton, L; Chabner, B; Knollman, B (2010). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill Professional. ISBN 978-0-07-162442-8.
- ↑ Massot, O.; Rousselle, J. C.; Fillion, M. P.; Januel, D.; Plantefol, M.; Fillion, G. (1999). "5-HT1B Receptors: A Novel Target for Lithium Possible Involvement in Mood Disorders". Neuropsychopharmacology. 21 (4): 530–541. doi:10.1016/S0893-133X(99)00042-1. PMID 10481837.
- ↑ Scheuch, K.; Höltje, M.; Budde, H.; Lautenschlager, M.; Heinz, A.; Ahnert-Hilger, G.; Priller, J. (2010). "Lithium modulates tryptophan hydroxylase 2 gene expression and serotonin release in primary cultures of serotonergic raphe neurons". Brain Research. 1307: 14–21. doi:10.1016/j.brainres.2009.10.027. PMID 19840776.
- ↑ York JD, et al. (1995). "Definition of a metal-dependent/Li+-inhibited phosphomonoesterase protein family based upon a conserved three-dimensional core structure". Proc. Natl. Acad. Sci. U.S.A. 92: 5149–5153. doi:10.1073/pnas.92.11.5149. PMC 41866
 . PMID 7761465.
. PMID 7761465. - ↑ Yenush (2000). "A novel target of lithium therapy". FEBS Lett. 467: 321–325. doi:10.1016/s0014-5793(00)01183-2.
- ↑ Toledano E, et al. (2012). "3'-5' phosphoadenosine phosphate is an inhibitor of PARP-1 and a potential mediator of the lithium-dependent inhibition of PARP-1 in vivo". Biochem J. 443 (2): 485–90. doi:10.1042/BJ20111057. PMID 22240080.
- ↑ Ghasemi M, Sadeghipour H, Mosleh A, Sadeghipour HR, Mani AR, Dehpour AR; Sadeghipour; Mosleh; Sadeghipour; Mani; Dehpour (May 2008). "Nitric oxide involvement in the antidepressant-like effects of acute lithium administration in the mouse forced swimming test". Eur Neuropsychopharmacol. 18 (5): 323–32. doi:10.1016/j.euroneuro.2007.07.011. PMID 17728109.
- ↑ Ghasemi M, Sadeghipour H, Poorheidari G, Dehpour AR; Sadeghipour; Poorheidari; Dehpour (June 2009). "A role for nitrergic system in the antidepressant-like effects of chronic lithium treatment in the mouse forced swimming test". Behav. Brain Res. 200 (1): 76–82. doi:10.1016/j.bbr.2008.12.032. PMID 19166880.
- ↑ Ghasemi M, Raza M, Dehpour AR; Raza; Dehpour (April 2010). "NMDA receptor antagonists augment antidepressant-like effects of lithium in the mouse forced swimming test". J. Psychopharmacol. (Oxford). 24 (4): 585–94. doi:10.1177/0269881109104845. PMID 19351802.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Malhi GS (2013). "Potential mechanisms of action of lithium in bipolar disorder. Current understanding.". CNS Drugs. 27 (2): 135–53. doi:10.1007/s40263-013-0039-0. PMID 23371914.
- ↑ Einat H, Kofman O, Itkin O, Lewitan RJ, Belmaker RH; Kofman; Itkin; Lewitan; Belmaker (1998). "Augmentation of lithium's behavioral effect by inositol uptake inhibitors". J Neural Transm. 105 (1): 31–8. doi:10.1007/s007020050035. PMID 9588758.
- ↑ Jope RS (1999). "Anti-bipolar therapy: mechanism of action of lithium". Mol. Psychiatry. 4 (2): 117–128. doi:10.1038/sj.mp.4000494. PMID 10208444.
- ↑ Wallace, James (Mar 2014). "Calcium dysregulation, and lithium treatment to forestall Alzheimer's disease - a merging of hypotheses". Cell Calcium. 55 (3): 175–181. doi:10.1016/j.ceca.2014.02.005. PMID 24636273.
- 1 2 3 Marmol, F. (2008). "Lithium: Bipolar disorder and neurodegenerative diseases Possible cellular mechanisms of the therapeutic effects of lithium". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 32 (8): 1761–1771. doi:10.1016/j.pnpbp.2008.08.012. PMID 18789369.
- ↑ Lenox, RH; Watson, DG (1994). "Lithium and the brain: a psychopharmacological strategy to a molecular basis for manic depressive illness". Clinical Chemistry. 40 (2): 309–14. PMID 8313612.
- ↑ Mitchell, PB; Hadzi-Pavlovic, D (2000). "Lithium treatment for bipolar disorder" (PDF). Bulletin of the World Health Organization. 78 (4): 515–7. PMC 2560742
 . PMID 10885179.
. PMID 10885179. - ↑ Greenfield, Susan: "Brain Power: Working out the Human Mind", page 91. Element Books Limited, 1999
- ↑ Shorter E (2009). "The history of lithium therapy". Bipolar Disorders. 11: 4–9. doi:10.1111/j.1399-5618.2009.00706.x.
- ↑ Cade J. F. J. (1949). "Lithium salts in the treatment of psychotic excitement" (PDF). Medical Journal of Australia. 2 (10dfbnm): 349–52. PMID 18142718.
- ↑ P. B. Mitchell, D. Hadzi-Pavlovic; Hadzi-Pavlovic (2000). "Lithium treatment for bipolar disorder" (PDF). Bulletin of the World Health Organization. 78 (4): 515–7. PMC 2560742
 . PMID 10885179.
. PMID 10885179. - ↑ Agassi, Tirzah (1996-03-12). "Sting is now older, wiser and duller". The Jerusalem Post. Retrieved 2009-06-25.
- ↑ "7 UP: The Making of a Legend". Cadbury Schweppes: America's Beverages.
- ↑ "Urban Legends Reference Pages: 7Up". Retrieved 13 November 2007.
- ↑ anonymous (13 July 1950). "ISALLY'S (ad)". Painesville Telegraph. Retrieved 8 September 2013.
- ↑ Nieper HA (1973). "The clinical applications of lithium orotate. A two years study". Agressologie. 14 (6): 407–11. PMID 4607169.
- ↑ Forlenza, OV; de Paula, VJ; Machado-Vieira, R; Diniz, BS; Gattaz, WF (1 May 2012). "Does lithium prevent Alzheimer's disease?". Drugs & aging. 29 (5): 335–42. doi:10.2165/11599180-000000000-00000. PMID 22500970.
- ↑ Ludolph, AC; Brettschneider, J; Weishaupt, JH (October 2012). "Amyotrophic lateral sclerosis.". Current opinion in neurology. 25 (5): 530–5. doi:10.1097/WCO.0b013e328356d328. PMID 22918486.
External links
- Official FDA information published by Drugs.com
- "Exposing lithium's circadian action"
- http://www.psycheducation.org/depression/meds/moodstabilizers.htm
- http://www.psycheducation.org/depression/meds/lithium.html
- CID 11125 — PubChem Compound Summary (Lithium Carbonate)
- N05AN01 (WHO)
Further reading
- Mota de Freitas, Duarte; Leverson, Brian D.; Goossens, Jesse L. (2016). "Chapter 15. Lithium in Medicine: Mechanisms of Action". In Astrid, Sigel; Helmut, Sigel; Roland K.O., Sigel. The Alkali Metal Ions: Their Role in Life. Metal Ions in Life Sciences. 16. Springer. pp. 557–584. doi:10.1007/978-4-319-21756-7_15.