Phthalate
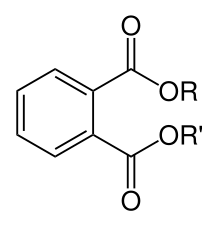
Phthalates (pronounced /ˈθæˌleɪts/[1] or in British English /ˈ(f)θaleɪts/[2]), or phthalate esters, are esters of phthalic acid and are mainly used as plasticizers (substances added to plastics to increase their flexibility, transparency, durability, and longevity). Phthalates are manufactured by reacting phthalic anhydride with alcohol(s) that range from methanol and ethanol (C1/C2) up to tridecyl alcohol (C13), either as a straight chain or with some branching. They are divided into two distinct groups, with very different applications, toxicological properties, and classification, based on the number of carbon atoms in their alcohol chain. They are used primarily to soften polyvinyl chloride (PVC). Lower-molecular-weight phthalates (3-6 carbon atoms in their backbone) are being gradually replaced in many products in the United States, Canada, and European Union over health concerns. They are replaced by high-molecular-weight phthalates (those with more than 6 carbons in their backbone, which gives them increased permanency and durability). In 2010, the market was still dominated by high-phthalate plasticizers; however, due to legal provisions and growing environmental awareness and perceptions, producers are increasingly forced to use non-phthalate plasticizers.[3]
Phthalates are used in a wide range of common products, and are released into the environment.[4] There is no covalent bond between the phthalates and plastics; rather, they are entangled within the plastic as a result of the manufacturing process used to make PVC articles.[5] They can be removed by exposure to heat or with organic solvents. Due to the ubiquity of plastics (and therefore plasticizers) in modern life, the vast majority of people are exposed to some level of phthalates, and most Americans tested by the Centers for Disease Control and Prevention have metabolites of multiple phthalates in their urine.[6] Phthalate exposure may be through direct use or by indirect means through leaching and general environmental contamination. Diet is believed to be the main source of di(2-ethylhexyl) phthalate (DEHP) and other phthalates in the general population.[6] Fatty foods such as milk, butter, and meats are a major source.[7] In studies of rodents exposed to certain phthalates, high doses have been shown to change hormone levels and cause birth defects.[8]
Uses
Phthalates are used in a large variety of products, from enteric coatings of pharmaceutical pills and nutritional supplements to viscosity control agents, gelling agents, film formers, stabilizers, dispersants, lubricants, binders, emulsifying agents, and suspending agents. End-applications include adhesives and glues, agricultural adjuvants, building materials, personal-care products, medical devices, detergents and surfactants, packaging, children's toys, modelling clay, waxes, paints, printing inks and coatings, pharmaceuticals, food products, and textiles. Phthalates are also frequently used in soft plastic fishing lures, caulk, paint pigments, and sex toys made of so-called "jelly rubber". Phthalates are used in a variety of household applications such as shower curtains, vinyl upholstery, adhesives, floor tiles, food containers and wrappers, and cleaning materials. Personal-care items containing phthalates include perfume, eye shadow, moisturizer, nail polish, liquid soap, and hair spray.[9]
Phthalates are also found in modern electronics and medical applications such as catheters and blood transfusion devices. The most widely used phthalates are di(2-ethylhexyl) phthalate (DEHP), diisodecyl phthalate (DIDP), and diisononyl phthalate (DINP). DEHP was the dominant plasticizer used globally in PVC due to its low cost. Benzylbutylphthalate (BBP) is used in the manufacture of foamed PVC, which is used mostly as a flooring material, though its use is decreasing rapidly in the Western countries. Phthalates with small R and R' groups are used as solvents in perfumes and pesticides.
Approximately 8.4 million tonnes of plasticizers are consumed globally every year, of which European consumption accounts for approximately 1.5 million metric tonnes.[10] Approximately 70% of those totals are phthalates, down from about 88% in 2005. The remaining 30% are alternative chemistries. Plasticizers contribute 10-60% of total weight of plasticized products. More recently in Europe and the US, regulatory developments have resulted in a change in phthalate consumption, with the higher phthalates (DINP and DIDP) replacing DEHP as the general purpose plasticizer of choice because DIDP and DINP were not classified as hazardous. All of these mentioned phthalates are now regulated and restricted in many products. DEHP, although most applications are shown to pose no risk when studied using recognized methods of risk assessment, has been classified as a Category 1A reprotoxin, and is now on the Annex XIV of the European Union's REACH legislation, which means that producers and users must submit authorization requests to the European Chemicals Agency in Helsinki in order to continue to use DEHP. Analysis of such applications will involve studies on alternatives and, given the wide number of compounds that have been used as plasticizers, such evaluations are likely to be far-reaching.
History
The development of cellulose nitrate plastic in 1846 led to the patent of castor oil in 1856 for use as the first plasticizer. In 1870, camphor became the more favored plasticizer for cellulose nitrate. Phthalates were first introduced in the 1920s and quickly replaced the volatile and odorous camphor. In 1931, the commercial availability of polyvinyl chloride and the development of di(2-ethylhexyl) phthalate began the boom of the plasticizer PVC industry.
Properties
Phthalate esters are the dialkyl or alkyl aryl esters of phthalic acid (also called 1,2-benzenedicarboxylic acid, not be confused with the structurally isomeric terephthalic or isophthalic acids ); the name "phthalate" derives from phthalic acid, which itself is derived from word "naphthalene". When added to plastics, phthalates allow the long polyvinyl molecules to slide against one another. The phthalates have a clear syrupy liquid consistency and show low water solubility, high oil solubility, and low volatility. The polar carboxyl group contributes little to the physical properties of the phthalates, except when R and R' are very small (such as ethyl or methyl groups). Phthalates are colorless, odorless liquids produced by reacting phthalic anhydride with an appropriate alcohol (usually 6- to 13-carbon).
The mechanism by which phthalates and other molecules afford plasticization to polar polymers has been a subject of intense study since the 1960s. The mechanism is one of polar interactions between the polar centres of the phthalate molecule (the C=O functionality) and the positively charged areas of the vinyl chain, typically residing on the carbon atom of the carbon-chlorine bond. In order for this to be established, the polymer must be heated in the presence of the plasticizer, first above the Tg of the polymer and then into a melt state. This enables an intimate mix of polymer and plasticizer to be formed, and for these interactions to occur. When cooled, these interactions remain and the network of PVC chains cannot reform (as is present in unplasticized PVC, or PVC-U). The alkyl chains of the phthalate then screen the PVC chains from each other as well.
Table of the most common phthalates
| Name | Abbreviation | Structural formula | Molecular weight (g/mol) | CAS No. |
|---|---|---|---|---|
| Dimethyl phthalate | DMP | C6H4(COOCH3)2 | 194.18 | 131-11-3 |
| Diethyl phthalate | DEP | C6H4(COOC2H5)2 | 222.24 | 84-66-2 |
| Diallyl phthalate | DAP | C6H4(COOCH2CH=CH2)2 | 246.26 | 131-17-9 |
| Di-n-propyl phthalate | DPP | C6H4[COO(CH2)2CH3]2 | 250.29 | 131-16-8 |
| Di-n-butyl phthalate | DBP | C6H4[COO(CH2)3CH3]2 | 278.34 | 84-74-2 |
| Diisobutyl phthalate | DIBP | C6H4[COOCH2CH(CH3)2]2 | 278.34 | 84-69-5 |
| Butyl cyclohexyl phthalate | BCP | CH3(CH2)3OOCC6H4COOC6H11 | 304.38 | 84-64-0 |
| Di-n-pentyl phthalate | DNPP | C6H4[COO(CH2)4CH3]2 | 306.40 | 131-18-0 |
| Dicyclohexyl phthalate | DCP | C6H4[COOC6H11]2 | 330.42 | 84-61-7 |
| Butyl benzyl phthalate | BBP | CH3(CH2)3OOCC6H4COOCH2C6H5 | 312.36 | 85-68-7 |
| Di-n-hexyl phthalate | DNHP | C6H4[COO(CH2)5CH3]2 | 334.45 | 84-75-3 |
| Diisohexyl phthalate | DIHxP | C6H4[COO(CH2)3CH(CH3)2]2 | 334.45 | 146-50-9 |
| Diisoheptyl phthalate | DIHpP | C6H4[COO(CH2)4CH(CH3)2]2 | 362.50 | 41451-28-9 |
| Butyl decyl phthalate | BDP | CH3(CH2)3OOCC6H4COO(CH2)9CH3 | 362.50 | 89-19-0 |
| Di(2-ethylhexyl) phthalate | DEHP, DOP | C6H4[COOCH2CH(C2H5)(CH2)3CH3]2 | 390.56 | 117-81-7 |
| Di(n-octyl) phthalate | DNOP | C6H4[COO(CH2)7CH3]2 | 390.56 | 117-84-0 |
| Diisooctyl phthalate | DIOP | C6H4[COO(CH2)5CH(CH3)2]2 | 390.56 | 27554-26-3 |
| n-Octyl n-decyl phthalate | ODP | CH3(CH2)7OOCC6H4COO(CH2)9CH3 | 418.61 | 119-07-3 |
| Diisononyl phthalate | DINP | C6H4[COO(CH2)6CH(CH3)2]2 | 418.61 | 28553-12-0 |
| Di(2-propylheptyl) phthalate | DPHP | C6H4[COOCH2CH(CH2CH2CH3)(CH2)4CH3]2 | 446.66 | 53306-54-0 |
| Diisodecyl phthalate | DIDP | C6H4[COO(CH2)7CH(CH3)2]2 | 446.66 | 26761-40-0 |
| Diundecyl phthalate | DUP | C6H4[COO(CH2)10CH3]2 | 474.72 | 3648-20-2 |
| Diisoundecyl phthalate | DIUP | C6H4[COO(CH2)8CH(CH3)2]2 | 474.72 | 85507-79-5 |
| Ditridecyl phthalate | DTDP | C6H4[COO(CH2)12CH3]2 | 530.82 | 119-06-2 |
| Diisotridecyl phthalate | DITP | C6H4[COO(CH2)10CH(CH3)2]2 | 530.82 | 68515-47-9 |
Health effects
Exposure
Phthalates are easily released into the environment.[4] In general, they do not persist in the outdoor environment due to biodegradation, photodegradation, and anaerobic degradation. Outdoor air concentrations are higher in urban and suburban areas than in rural and remote areas.[9]
In general, indoor air concentrations are higher than outdoor air concentrations due to the nature of the sources. Because of their volatility, DEP and DMP are present in higher concentrations in air in comparison with the heavier and less volatile DEHP. Higher air temperatures result in higher concentrations of phthalates in the air. PVC flooring leads to higher concentrations of BBP and DEHP, which are more prevalent in dust.[9][11] A 2012 Swedish study of children found that phthalates from PVC flooring were taken up into their bodies, showing that children can ingest phthalates not only from food but also by breathing and through the skin.[12]
People are commonly exposed to phthalates, and most people in the US tested by the Centers for Disease Control and Prevention have metabolites of multiple phthalates in their urine. Recent human biomonitoring data shows that the tolerable intake of children is exceeded to a considerable degree, in some instances up to 20-fold. Because phthalate plasticizers are not chemically bound to PVC, they can easily leach and evaporate into food or the atmosphere. Phthalate exposure can be through direct use or by indirect means through leaching and general environmental contamination.
Diet is believed to be the main source of DEHP and other phthalates in the general population. Fatty foods such as milk, butter, and meats are a major source. Studies show that exposure to phthalates is greater from ingestion of certain foods, rather than exposure via water bottles as is most often first thought of with plastic chemicals.[13] Low-molecular-weight phthalates such as DEP, DBP, BBzP may be dermally absorbed. Inhalational exposure is also significant with the more volatile phthalates.[14] Another study, conducted between 2003 and 2010 analysing data from 9,000 individuals, from those reported that had eaten at a fast food restaurant were found with much higher levels of two separate phthalates - DEHP and DiNP - in their urine samples. Interestingly, even small consumption of fast food caused higher presence of phthalates. 'People who reported eating only a little fast food had DEHP levels that were 15.5 percent higher and DiNP levels that were 25 percent higher than those who said they had eaten none. For people who reported eating a sizable amount, the increase was 24 percent and 39 percent, respectively.'
In a 2008 Bulgarian study, higher dust concentrations of DEHP were found in homes of children with asthma and allergies, compared with healthy children's homes.[15] The author of the study stated, "The concentration of DEHP was found to be significantly associated with wheezing in the last 12 months as reported by the parents."[15] Phthalates were found in almost every sampled home in Bulgaria. The same study found that DEHP, BBzP, and DnOP were in significantly higher concentrations in dust samples collected in homes where polishing agents were used. Data on flooring materials was collected, but there was not a significant difference in concentrations between homes where no polish was used that have balatum (PVC or linoleum) flooring and homes with wood. High frequency of dusting did decrease the concentration.[15]
In general, children's exposure to phthalates is greater than that of adults. In a 1990s Canadian study that modeled ambient exposures, it was estimated that daily exposure to DEHP was 9 μg/kg bodyweight/day in infants, 19 μg/kg bodyweight/day in toddlers, 14 μg/kg bodyweight/day in children, and 6 μg/kg bodyweight/day in adults.[14] Infants and toddlers are at the greatest risk of exposure, because of their mouthing behavior. Body-care products containing phthalates are a source of exposure for infants. The authors of a 2008 study "observed that reported use of infant lotion, infant powder, and infant shampoo were associated with increased infant urine concentrations of [phthalate metabolites], and this association is strongest in younger infants. These findings suggest that dermal exposures may contribute significantly to phthalate body burden in this population." Though they did not examine health outcomes, they noted that "Young infants are more vulnerable to the potential adverse effects of phthalates given their increased dosage per unit body surface area, metabolic capabilities, and developing endocrine and reproductive systems."[16]
Infants and hospitalized children are particularly susceptible to phthalate exposure. Medical devices and tubing may contain 20-40% Di(2-ethylhexyl) phthalate (DEHP) by weight, which "easily leach out of tubing when heated (as with warm saline/blood) ".[17] Several medical devices contain phthalates including, but not limited to, IV tubing, gloves, nasogastric tubes and respiratory tubing. The Food and Drug Administration did an extensive risk assessment of phthalates in the medical setting and found that neonates may be exposed to five times greater than the allowed daily tolerable intake. This finding led to the conclusion by the FDA that, "Children undergoing certain medical procedures may represent a population at increased risk for the effects of DEHP." [17]
In 2008, the Danish Environmental Protection Agency (EPA) found a variety of phthalates in erasers and warned of health risks when children regularly suck and chew on them. The European Commission Scientific Committee on Health and Environmental Risks (SCHER), however, considers that, even in the case when children bite off pieces from erasers and swallow them, it is unlikely that this exposure leads to health consequences.[18]
Phthalates are also found in medications, where they are used as inactive ingredients in producing enteric coatings. It is not known how many medications are made using phthalates, but some include omeprazole, didanosine, mesalamine, and theophylline. A recent study found that urinary concentrations of monobutyl phthalate, the DBP metabolite, of Asacol (a particular formulation of mesalamine) users was 50 times higher than the mean of nonusers.[19] The study showed that exposures from phthalate-containing medications can far exceed population levels from other sources.[19] DBP in medications raises concern about health risks due to the high level of exposures associated with taking these medications, especially in vulnerable segments of the population, including pregnant women and children.[19]
In 2008, the United States National Research Council recommended that the cumulative effects of phthalates and other antiandrogens be investigated. It criticized US EPA guidances, which stipulate that, when examining cumulative effects, the chemicals examined should have similar mechanisms of action or similar structures, as too restrictive. It recommended instead that the effects of chemicals that cause similar adverse outcomes should be examined cumulatively.[20]:9 Thus, the effect of phthalates should be examined together with other antiandrogens, which otherwise may have been excluded because their mechanisms or structure are different.
Breast cancer
Much of the current research on effects of phthalate exposure has been focused on children and men's health.[21] However, women may be at higher risk for potential adverse health effects of phthalates due to increased cosmetic use. Diethyl phthalate and dibutyl phthalate are especially ubiquitous in cosmetics and personal care products in some countries (NB: DBP is banned in cosmetics in the European Union under Directive 76/768/EEC 1976[22])[21] According to in vivo and observational studies by Davis et al. (1994) and Lopez-Carillo et al. (2010), there is an association between phthalate exposure and endocrine disruption leading to development of breast cancer. Furthermore, it has been well-documented that endocrine disruptors such as phthalates can be additive, so even very small amounts can interact with other chemicals to have cumulative, adverse "cocktail effects" [23]
Phthalate parent compounds and/or their metabolites have recently been implicated as a cause of breast cancer (BC).[21] A 2010 study published in Environmental Health Perspectives for the first time implicated that the exposure to diethyl phthalates (DEP), a parent compound of the monoethyl phthalate (MEP) metabolite, may be associated with increased risk of BC (Odds Ratio of 2.20, p value for trend, p<0.003).[21] The case-control study was age matched to 233 BC cases residing in northern Mexico. The phthalate level was determined in urine samples collected pretreatment from the cases. This is only a preliminary finding therefore additional research is required. It is interesting to note that exposure to the parent phthalate, butylbenzyl phthalate (BBzP) of the monobenzyl phthalate (MBzP) metabolite showed a negative association with breast cancer (Odds ratio=0.46, p value for trend, p<.008).[21] This finding may be associated with the demethylation of the estrogen receptor complex in breast cancer cells of this particular phthalate resulting in a negative effect.[21] This explanation will require further confirmatory research since confounders may be playing an unknown role. It is also known that DEP is found in a high proportion of personal care products, deodorants, and perfumes, whereas, in contrast, BBzP is not detected in most deodorants and hair products and in less than one-third of all products tested,[21] so degree of exposure may also be influencing results. A higher phthalate tertile (microgram/g creatinine) of DEP/MEP was compared to a lower phthalate tertile of BBzP/MBzP in this study. In most cases of breast cancer, the cause is unknown, and less than 25% of patients have a history of commonly associated risk factors.[21] such as: early menarche, later age at first childbirth, nulliparity, family history of BC, or history of benign breast biopsy [24]
Endocrine disruption
Several phthalates are "plausibly" endocrine disruptors.[25] In studies of rodents exposed to certain phthalates, high doses have been shown to change hormone levels and cause birth defects.[8] A British study showed that the phthalate di(n-butyl) phthalate (DBP) or its metabolite monobutyl phthalate (MBP) suppresses steroidogenesis by fetal-type Leydig cells in primates as in rodents.[26] And fly models have shown disruptions in insulin and glucagon signaling.[27]
In a study published in 2005, lead investigator Dr. Shanna Swan reported in the "Swan Study" that human phthalate exposure during pregnancy results in decreased anogenital distance among baby boys.[28] In this study, phthalate metabolites were measured in urine samples collected from the pregnant women having given birth to the infants. After birth, the genital features and anogenital distance of these women's babies were measured and correlated with the residue levels in the mother's urine. Boys born to mothers with the highest levels of phthalates were 7 times more likely to have a shortened anogenital distance.[28] An editorial concerning this paper in the same volume stated that the study population was small, and "needs to be investigated more thoroughly in a larger, more diverse population".[29] While anogenital distance is routinely used as a measure of fetal exposure to endocrine disruptors in animals,[30] this parameter is rarely assessed in humans, and its significance is unknown.[31] One paper states that "Whether anogenital distance measurements in humans relate to clinically important outcomes remains to be determined,"[32] and a National Toxicology Program expert panel concluded that anogenital distance is a "'novel index' whose relevance in humans 'has not been established,'" and that there is "insufficient evidence in humans" that DEHP causes harm.[33] The Swan study is thought by some to "suggest that male reproductive development in humans could be affected by prenatal exposure to environmentally relevant levels of phthalates."[34] Authors of a 2006 study of boys with undescended testis hypothesized that exposure to a combination of phthalates and anti-androgenic pesticides may have contributed to that condition.[35]
In contrast to the Swan study, an earlier study found that "adolescents exposed to significant quantities of DEHP as neonates showed no significant adverse effects on their physical growth and pubertal maturity."[36] This study, however, examined children exposed intravenously to phthalate diesters, and intravenous exposure results in little metabolic conversion of the relatively nontoxic phthalate diester to its more toxic monoester metabolite.[37]
In November 2009, Swan et al., in the International Journal of Andrology, in a paper titled "Prenatal phthalate exposure and reduced masculine play in boys",
"... suggest that prenatal exposure to antiandrogenic phthalates may be associated with less male-typical play behaviour in boys. ... [and] ... suggest that these ubiquitous environmental chemicals have the potential to alter androgen-responsive brain development in humans."[38][39]
A scientific review in 2013 came to the conclusion that epidemiological and in vitro studies generally converge sufficiently to conclude that phthalate anti-androgenicity is plausible in adult men.[25]
Endocannabinoid system disruption
Phthalates may act as endocrine disruptors and carcinogens. They also block CB1 as allosteric antagonists. Data are consistent with an allosteric mechanism for inhibition, with phthalates acting as relatively low affinity antagonists of CB(1) receptors and cannabinoid agonist-dependent activation of the G-protein.[40][41]
Prenatal exposure and birth defects in offspring
There is an inverse relationship between levels of metabolites of phthalates in the urine of pregnant women and the mental and intellectual development of the offspring. Intellectual deficits have been shown to persist even in children at the age of seven.[42]
Proposed effects of phthalates on prenatal development, fetuses, and infants include preterm birth, adverse effect on behavior, physiological abnormalities, and intellectual development issues. Because some phthalates compete for hormone receptors, they can block endogenous hormones from binding to cell structures. This can be disastrous for developing fetuses while their organ and neural systems are forming. Studies have shown that phthalates are anti-androgens that can be linked to urogenital malformation in males.[43] This means that their sexual organs do not develop normally and results in reduced anus-to-penis distance, undescended testicles, and other testicular abnormalities that result in decreased function. Though roughly 90% of mothers are exposed to phthalates, maternal uterine concentrations show that higher levels of exposure to phthalates are correlated with higher odds of the baby boy experiencing these abnormalities.
In a study conducted at Brigham and Women’s hospital between the years 2006 and 2008, it was concluded that women who had exposure to phthalate metabolites had significantly higher odds of spontaneous preterm birth than women who had little or no exposure to phthalates.[44] In turn, preterm birth results in higher odds of mortality, health and developmental problems, and complications to include acute respiratory, gastrointestinal, immunologic, central nervous system, hearing, vision, motor, cognitive, behavioral, socio-emotional, and growth problems.[45]
Additionally, prenatal exposure to phthalates has also shown associations with delinquent behavior later on in life. In a study looking at the effects of maternal exposure to phthalates, it was observed that both boys and girls scored higher in tests evaluating externalizing problems and aggressive behaviors in the clinical range in comparison to children who did not have high levels of prenatal phthalate exposure.[46]
Phthalates are also associated with altering brain development and gender specific behavior. As mentioned before, phthalates have anti-androgenic properties that are linked to suppression of activity of the androgen system and results in a more “female” version of the brain.[47] Studies conducted in preschool-aged children examined behavior in relation to mothers’ phthalate exposure suggest that early prenatal phthalate exposure can be linked to what is described as gender-specific behavior. The children from mothers with higher phthalates exposures choose to play with “boy typical toys” less often than the children from mothers with less phthalates exposure.[48] Other studies show that the exposure to phthalates may affect mental development differently by gender. The exposure during first trimester and study of neural development for first three years of life in children show no overall effect. But there is significant negative association between MDI (mental development index) and MEHP (mono-2-ethylhexyl-phthalate) exposure and neural development in girls but no association in boys.[49]
Other effects
There may be a link between the obesity epidemic and endocrine disruption and metabolic interference. Studies conducted on mice exposed to phthalates in utero did not result in metabolic disorder in adults.[50] However, "in a national cross-section of U.S. men, concentrations of several prevalent phthalate metabolites showed statistically significant correlations with abnormal obesity and insulin resistance."[50] Mono-ethylhexyl-phthalate (MEHP), a metabolite of DEHP, has been found to interact with all three peroxisome proliferator-activated receptors (PPARs).[50] PPARs are members of the nuclear receptor superfamily. The author of the study stated "The roles of PPARs in lipid and carbohydrate metabolism raise the question of their activation by a sub-class of pollutants, tentatively named metabolic disrupters."[50] Phthalates belong to this class of metabolic disruptors. It is a possibility that, over many years of exposure to these metabolic disruptors, they are able to deregulate complex metabolic pathways in a subtle manner.[50] A 2011 study of New York City children found an association between phthalate metabolite urinary concentrations and larger body size measurements.[51] A 2012 study suggested that high levels of phthalates may be connected to the current obesity epidemic in children. It was found that obese children show greater exposure to phthalates than nonobese children. It was reported that the obesity risk increases according to the level of the chemical found in the children's bloodstream.[52]
Large amounts of specific phthalates fed to rodents have been shown to damage their liver and testes,[8] and initial rodent studies also indicated hepatocarcinogenicity. Following this result, di(2-ethylhexyl) phthalate was listed as a possible carcinogen by IARC, EC, and WHO. Later studies on primates showed that the mechanism is specific to rodents - humans are resistant to the effect.[53] The carcinogen classification was subsequently withdrawn.
In 2004, a joint Swedish-Danish epidemiologic team found a link between allergies in children and the phthalates DEHP and BBzP. Their review article and meta-analysis of published data relating to phthalates and asthma found an association between phthalates in the home and asthma, especially in children, but this evidence was limited by imprecise data on levels of exposure.[54]
In 2007, a cross-sectional study of US males concluded that urine concentrations of four phthalate metabolites correlate with waist size and three phthalate metabolites correlate with the cellular resistance to insulin, a precursor to Type II diabetes. The authors note the need for follow-up longitudinal studies, as waist size is known to correlate with insulin resistance.[55] A 2012 study found that people with elevated phthalate levels had roughly twice the risk of developing diabetes compared with those with lower levels. They also found that phthalates were associated with disrupted insulin production.[56]
A 2009 study published in the Journal of Pediatrics found that prenatal phthalate exposure was related to low birth weight in infants. Low birth weight is the leading cause of death in children under 5 years of age and increases the risk of cardiovascular and metabolic disease in adulthood.[57] Researchers at the University of Michigan School of Public Health found that women that deliver prematurely have, on average, up to three times the phthalate level in their urine compared to women that carry to term.[58]
In 2009, South Korean scientists reported findings of a statistically significant correlation between urine phthalate concentrations in children and symptoms of ADHD. Although more research is needed in order to conclusively determine the relationship between phthalate and ADHD, the article suggests that consumers should be aware of its potential effects on behavior and neurological disorders.[59] The findings were replicated in The Mount Sinai Children's Environmental Health Study, which enrolled a multiethnic prenatal population in New York City between 1998 and 2002 (n= 404), published in Jan 2010. There was an association of prenatal phthalate exposure with offspring behavior and executive functioning at ages 4 to 9 years.[60]
A study published in 2011 followed the children of 319 women who gave birth between 1999 and 2006 to evaluate possible associations between prenatal exposures to phthalates and possible adverse effects in development at age 3 years. The results suggested that prenatal exposure to phthalates had affected the children's mental, motor and behavioral development during the preschool years. The senior epidemiologist on the study stated, "The results are concerning since increasing exposures from the lowest 25% to the highest 25% among the women in our study was associated with a doubling or tripling in the odds of motor and/or behavioral problems in the children".[61]
A 2012 study found a strong association between the presence of DEHP and diabetes. A 2013 study found that exposure to the industrial chemical can increase the risk of various allergic diseases in children. And a 2016 study concluded that it can also negatively affect child behavior. While there is less evidence that DiNP is problematic, some recent research suggests it very well could be. A study undertaken last year, for instance, found that exposure to the phthalate was associated with higher blood pressure.
Alternatives
There are numerous biological alternatives on the market. The problem is that they are typically expensive and not compatible as a primary plasticizer. However, Dioctyl terephthalate (a terephthalate isomeric with DEHP) and 1,2-Cyclohexane dicarboxylic acid diisononyl ester (a hydrogenated version of DINP) are available at cost-competitive pricing and with good plasticization properties.
A plasticizer based on vegetable oil that uses single reactor synthesis and is compatible as a primary plasticizer has been developed. It is a ready substitute for dioctyl phthalate.[62] And several other bio-based plasticizers have been and are being developed as alternatives to phthalates.
Legal status
European Union
The use of some phthalates has been restricted in the European Union for use in children's toys since 1999.[63] DEHP, BBP, and DBP are restricted for all toys; DINP, DIDP, and DNOP are restricted only in toys that can be taken into the mouth. The restriction states that the amount of these phthalates may not be greater than 0.1% mass percent of the plasticized part of the toy. Generally the high molecular weight phthalates DINP, DIDP and DPHP have been registered under REACH (see below) and have demonstrated their safety for use in current applications. They are not classified for any health or environmental effects.
The low molecular weight products BBP, DEHP, DIBP, and DBP were added to the Candidate list of Substances for Authorisation under REACH in 2008-9, and added to the Authorisation list, Annex XIV, in 2012.[64] This means that from February 2015 they are not allowed to be produced in the EU unless authorisation has been granted for a specific use, however they may still be imported in consumer products.[65] The creation of an Annex XV dossier, which could ban the import of products containing these chemicals, is being jointly prepared by the ECHA and Danish authorities and is expected to be submitted by April 2016.[66]
The Dutch office of Greenpeace UK sought to encourage the European Union to ban sex toys that contained phthalates.[67]
United States
During August 2008, the United States Congress passed and President George W. Bush signed the Consumer Product Safety Improvement Act (CPSIA), which became public law 110-314.[68] Section 108 of that law specified that as of February 10, 2009, "it shall be unlawful for any person to manufacture for sale, offer for sale, distribute in commerce, or import into the United States any children's toy or child care article that contains concentrations of more than 0.1 percent of" DEHP, DBP, or BBP and "it shall be unlawful for any person to manufacture for sale, offer for sale, distribute in commerce, or import into the United States any children's toy that can be placed in a child's mouth or child care article that contains concentrations of more than 0.1 percent of" DINP, DIDP, DnOP. Furthermore, the law requires the establishment of a permanent review board to determine the safety of other phthalates. Prior to this legislation, the Consumer Product Safety Commission had determined that voluntary withdrawals of DEHP and DINP from teethers, pacifiers, and rattles had eliminated the risk to children, and advised against enacting a phthalate ban.[69]
In another development in 1986, California voters approved an initiative to address their growing concerns about exposure to toxic chemicals. That initiative became the Safe Drinking Water and Toxic Enforcement Act of 1986, better known by its original name of Proposition 65.[70] In December 2013 DINP was listed as a chemical "known to the State of California to cause cancer"[71] This means that, starting December 2014, companies with 10 or more employees manufacturing, distributing or selling the product(s) containing diisononyl phthalate (DINP) are required to provide a clear and reasonable warning for that product. The California Office of Environmental Health Hazard Assessment, charged with maintaining the Proposition 65 list and enforcing its provisions, has implemented a "No Significant Risk Level" of 146 ug/day for DINP, as of 1 April 2016.
Identification in plastics
Phthalates are used in some but not all PVC formulations, and there are no specific labeling requirements for phthalates. PVC plastics are typically used for various containers and hard packaging, medical tubing, and bags, and are labelled "Type 3" for recycling reasons. However, the presence of phthalates rather than other plasticizers is not marked on PVC items. Only unplasticized PVC (uPVC), which is mainly used as a hard construction material, has no plasticizers. If a more accurate test is needed, chemical analysis, for example by gas chromatography or liquid chromatography, can establish the presence of phthalates.
Polyethylene terephthalate (PETE) is the main substance used to package bottled water and many sodas. Products containing PETE are labeled "Type 1" (with a "1" in the recycle triangle) for recycling purposes. Although the word "phthalate" appears in the name, PETE does not use phthalates as plasticizers. The terephthalate polymer PETE and the phthalate ester plasticizers are chemically different substances.[72] Despite this, however, a number of studies have found phthalates such as DEHP in bottled water and soda.[73] One hypothesis is that these may have been introduced during plastics recycling.[73] Several studies tested the liquids before they were bottled, in order to make sure the phthalates came from the bottles rather than already being in the water.
Detection in food products
In February 2009, the Joint Research Centre (JRC) of the European Commission published a review of methods to measure phthalates in food.[74]
See also
- Xenoestrogen
- Non-phthalate plasticizers such as 1,2-Cyclohexane dicarboxylic acid diisononyl ester, Dioctyl terephthalate, and Citrates
References
- ↑ "ACC Addresses Phthalates Safety" on YouTube: video of Steve Risotto of the American Chemistry Council, uploaded by user AmericanChemistry on 23 Oct 2009, retrieved 23 Dec 2011.
- ↑ "phthalate, n.". oed.com.
- ↑ Ceresana. "Plasticizers – Study: Market, Analysis, Trends - Ceresana". ceresana.com.
- 1 2 ehp.1205256_508 (PDF)
- ↑ bilder.buecher.de (PDF)
- 1 2 Phthalates FactSheet (PDF)
- ↑ "4. To what extent are people exposed to phthalates?". europa.eu.
- 1 2 3 Third National Report on Human Exposure to Environmental Chemicals, (PDF) U.S. CDC, July 2005. Archived April 1, 2007, at the Wayback Machine.
- 1 2 3 Rudel R, Perovich L (January 2008). "Endocrine disrupting chemicals in indoor and outdoor air". Atmospheric Environment. 43 (1): 170–81. doi:10.1016/j.atmosenv.2008.09.025. PMC 2677823
 . PMID 20047015.
. PMID 20047015. - ↑ Malveda, Michael P (July 2015). "Chemical Economics Handbook Report on Plasticizers".
- ↑ 23 May 2012 Expertsvar (2012-05-23). "Phthalates in PVC floors taken up by the body in infants". Alphagalileo.org. Retrieved 2013-09-23.
- ↑ "Phthalates in PVC floors taken up by the body in infants". Sciencedaily.com. 2012-05-23. doi:10.1111/j.1600-0668.2012.00788. Retrieved 2013-09-23.
- ↑ Erythropel, Hanno C.; Maric, Milan; Nicell, Jim A.; Leask, Richard L.; Yargeau, Viviane (2014-12-01). "Leaching of the plasticizer di(2-ethylhexyl)phthalate (DEHP) from plastic containers and the question of human exposure". Applied Microbiology and Biotechnology. 98 (24): 9967–9981. doi:10.1007/s00253-014-6183-8. ISSN 1432-0614. PMID 25376446.
- 1 2 Heudorf U, Mersch-Sundermann V, Angerer J (October 2007). "Phthalates: toxicology and exposure". Int J Hyg Environ Health. 210 (5): 623–34. doi:10.1016/j.ijheh.2007.07.011. PMID 17889607.
- 1 2 3 Kolarik B, Bornehag C, Naydenov K, Sundell J, Stavova P, Nielsen O (December 2008). "The concentration of phthalates in settled dust in Bulgarian homes in relation to building characteristic and cleaning habits in the family". Atmospheric Environment. 42 (37): 8553–9. doi:10.1016/j.atmosenv.2008.08.028.
- ↑ Sathyanarayana S, Karr CJ, Lozano P, et al. (February 2008). "Baby care products: possible sources of infant phthalate exposure". Pediatrics. 121 (2): e260–8. doi:10.1542/peds.2006-3766. PMID 18245401.
- 1 2 Sathyanarayana S (2008). "Phthalates and children's health". Current Problems In Adolescent Health Care. 38: 34–39. doi:10.1016/j.cppeds.2007.11.001.
- ↑ "Phthalates in school supplies". GreenFacts Website. Retrieved 2009-06-10.
- 1 2 3 Hernández-Díaz S, Mitchell AA, Kelley KE, Calafat AM, Hauser R (February 2009). "Medications as a Potential Source of Exposure to Phthalates in the U.S. Population". Environ. Health Perspect. 117 (2): 185–9. doi:10.1289/ehp.11766. PMC 2649218
 . PMID 19270786.
. PMID 19270786.
- ↑ Committee on the Health Risks of Phthalates, National Research Council. (2008). Phthalates and Cumulative Risk Assessment: The Task Ahead. National Academies Press. Free full-text available.
- 1 2 3 4 5 6 7 8 Lopez-Carillo L.; Hernandez-Ramirez R.U.; Calafat A.M.; Torres-Sanchez L.; Galvan-Portillo M.; Needham L.L.; Ruiz-Ramos R.; Cebrian M.E. (2010). "Exposure to phthalates and breast cancer risk in Northern Mexico". Environmental Health Perspectives. 118 (4): 539–544. doi:10.1289/ehp.0901091. PMC 2854732
 . PMID 20368132.
. PMID 20368132. - ↑ http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:31976L0768:EN:HTML
- ↑ Waring R.H.; Harris R.M. (2011). "Endocrine disrupters – a threat to women's health?". Maturitas. 68: 111–115. doi:10.1016/j.maturitas.2010.10.008.
- ↑ breast cancer risk factors 5/7/2011. (Cancer.org).
- 1 2 Albert, O.; Jegou, B. (2013). "A critical assessment of the endocrine susceptibility of the human testis to phthalates from fetal life to adulthood". Human Reproduction Update. 20 (2): 231–49. doi:10.1093/humupd/dmt050. PMID 24077978.
- ↑ Hallmark N, Walker M, McKinnell C, et al. (March 2007). "Effects of Monobutyl and Di(n-butyl) Phthalate in Vitro on Steroidogenesis and Leydig Cell Aggregation in Fetal Testis Explants from the Rat: Comparison with Effects in Vivo in the Fetal Rat and Neonatal Marmoset and in Vitro in the Human". Environ. Health Perspect. 115 (3): 390–6. doi:10.1289/ehp.9490. PMC 1849934
 . PMID 17431488.
. PMID 17431488. - ↑ Williams MJ, Wiemerslage L, Gohel P, Kheder S, Kothegala LV, Schiöth HB (2016). "Dibutyl Phthalate Exposure Disrupts Evolutionarily Conserved Insulin and Glucagon-Like Signaling in Drosophila Males.". Endocrinology. doi:10.1210/en.2015-2006. PMID 27100621.
- 1 2 Swan SH, Main KM, Liu F, Stewart SL, Kruse RL, Calafat AM, Mao CS, Redmon JB, Ternand CL, Sullivan S, Teague JL (August 2005). "Decrease in Anogenital Distance among Male Infants with Prenatal Phthalate Exposure". Environ. Health Perspect. 113 (8): 1056–61. doi:10.1289/ehp.8100. PMC 1280349
 . PMID 16079079.
. PMID 16079079. - ↑ Barrett, Julia R. (2005). "Phthalates and Baby Boys: Potential Disruption of Human Genital Development". Environ Health Perspect. 113 (8): A542. doi:10.1289/ehp.113-a542a. PMC 1280383
 .
. - ↑ Salazar-Martinez E, Romano-Riquer P, Yanez-Marquez E, Longnecker MP, Hernandez-Avila M (2004). "Anogenital distance in human male and female newborns: a descriptive, cross-sectional study". Environ Health. 3 (1): 8. doi:10.1186/1476-069X-3-8. PMC 521084
 . PMID 15363098. Retrieved 2008-06-20.
. PMID 15363098. Retrieved 2008-06-20. - ↑ Postellon, Daniel C. (June 2008). "Baby Care Products" (letter). Pediatrics. 121 (6): 1292; author reply 1292–3. doi:10.1542/peds.2008-0401. PMID 18519505. Retrieved 2008-06-03.
- ↑ Romano-Riquer SP, Hernández-Avila M, Gladen BC, Cupul-Uicab LA, Longnecker MP (2007). "Reliability and determinants of anogenital distance and penis dimensions in male newborns from Chiapas, Mexico". Paediatr Perinat Epidemiol. 21 (3): 219–28. doi:10.1111/j.1365-3016.2007.00810.x. PMID 17439530.
- ↑ Kaiser J (October 2005). "Toxicology. Panel finds no proof that phthalates harm infant reproductive systems". Science. 310 (5747): 422. doi:10.1126/science.310.5747.422a. PMID 16239449.
- ↑ Tilson HA (June 2008). "EHP Papers of the Year, 2008". Environ. Health Perspect. 116 (6): A234. doi:10.1289/ehp.11684. PMC 2430244
 .
. - ↑ Toppari J, Virtanen H, Skakkebaek NE, Main KM (2006). "Environmental effects on hormonal regulation of testicular descent". J Steroid Biochem Mol Biol. 102 (1–5): 184–6. doi:10.1016/j.jsbmb.2006.09.020. PMID 17049842.
- ↑ Rais-Bahrami K, Nunez S, Revenis ME, Luban NL, Short BL (September 2004). "Follow-Up Study of Adolescents Exposed to Di(2-Ethylhexyl) Phthalate (DEHP) as Neonates on Extracorporeal Membrane Oxygenation (ECMO) Support". Environ. Health Perspect. 112 (13): 1339–40. doi:10.1289/ehp.6901. PMC 1247527
 . PMID 15345350.
. PMID 15345350. - ↑ Huber WW, Grasl-Kraupp B, Schulte-Hermann R (1996). "Hepatocarcinogenic potential of di(2-ethylhexyl)phthalate in rodents and its implications on human risk". Crit Rev Toxicol. 26 (4): 365–481. doi:10.3109/10408449609048302. PMID 8817083.
- ↑ "Phthalate exposure linked to less-masculine play by boys". Sciencedaily.com. 2009-11-16. Retrieved 2013-09-23.
- ↑ Swan SH; Liu F; Hines M; et al. (April 2010). "Prenatal phthalate exposure and reduced masculine play in boys". International Journal of Andrology. 33: 259–269. doi:10.1111/j.1365-2605.2009.01019.x. PMC 2874619
 . PMID 19919614.
. PMID 19919614.
- ↑ McPartland, John M.; Guy, Geoffrey W.; Di Marzo, Vincenzo (2014-03-12). "Care and Feeding of the Endocannabinoid System: A Systematic Review of Potential Clinical Interventions that Upregulate the Endocannabinoid System". PLoS ONE. 9 (3). doi:10.1371/journal.pone.0089566. ISSN 1932-6203. PMC 3951193
 . PMID 24622769.
. PMID 24622769. - ↑ Bisset, Kathleen M.; Dhopeshwarkar, Amey S.; Liao, Chengyong; Nicholson, Russell A. (2011-10-01). "The G protein-coupled cannabinoid-1 (CB1) receptor of mammalian brain: inhibition by phthalate esters in vitro". Neurochemistry International. 59 (5): 706–713. doi:10.1016/j.neuint.2011.06.019. ISSN 1872-9754. PMID 21763743.
- ↑ Factor-Litvak, P; Insel, B; Calafat, A. M.; Liu, X; Perera, F; Rauh, V. A.; Whyatt, R. M. (2014). "Persistent Associations between Maternal Prenatal Exposure to Phthalates on Child IQ at Age 7 Years". PLoS ONE. 9 (12): e114003. doi:10.1371/journal.pone.0114003. PMC 4262205
 . PMID 25493564.
. PMID 25493564. - ↑ "Phthalates and Baby Boys: Potential Disruption of Human Genital Development". Environmental Health Perspectives. 113 (8): A542. doi:10.1289/ehp.113-a542a. PMC 1280383
 .
. - ↑ http://archpedi.jamanetwork.com/article.aspx?articleid=1769137#Discussion
- ↑ http://www.ncbi.nlm.nih.gov/books/NBK11362/
- ↑ http://ehp.niehs.nih.gov/1307154/
- ↑ https://www.novapublishers.com/catalog/product_info.php?products_id=40906
- ↑ http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2605.2009.01019.x/abstract
- ↑ "Prenatal urinary phthalate metabolites levels and neurodevelopment in children at two and three years of age". Science of The Total Environment. 461-462: 386–390. doi:10.1016/j.scitotenv.2013.05.021.
- 1 2 3 4 5 Desvergne B, Feige J, Casals-Casas C (2009). "PPAR-mediated activity of phthalates: A link to the obesity epidemic?". Mol Cell Endocrinol. 304 (1–2): 43–8. doi:10.1016/j.mce.2009.02.017. PMID 19433246.
- ↑ "Associations between phthalate metabolite urinary concentrations and body size measures in New York City children". Environmental Research. 112: 186–193. doi:10.1016/j.envres.2011.12.006. Retrieved 2013-09-23.
- ↑ "Phthalate, environmental chemical is linked to higher rates of childhood obesity". Sciencedaily.com. 2012-06-26. Retrieved 2013-09-23.
- ↑ "Chronic Hazard Advisory on Diisononyl Phthalate" (PDF). 2001. p. 87. Retrieved 2009-01-31.
Human risk is therefore seen as negligible
- ↑ Bornehag CG, Sundell J, Weschler CJ, Sigsgaard T, Lundgren B, Hasselgren M, Hägerhed-Engman L (October 2004). "The Association between Asthma and Allergic Symptoms in Children and Phthalates in House Dust: A Nested Case–Control Study". Environ. Health Perspect. 112 (14): 1393–7. doi:10.1289/ehp.7187. PMC 1247566
 . PMID 15471731.
. PMID 15471731. The lack of objective exposure information limits the epidemiologic data
- ↑ Stahlhut RW, van Wijngaarden E, Dye TD, Cook S, Swan SH (June 2007). "Concentrations of Urinary Phthalate Metabolites Are Associated with Increased Waist Circumference and Insulin Resistance in Adult U.S. Males". Environ. Health Perspect. 115 (6): 876–82. doi:10.1289/ehp.9882. PMC 1892109
 . PMID 17589594.
. PMID 17589594. - ↑ 11 April 2012 Uppsala Universitet (2012-04-11). "High levels of phthalates can lead to greater risk for type-2 diabetes". Alphagalileo.org. Retrieved 2013-09-23.
- ↑ "Exposure To Phthalates May Be A Risk Factor For Low Birth Weight In Infants". Sciencedaily.com. 2009-06-25. doi:10.1016/j.jpeds.2009.04.007. Retrieved 2013-09-23.
- ↑ "Chemical In Common Consumer Products (Phthalates) May Play A Role In Pre-term Births". Sciencedaily.com. 2009-07-07. doi:10.1289/ehp.0800522. Retrieved 2013-09-23.
- ↑ Kim Bung-Nyun; Cho Soo-Churl; Kim Yeni; Shin Min-Sup; Yoo Hee-Jeong; Kim Jae-Won; Hee Yang Young; Kim Hyo-Won; Bhang Soo-Young; Hong Yun-Chul (2009). "Phthalates Exposure and Attention-Deficit/Hyperactivity Disorder in School-Age Children". Biological Psychiatry. 66 (10): 958–963. doi:10.1016/j.biopsych.2009.07.034.
- ↑ Engel SM, Miodovnik A, Canfield RL, Zhu C, Silva MJ, Calafat AM, Wolff MS (2010). "Prenatal Phthalate Exposure Is Associated with Childhood Behavior and Executive Functioning". Environ. Health Perspect. 2010 Jan 8. [Epub ahead of print] (4): 565–71. doi:10.1289/ehp.0901470. PMC 2854736
 . PMID 20106747.
. PMID 20106747. - ↑ "Prenatal exposure to phthalates linked to decreased mental and motor development". Sciencedaily.com. 2011-09-07. doi:10.1289/ehp.1103705. Retrieved 2013-09-23.
- ↑ "Bio-based plasticizer". University of Minnesota.
- ↑ Ban of phthalates in childcare articles and toys, press release IP/99/829, 10 November 1999
- ↑ ECHA Website - Proposal for identification of Substances of Very High Concern Retrieved 22 December 2014
- ↑ https://chemicalwatch.com/23104/echa-and-denmark-to-prepare-phthalates-restriction
- ↑ http://echa.europa.eu/registry-of-current-restriction-proposal-intentions/-/substance-rev/6301/term
- ↑ Ms. KFT Retrieved 22 December 2014
- ↑ GovTrack.us. "H.R. 4040--110th Congress (2007): Consumer Product Safety Improvement Act of 2008, GovTrack.us (database of federal legislation) . Retrieved 14 August 2009.
- ↑ Public Concern, Not Science, Prompts Plastics Ban by Jon Hamilton, NPR.
- ↑ "OEHHA Proposition 65: Proposition 65 in Plain Language!". ca.gov.
- ↑ "OEHHA Proposition 65 (2013) Diisononyl Phthalate (DINP) listed". ca.gov.
- ↑ "Learn the Facts About Food Packaging and Phthalates". Plasticsmythbuster.org. Retrieved 2013-09-23.
- 1 2 Sax, Leonard (2010-04-01). "Polyethylene Terephthalate May Yield Endocrine Disruptors". Environmental Health Perspectives. 118 (4): 445–448. doi:10.1289/ehp.0901253. ISSN 0091-6765. PMC 2854718
 . PMID 20368129.
. PMID 20368129. - ↑ Methods for the determination of phthalates in food, (PDF) European Commission, Joint Research Centre Archived July 20, 2011, at the Wayback Machine.
Further reading
- Hauser R, Meeker JD, Singh NP, et al. (March 2007). "DNA damage in human sperm is related to urinary levels of phthalate monoester and oxidative metabolites". Hum. Reprod. 22 (3): 688–95. doi:10.1093/humrep/del428. PMID 17090632.
- Drew CH, Grace DA, Silbernagel SM, et al. (March 2003). "Nuclear waste transportation: case studies of identifying stakeholder risk information needs". Environ. Health Perspect. 111 (3): 263–72. doi:10.1289/ehp.5203. PMC 1241381
 . PMID 12611653.
. PMID 12611653. - Swan, S.H. 2004. Phthalates in pregnant women and children. e.hormone 2004 conference. October 27–30. New Orleans.
- Lovekamp-Swan T, Davis BJ (February 2003). "Mechanisms of phthalate ester toxicity in the female reproductive system". Environ. Health Perspect. 111 (2): 139–45. doi:10.1289/ehp.5658. PMC 1241340
 . PMID 12573895.
. PMID 12573895. - Gray LE, Ostby J, Furr J, Price M, Veeramachaneni DN, Parks L (December 2000). "Perinatal exposure to the phthalates DEHP, BBP, and DINP, but not DEP, DMP, or DOTP, alters sexual differentiation of the male rat". Toxicol. Sci. 58 (2): 350–65. doi:10.1093/toxsci/58.2.350. PMID 11099647.
- Tickner JA, Schettler T, Guidotti T, McCally M, Rossi M (January 2001). "Health risks posed by use of Di-2-ethylhexyl phthalate (DEHP) in PVC medical devices: a critical review". Am. J. Ind. Med. 39 (1): 100–11. doi:10.1002/1097-0274(200101)39:1<100::AID-AJIM10>3.0.CO;2-Q. PMID 11148020.
- Kohn MC, Parham F, Masten SA, et al. (October 2000). "Human exposure estimates for phthalates". Environ. Health Perspect. 108 (10): A440–2. doi:10.2307/3435033. JSTOR 3435033. PMC 1240144
 . PMID 11097556.
. PMID 11097556. - Centers for Disease Control. "National Report on Human Exposure to Environmental Chemicals. Updated Tables, February 2011". Archived from the original on November 29, 2010.
- Centers for Disease Control. "Phthalate Fact Sheet". Archived from the original on December 29, 2010.
- Centers for Disease Control. "Agency for Toxic Substances and Disease Registry-Public Health Statement for Di(2-ethylhexyl) phthalate DEHP".
- Davis, B.J., Maronpot, R.R. & Heindel, J.J. (1994). "Di (2-ethylhexyl) phthalate suppresses estradiol and ovulation in cycling rats". Toxicol Appl Pharmacol. 128 (2): 216–233. doi:10.1006/taap.1994.1200.
- Latini, G.; Del Vecchio, A.; et al. (2006). "Phthalate Exposure and Male Infertility". Toxicology. 226 (2–3): 90–98. doi:10.1016/j.tox.2006.07.011. PMID 16905236.
- Mendes, Amaral J. (2002). "The endocrine disruptors: a major medical challenge". Food and Chemical Toxicology. 40 (6): 781–788. doi:10.1016/S0278-6915(02)00018-2. PMID 11983272.
- Factor-Litvak P; Insel B; Calafat AM; Liu X; Perera F; et al. (2014). ": Persistent Associations between Maternal Prenatal Exposure to Phthalates on Child IQ at Age 7 Years.". PLoS ONE. 9: e114003. doi:10.1371/journal.pone.0114003. PMC 4262205
 . PMID 25493564.
. PMID 25493564. - Net Sopheak; Sempéré Richard; Delmont Anne; Paluselli Andrea; Ouddane Baghdad (2015). "Occurrence, Fate, Behavior and Ecotoxicological State of Phthalates in Different Environmental Matrices.". Environmental Science & Technology. 49: 4019–4035. doi:10.1021/es505233b.
External links
Research
- Bornehag CG, Sundell J, Weschler CJ, et al. (October 2004). "The Association between Asthma and Allergic Symptoms in Children and Phthalates in House Dust: A Nested Case–Control Study". Environ. Health Perspect. 112 (14): 1393–7. doi:10.1289/ehp.7187. PMC 1247566
 . PMID 15471731.
. PMID 15471731. - DIDP (PDF), DINP (PDF), and DBP (PDF) - Risk Assessment Reports by the European Chemicals Bureau (ECB).
- López-Carrillo L, Hernández-Ramírez RU, Calafat AM, et al. (December 2009). "Exposure to Phthalates and Breast Cancer Risk in Northern Mexico". Environ. Health Perspect. 118 (4): 539–44. doi:10.1289/ehp.0901091. PMC 2854732
 . PMID 20368132.
. PMID 20368132.
Sources suggesting low/no health risks
- Phthalates Information Centre; an initiative of the European Council for Plasticisers and Intermediates (ECPI)
- Phthalates Information Center; from the American Chemistry Council, Inc.
- Phthalates and Human Health, by Kenneth Green, D.Env.; Director of the Environmental Program at Reason Public Policy Institute, Reason Foundation, 2000
Media
- NOW on PBS: Phthalates and Toxic Toys?
- Interview with Mark Schapiro from Fresh Air (NPR) ; November 26, 2007
- Phthalates Now Linked to Fat, Related Health Risks, University of Rochester Medical Center, March 14, 2007.
- New Scientist and Scientific American articles on Environmental Health Perspectives report; see Research.
- Panel Ranks Risks of Common Phthalate: Additional research underscores concerns about DEHP that were first expressed in 2000 report, Bette Hileman, Chemical and Engineering News, NOVEMBER 14, 2005, 83(46):32–36.
- Congress Bans Toxic Phthalates from Toys, Everett Sizemore, US Recall News, August 13, 2008
- http://www.ted.com/talks/two_young_scientists_break_down_plastics_with_bacteria.html