Donohue syndrome
| Donohue syndrome | |
|---|---|
 | |
| insulin receptor | |
| Classification and external resources | |
| OMIM | 246200 |
| DiseasesDB | 30801 |
Donohue syndrome (also known as Leprechaunism) is an extremely rare and severe genetic disorder. Leprechaunism derives its name from the fact that people with the disease often have elfin features and are smaller than usual. Affected individuals have an insulin receptor with greatly impaired functionality.
Presentation
Facial features indicative of Donohue syndrome include protuberant and low-set ears, flaring nostrils, and thick lips. Physical features include stunted growth (including during gestation), an enlarged clitoris and breasts in affected females, and an enlarged penis in affected males. In the Journal of Pediatric Medicine, Donohue and Uchida described affected sisters whose growth appeared to have ended in the seventh month of gestation, both born alive but dying before four months of age.[1] Very early death (or spontaneous abortion) is the norm, although sufferers sometimes live longer than a decade.[1][2]
As the mutation causing the disorder affects insulin receptor function, those with the disease are also insulin resistant, with hyperglycemia and profound hyperinsulinemia (very high levels of insulin in the blood)[1] Another feature of the disease is that the subcutaneous adipose tissue is markedly diminished, which contributes to the unusual appearance of affected individuals.
A much milder form of the disease, in which there is some insulin resistance but normal growth and subcutaneous fat distribution, is also known.[3] It is caused by a less severe mutation of the same gene.
Genetics
Donohue syndrome is an autosomal recessive genetic disorder. The mutations responsible for the disorder are found on the short arm chromosome 19 (19p13.2) within the coding sequence of the INSR gene (insulin receptor) causing the production of inactive receptor molecules.[2] There are several mutations that can be responsible for the disease, as any mutation that severely impairs the functionality of the insulin receptor will have similar effects. The INSR gene spans over one hundred and twenty thousand base pairs, which contain twenty-two exons coding for a protein that consists of 1382 amino acids.[4] Some of the introns may or may not be spliced out depending on the kind of cell.[5]
Known mutations to the gene which can cause Donohue syndrome include a nonsense mutation that resulted in a frame shift,[6] a single missense mutation[1] and in the milder form mentioned above, a single codon change that altered isoleucine to methionine in the receptor protein.[1] Some mutations to the gene instead result in insulin resistant diabetes without Donohue syndrome.[1]
Because mutations in the gene are extremely rare, most cases result from consanguineous matings, for example, between cousins.[1] However, the exact mutation need not be the same. Disease can be caused by inheritance of two different mutant alleles, one from each parent, in which case the patient is a compound heterozygote.[7]
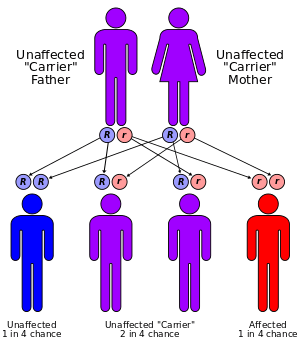
A heterozygous individual (i.e. one who is a carrier for the disease, having only one normal allele for the insulin receptor) will not be affected. Two heterozygous parents have, in theory, a one in four chance of having a child with the disease, and two thirds of their unaffected children will be carriers. However, because spontaneous abortion (miscarriage) often results when the fetus has the disease, in actuality the proportion of children born alive with Donohue syndrome will be lower than 25%.[1]
It is possible to do a genetic test to identify carriers, but because it is so rare, this is not usually done unless there is reason to suspect that the individual being tested is a carrier, for instance having an affected sibling or cousin. As expected for a genetic disease that can be caused by many different mutations, it is not limited to a specific ethnic group, and has been seen in people of various races.
Pathophysiology
The cause of the disease is the lack of a fully functional insulin receptor, which has a profound effect during fetal development and thereafter. In one case, it was found (by culturing pancreatic cells) that the receptor produced by the mutant allele is only about 15% as effective as the normal receptor.[1] The beta cells in the pancreas, which make and store insulin and release it on an as-needed basis, are often found to be very large or numerous.[1]
In some patients, particularly those who are longer-lived, unusual bone changes are sometimes seen, and there may be excessive body hair[1] and velvety hyperpigmentation of the skin.
The prognosis is quite dire, with early death usual.[2] In fact, most patients die in their first year except in milder forms of the disease, but few are known to have lived longer.[1] The variation is unsurprising given the diversity of mutations causing the disease.
Many of the problems associated with Donohue syndrome may be due to the insulin receptor binding the insulin-like growth factor, regulating the growth of the embryo, in addition to its well-known role in the regulation of blood sugar.[8]
Eponym
Donohue syndrome was first identified in 1948 by Canadian pathologist William L. Donohue (1906-1985).[9] The name leprechaunism has been largely abandoned because of the perception of the name by some parents of patients as insulting.[1]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Online Mendelian Inheritance in Man (OMIM) Insulin Receptor -147670
- 1 2 3 Longo N, Wang Y, Smith SA, Langley SD, DiMeglio LA, Giannella-Neto D (2002). "Genotype-phenotype correlation in inherited severe insulin resistance". Hum. Mol. Genet. 11 (12): 1465–75. doi:10.1093/hmg/11.12.1465. PMID 12023989.
- ↑ al-Gazali LI, Khalil M, Devadas K (1993). "A syndrome of insulin resistance resembling leprechaunism in five sibs of consanguineous parents". J. Med. Genet. 30 (6): 470–5. doi:10.1136/jmg.30.6.470. PMC 1016418
 . PMID 8326490.
. PMID 8326490. - ↑ NCBI Sequence Viewer v2.0
- ↑ Benecke H, Flier JS, Moller DE (1992). "Alternatively spliced variants of the insulin receptor protein. Expression in normal and diabetic human tissues". J. Clin. Invest. 89 (6): 2066–70. doi:10.1172/JCI115819. PMC 295926
 . PMID 1602013.
. PMID 1602013. - ↑ Psiachou H, Mitton S, Alaghband-Zadeh J, Hone J, Taylor SI, Sinclair L (1993). "Leprechaunism and homozygous nonsense mutation in the insulin receptor gene". Lancet. 342 (8876): 924. doi:10.1016/0140-6736(93)91970-W. PMID 8105179.
- ↑ Elsas LJ, Endo F, Strumlauf E, Elders J, Priest JH (1985). "Leprechaunism: an inherited defect in a high-affinity insulin receptor". Am. J. Hum. Genet. 37 (1): 73–88. PMC 1684537
 . PMID 3883764.
. PMID 3883764. - ↑ Personal communication with J. Bell, Ph.D.
- ↑ Donohue WL; Edwards, HE (1948). "Dysendocrinism". The Journal of Pediatrics. 32 (6): 739–48. doi:10.1016/S0022-3476(48)80231-3. PMID 18866943.