Cardiac contractility modulation
.jpg)
Cardiac contractility modulation (CCM) is a treatment for patients with moderate to severe left ventricular systolic heart failure (NYHA class II–IV). The short- and long-term use of this therapy enhances both the strength of ventricular contraction and the heart’s pumping capacity by modulating (adjusting) the myocardial contractility. The CCM mechanism is based on stimulation of the cardiac muscle by non-excitatory electrical signals (NES). CCM treatment is delivered by a pacemaker-like device that applies the NES, adjusted to and synchronized with the electrical action in the cardiac cycle.[1][2][3]
In CCM therapy, electrical stimulation is applied to the cardiac muscle during the absolute refractory period. In this phase of the cardiac cycle, electrical signals cannot trigger new cardiac muscle contractions, hence this type of stimulation is known as a non-excitatory stimulation. However, the electrical CCM signals increase the influx of calcium ions into the cardiac muscle cells (cardiomyocytes).[4][5] In contrast to other electrical stimulation treatments for heart failure, such as pacemaker therapy or implantable cardioverter defibrillators (ICD), CCM does not affect the cardiac rhythm directly. Rather, the aim is to enhance the heart’s natural contraction (the native cardiac contractility) sustainably over long periods of time. Furthermore, unlike most interventions that increase cardiac contractility, CCM is not associated with an unfavorable increase in oxygen demand by the heart (measured in terms of Myocardial Oxygen Consumption or MVO2). This may be explained by the beneficial effect CCM has in improving cardiac efficiency.[6][7][8] A meta-analysis in 2014[2] and an overview of device-based treatment options in heart failure in 2013[1] concluded that CCM treatment is safe,[1][9] that it is generally beneficial to patients[1][9] and that CCM treatment increases the exercise tolerance (ET) and quality of life (QoL) of patients.[2] Furthermore, preliminary long-term survival data shows that CCM is associated with lower long-term mortality in heart failure patients when compared with expected rates among similar patients not treated with CCM.[10]
Medical uses
Approval
Based on the results of clinical trials,[3][11] CCM devices are approved and available for clinical use in all European Union countries and in Australia, Turkey, India and Hong Kong, as well as in other countries that recognize CE marking for medical devices.
At the present time, CCM therapy is not approved for clinical use in the United States. However, a study has been initiated in order to obtain FDA approval.[11][12]
Indication
Based on the approval of CCM devices, cardiac contractility modulation is a treatment option for patients that are at least 18 years old who suffer from heart failure symptoms due to left ventricular systolic dysfunction (LVSD) despite adequate medical treatment. Further clinical research is required to identify which patient group within the scope of the device approval benefits most from CCM treatment.[1][2][3][12]
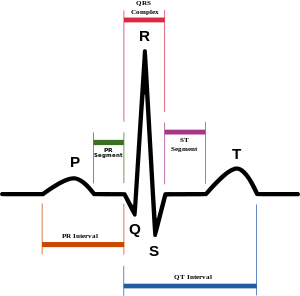
Criteria for the classification of patients with left ventricular systolic heart failure include the severity of the disease based on functional parameters (NYHA classification), the average percentage of blood volume ejected by the left ventricle with each heart beat (left ventricular ejection fraction or LVEF) and the duration of the QRS complex seen in the electrocardiogram (ECG). Most clinical studies on CCM therapy have involved heart failure patients who were classified initially as NYHA Class II, III or IV and had a normal QRS duration (QRS duration ≤ 120 ms). The efficacy of CCM on patients in an earlier stage of heart failure has not yet been studied.[2][13]
A subsequent evaluation study (subgroup analysis) has already suggested a particular patient group that responds exceptionally well to CCM therapy. The patients were characterized by a disease severity of NYHA class III and a left ventricular ejection fraction of ≥ 25%.[1][14]
Although studies on CCM therapy have focused on patients with a normal QRS duration (i.e. ≤ 120 ms), it is possible to use CCM in patients who meet the treatment indication but who do not have a normal QRS duration.[3][15][16] A preliminary study has previously shown that CCM may be safe and effective in such patients who have not responded to cardiac resynchronization therapy (CRT).[17]
Therapeutic gap
Cardiac resynchronization therapy (CRT; also known as biventricular pacing) has proven to be an effective treatment in heart failure.[18] However, CRT is generally recommended exclusively for patients with a preserved sinus rhythm and a prolonged QRS complex (≥ 120 ms) who also suffer from left bundle branch block (LBBB), or for patients without left bundle branch block but who have a preserved sinus rhythm and a QRS complex with a width of ≥ 150 ms.[18] However, only 30-40% of all heart failure patients show such a prolonged QRS complex,[2][13][15] and therefore the 60-70% of patients who have a normal QRS complex cannot be treated with CRT. In addition, around 30% of the patients eligible for CRT treatment do not respond to CRT.[2][13][15]
Until recently, the only other available device-based treatment was the left ventricular assist device (LVAD). LVAD therapy is indicated in patients with severe illness and is associated with several hours of surgery (involving a cardiopulmonary bypass). It is usually considered as a therapy providing a “bridge to transplant” for heart failure patients classified as NYHA class IV, and is intended to support heart function until a heart transplant is received.[2][13][15] Current research results suggest that the therapeutic gap described above could now be closed by CCM therapy.[2][13][15] Additionally, a long-term study on CCM showed that the therapy was able to stop the common and prognostically unfavorable long-term prolongation of QRS duration in heart failure patients. This result was interpreted as signaling the safety of the treatment and as an indicator that patients could benefit from CCM therapy in the long term. If the QRS-stabilizing effect were to be confirmed in further studies, CCM would become the first device-based treatment for heart failure with the potential to halt QRS prolongation, a factor associated with a poor prognosis.[19]
Recommendations
As of February 2015, no recommendations concerning the use of CCM in the treatment of heart failure are available from either national or international medical societies. This includes the guidelines issued by the European Society of Cardiology (ESC), which were most recently updated in 2012 and in most cases are endorsed by national cardiac societies in individual countries within the European Union.[18][20]
This deficiency has been criticized by experts and has served as one of two cases brought forward in a request to discuss the assessment criteria of the ESC.[21]
Efficacy
Cardiac contractility modulation has proven to be effective and safe in randomized controlled trials involving several hundred patients.[22][23][24]
The nature and extent of the effect of CCM have been the subject of numerous investigations. Although various individual publications, as well as one of two meta-analyses, have presented CCM‘s efficacy and significant potential in treatment of heart failure, medical evaluation of the therapy efficacy is not yet complete. Scientists point out, however, that this was also the case for CRT therapy when it was first introduced, advocating the provision of CCM to suitable patients before further studies are completed.[3][15]
To date (February 2015), there are at least two meta-analyses studying the efficacy of CCM therapy on heart failure,[2][25] a large number of review articles (e.g.[3][15][16][26][27]) and at least two survey articles on device-based treatments of advanced heart failure[1][13] which address cardiac contractility modulation. Furthermore, there are more than 70 individual publications focusing specifically on CCM.[28]
Further randomized controlled trials studying the effect of CCM on the progression of heart failure have been initiated and are currently (as of Feb 2015) recruiting patients.[3][12][15]
Meta-analyses
Giallauria et al. evaluated the three randomized controlled trials (RCTs) currently available on CCM as a treatment for heart failure patients.[2] The three trials included a total of 641 patients and assessed the effect of CCM either in comparison to a sham treatment[22][23] or in comparison to the best medical treatment.[24] In contrast to an earlier meta-analysis by Kwong et al.[25] the study did not evaluate the data based on summarized results alone, but on the basis of the individual data sets of the 641 enrolled patients.
The study concluded that CCM significantly improved important markers of cardiac performance. These included the maximal oxygen uptake (peak VO2 or pVO2 – measured by ventilatory parameters during a cardiopulmonary exercise test), which is indicative of improved survival,[29] and the 6-minute walk test. The quality of life of participating patients, measured by the Minnesota Living with Heart Failure Questionnaire (MLWHFQ), also improved significantly. However, both meta-analyses demanded additional and larger randomized controlled trials in order to evaluate the effect of CCM more precisely.
Giallauria et al. describe the success of cardiac contractility modulation and the further potential of the therapy. Particular emphasis is given to the possibility that CCM therapy may close the therapeutic gap in heart failure treatment if previous study outcomes are confirmed.
Long-Term Survival Studies
As of February 2015, the effect of CCM therapy on the long-term mortality rates of heart failure patients has not been studied in a randomized controlled trial. Some preliminary single-center studies have been reported though.[10] Kuschyk et al. evaluated the long-term efficacy and survival of patients with CCM.[10] Their analysis included 81 patients with a disease severity of NYHA class II, III or IV and a mean follow-up of around 3 years. The analysis compared the observed mortality rate with the prediction of the Meta-analysis Global Group in Chronic Heart Failure (MAGGIC) model[30][31] which is based on the records of over 39,000 heart failure patients. Unlike a previous long-term outcome study of CCM,[32] this study was not limited by a widely heterogeneous group of patients.
Following long-term observation, the study concluded that CCM improved quality of life, exercise tolerance, NYHA class, left ventricular ejection fraction (LVEF) and brain natriuretic peptide (BNP) levels. Mortality rates were significantly lower than predicted at year 1, and lower than predicted but not statistically significant at year 3.
General
Heart failure is a chronic disease that usually progresses gradually.[18] The rate of progression and the degree of symptoms of the disease varies between different patients. CCM therapy aims to treat heart failure through a medium- to long-term treatment, over the course of weeks and months.
According to large implanting clinics, after the implantation wound is healed, the lifestyle of a patient is not restricted by the implanted device.[33] Leisure, travel (by car, train, ship or plane), hobbies and sex life will not be restricted. The patient may perceive an improved capacity for these activities and overall enhanced performance and exercise capacity in response to the actual therapy.
Contraindications
The most important contraindication in CCM treatment is permanent and long-standing persistent atrial fibrillation. The signal application in current CCM devices is timed and triggered according to the electrical activity of the atrium. In atrial fibrillation, electrical activity in the atrium is severely disturbed and is therefore not a reliable basis for the triggering of CCM signals. This also applies to other diseases involving severe disturbance in electrical atrial sensing.[34] Requests have been raised in scientific literature for an improved CCM algorithm which would allow CCM therapy to be delivered independently from any atrial signal. A pioneering study has already shown that an improved CCM algorithm could make CCM an effective treatment for patients with persistent atrial fibrillation.[34]
Other irregular rhythms, including frequent premature ventricular contractions (ventricular extra systoles) or a distinct signal transduction disorder in the heart (untreated AV block of more than 300 ms), may also represent contraindications. CRT treatment should be considered in lieu of CCM in patients with left bundle branch block (LBBB) and a QRS duration of over 120 ms, or when the QRS duration is greater than 150 ms and independent of LBBB.[9][18]
As with conventional pacemaker therapy, the CCM device cannot be implanted if the leads cannot be positioned appropriately in the heart. In cases where there is an artificial heart valve between the right atrium and ventricle (a mechanical prosthetic tricuspid valve), the valve function could be greatly affected by the ventricular leads. In some instances it may be impossible to guide the leads thorough the main veins in the upper half of the body to the heart due to venous thrombosis, for example VVI pacemakers, in the case of 100% stimulation, are also contraindicated.[9]
Side effects
The most frequently encountered adverse events related to CCM therapy are lead fracture or lead dislodgement.[24] Other reported complications include:
- Infection and bleeding at the IPG implantation site
- Accumulation of fluid in the pericardium (pericardial effusion)[23]
These side effects are similar to those that occur with other electrical stimulation therapies, such as pacemakers, CRT devices or ICD devices.[29] Furthermore, recorded complications did not differ between patients with activated CCM devices and patients with deactivated CCM devices.[15]
Overall, CCM treatment was demonstrated to have no negative impact on health markers.[15]
Precautions

Similarly to patients with other electrical stimulation devices, patients with a CCM device must follow certain precautions arising from the device implantation and its function.
- Electromagnetic fields: Strong electromagnetic fields can interfere with the function of the CCM device. Most interference will lead to inhibition of CCM signal delivery. Once away from the field, the CCM device will resume its normal function in most cases. The electromagnetic fields of household appliances are usually considered harmless.[35][36]
- Mobile phones: Similarly to other electrical stimulation devices, such as pacemakers, aside from a recommended safety distance of 10–15 cm (4-6 inches) between the CCM device and mobile phones, there are no restrictions on the use of mobile phones.[35]
- Security checks: Full body or hand-held metal detectors, such as those used at airport security controls, do not usually affect the function of the CCM device. However, where such detectors are used there are often signs warning people with cardiac pacemakers and defibrillators, and CCM patients are therefore advised to present their device ID. In these cases, the security check will typically continue with the use of a hand-held metal detector or by physical inspection.[35]
- Sports: All sports associated with increased stress on the arms or the chest, such as body building, martial arts or tennis, are usually not permitted. Diving is only permitted up to a depth of 5 meters due to the high pressure at greater depths.[33]
- Magnetic Resonance Imaging (MRI): Similarly to other electrical stimulation devices, such as pacemakers, CCM therapy is a contraindication for MRI, a medical imaging technique.[37]
Mechanism of action
The mechanism of action of CCM has been subject to continuous research since its initial discovery. Based on animal testing and experiments on human myocardial tissue obtained by biopsies, essential parts of the mechanism of action have been identified.[4][38] According to current understanding (as of February 2015), the mechanism of action of CCM may be summarized in the following manner: The CCM signals applied during the electrical non-excitatory state of the cardiac muscle cells (the absolute refractory period) cause an increase in myocyte calcium in the cytosol during systole. This increases the muscle contraction strength. Additionally, within minutes, cell metabolism and gene expression, which are typically abnormal in heart failure, improve towards their normal state.[38] This beneficial effect occurs initially only in the area adjacent to the electrodes, but with time also spreads to remote areas of the cardiac muscle.[38] CCM therefore restores the structure and function of damaged cells back towards their normal state. In some cases, disease-related changes in the ventricular heart structure can be partially reversed by CCM through a process known as reverse remodeling of the heart.[3][4][5][16][39][40]
Function
Composition
CCM devices are similar in structure to other implantable devices used for electrical stimulation of the heart, such as pacemakers or implantable cardioverter defibrillators (ICDs).[16] The currently available CCM system (as of February 2015) consists of four components, as described below.[16]

- Implantable Pulse Generator (IPG): The pulse generator generates the CCM’s non-excitatory electrical signals. The IPGs currently in use are similar in dimension to a matchbox, but have a slightly larger surface and are a little more slender (approx. 6.5 cm x 4.7 cm x 1.2 cm or approx. 2 9/16" x 1 7/8" x 1/2"). The IPG is usually implanted in the chest subcutaneously (under the skin), below the right clavicle of the patient. In some cases, the IPG remains noticeable as a slight bulge under the skin. Pulse generators combining CCM therapy with the functionality of other electrical stimulation devices such as pacemakers or ICDs are not currently available, although the development of such a combined device has already been suggested in literature.[13]
- Leads: Currently available CCM delivery devices use three standard (commercially available) pacemaker leads. These leads are special medical wires that conduct the electrical signals between the pulse generator and the heart. During implantation, the leads are inserted into the subclavian vein below the clavicle or, less often, the cephalic vein or axillary vein. The leads are then advanced through the superior vena cava to their position in the right atrium or right ventricle. The lead in the right atrium detects atrial electric signals and transmits them to the pulse generator. The IPG processes the atrial signal and generates the CCM signals which are transmitted to the right ventricle via two ventricular leads. The ventricular leads are positioned in the upper and middle region of the septum that separates the right ventricle from the left ventricle (interventricular septum). The leads themselves do not cause a change in the blood flow to the heart.
- Battery charger: The battery charger ensures the power supply of the implantable pulse generator (IPG). Currently available battery chargers are used externally and are portable, allowing the patient to move freely while charging. The battery of the IPG can be charged wirelessly through the skin, without contact, since the charger operates by electromagnetic induction. Charging is carried out independently at home by the patient after having received the necessary briefing. One load cycle supplies the IPG with energy for about a week. This differs from conventional pacemaker and ICD devices which usually do not have a battery charging function and need to be surgically replaced prior to battery depletion.
- Programming unit: The programming unit is used solely by the doctor for device check-ups or in case of technical problems. The stimulation signal of the pulse generator can be adjusted to the needs of each patient through the programming unit. For example, the programmer may be used to adjust the signal intensity and duration of the daily CCM application. The IPG can be programmed wirelessly through the skin by induction.
CCM signals

Cardiac contractility modulation (CCM) acts on the cardiac muscle during the absolute refractory period via specific electrical signals generated by the pulse generator. Signals are applied approximately 30 ms after onset of the QRS complex (normal total QRS duration: ≤ 120 ms). The signal consists of two bi-phasic pulses with an amplitude of ± 7.7 V and with a total signal duration of about 20 ms.[3][13]
Since CCM signals are delivered during the absolute refractory period of the cardiac cycle, they neither trigger muscle contractions nor cause activation of additional muscle fibers. Accordingly, the heart’s electrical and mechanical activation sequence remains unchanged. As CCM signals contain around 50-100 times more energy than signals from conventional pacemakers, their peaks can easily be recognized in an electrocardiogram (ECG).[3][13]
Implantation
The implantation of the pulse generator (IPG) and the corresponding CCM delivery leads is comparable to a pacemaker implantation. This sort of intervention is carried out approximately one million times per year worldwide.[41] The implantation procedure is minimally invasive, lasts roughly 40 minutes and is usually carried out under local anesthesia. However, patients should fast ahead of the implantation due to possible complications which may result in a longer procedure and/or require longer anesthesia.[16]
First, the doctor checks the function of the pulse generator and the leads, before positioning the leads in the heart. The positioning of the leads is verified by X-ray imaging and by the measurement of voltage and electric current through the leads (lead impedance).[16]
Following successful positioning, the leads are connected to the pulse generator. A pocket is formed under the skin or chest muscle below the clavicle of the patient in order to implant the pulse generator. The IPG is inserted in the pocket and its function is tested. If the patient happens to have a pacemaker or implantable cardioverter defibrillator, the doctor and/or a trained technician ensures that there is no interference between the two devices by performing a “crosstalk check”. Finally, the pocket is sutured and the wound is bandaged.
Following implantation, patients are usually monitored for a period of time to ensure that the CCM device functions properly before being discharged from hospital.[16] Once the healing process is complete, there is no need for any precautionary measures concerning water contact with the device as it is completely under the skin. It is not problematic for patients to shower or swim with the device, providing their health condition permits these activities.[33]
After discharge, treatment is continued under the care of an outpatient cardiologist. Check-ups are carried out after a few days, after a few weeks and then following the treating cardiologist’s recommendation.[16]
Maintenance

Aside from periodic battery charging (charging takes approximately 1 hour per week[26]) and the surgical replacement needed after expiration of its battery life, CCM devices are maintenance-free. Nevertheless, the settings and function of the system must be checked and may be adjusted by a cardiologist from time to time.[26] Battery chargers are equipped with a patient alert system which warns the patient to contact a physician in case of device malfunction or other functional abnormalities, such as low therapy delivery.[42]
Interactions with other electrical stimulation treatments
Adverse interactions between CCM therapy and other electrical stimulation therapies have not been observed to date. Studies have shown that CCM therapy can be carried out simultaneously with a pacemaker and/or CRT treatment, and with or without an implantable cardioverter defibrillator (ICD), without causing disturbance to the individual therapies.[3] As a result of these findings, the development of devices combining CCM and cardioverter defibrillation has been requested by some physicians in order to spare patients from the need for additional separate electrical stimulation devices and implantation procedures.[3][13]
Referral and Reimbursement
CCM treatment is usually recommended by a cardiologist and the device may be implanted by a cardiac electrophysiologist. The treatment cost is covered both by statutory as well as private health insurance in Germany, Switzerland, Italy and Austria.[42] The appropriate comparator for CCM therapy is failed Optimal Medical Therapy (OMT).[43]
History
Development of cardiac contractility modulation began in the late 1990s.[44][45] Studies on individual cardiac muscle cells using a patch-clamp technique had already shown, in 1969, that a voltage applied during the absolute refractory period through leads between the interior of the cell and its outside environment increased the calcium influx through the cell membrane and improved the contraction of cardiac muscle cells.[46][47] In 2001, scientists observed that a similar effect occurs even if the voltage is applied exclusively outside the cardiac muscle cells.[48] Additionally, it was observed that therapeutically useful effects on the cardiac muscle were achieved if the electrical signals were applied not only to single cells but to large areas using larger leads, as used in conventional cardiac pacemakers. The contractility of both a healthy heart and a damaged heart could be increased through application of appropriate signals during the absolute refractory period of the cardiac muscle cells.[48][49]
An implantable CCM device was received by a patient for the first time in 2001.[50][51] The first study on the therapeutic effects of CCM in humans was presented in 2004.[52] To date, more than 2,000 heart failure patients have been treated with CCM worldwide,[11] including 641 patients under the study conditions recommended by the Cochrane Collaboration as being necessary for inclusion in a meta-analysis.[2]
Research
CCM technology does not only affect the function of cardiac tissue, but can also be used to affect the function of other muscle tissue. Approval has already been given for clinical use of the technology in treatment of the stomach to support weight loss and better control of sugar metabolism in obese patients with diabetes mellitus type 2.[53]
See also
- Heart
- Cardiac cycle
- Heart failure
- Artificial cardiac pacemaker
- Implantable cardioverter-defibrillator
- NYHA classification
- Cardiac resynchronization therapy
External links
References
- 1 2 3 4 5 6 7 Abraham, W.T.; S.A. Smith (Feb 2013). "Devices in the management of advanced, chronic heart failure" (PDF). Nat Rev Cardiol. 10 (2): 98–110. doi:10.1038/nrcardio.2012.178. PMC 3753073
 . PMID 23229137. Retrieved Oct 10, 2014.
. PMID 23229137. Retrieved Oct 10, 2014. - 1 2 3 4 5 6 7 8 9 10 11 12 Giallauria, F.; et al. (Aug 2014). "Effects of cardiac contractility modulation by non-excitatory electrical stimulation on exercise capacity and quality of life: an individual patient's data meta-analysis of randomized controlled trials". Int J Cardiol. 175 (2): 352–357. doi:10.1016/j.ijcard.2014.06.005. PMID 24975782.
- 1 2 3 4 5 6 7 8 9 10 11 12 Borggrefe, M.; D. Burkhoff (Jul 2012). "Clinical effects of cardiac contractility modulation (CCM) as a treatment for chronic heart failure". Eur J Heart Fail. 14 (7): 703–712. doi:10.1093/eurjhf/hfs078. PMID 22696514.
- 1 2 3 Butter, C.; et al. (May 2008). "Cardiac Contractility Modulation Electrical Signals Improve Myocardial Gene Expression in Patients With Heart Failure" (PDF). J Am Coll Cardiol. 51 (18): 1784–1789. doi:10.1016/j.jacc.2008.01.036. PMID 18452785. Retrieved Oct 9, 2014.
- 1 2 Yu, C.M.; et al. (Dec 2009). "Impact of cardiac contractility modulation on left ventricular global and regional function and remodeling" (PDF). JACC Cardiovasc Imaging. 2 (12): 1341–1349. doi:10.1016/j.jcmg.2009.07.011. PMID 20083066. Retrieved Oct 10, 2014.
- ↑ Marcus, Melvin L. (1983). The Coronary Circulation in Health and Disease. McGraw Hill. ISBN 978-0070402935.
- ↑ Butter, C.; et al. (Mar 2007). "Enhanced inotropic state of the failing left ventricle by cardiac contractility modulation electrical signals is not associated with increased myocardial oxygen consumption". J Card Fail. 13 (2): 137–142. doi:10.1016/j.cardfail.2006.11.004. PMID 17395055.
- ↑ Goliasch, G.; et al. (Mar 2012). "The effect of device-based cardiac contractility modulation therapy on myocardial efficiency and oxidative metabolism in patients with heart failure". Eur J Nucl Med Mol Imaging. 39 (3): 408–415. doi:10.1007/s00259-011-1977-8. PMID 22083298.
- 1 2 3 4 Tönnis, T.; Kuck, K.-H. (Oct 2011). "Therapie der chronischen Herzinsuffizienz durch kardiale Kontraktionsmodulation (CCM) Möglichkeiten und Studienübersicht". Herz. 36 (7): 600–607. doi:10.1007/s00059-011-3510-z. PMID 21912910.
- 1 2 3 Kuschyk, J.; et al. (Jan 2015). "Efficacy and survival in patients with cardiac contractility modulation: Long-term single center experience in 81 patients". Int J Cardiol. 20 (183C): 76–81. doi:10.1016/j.ijcard.2014.12.178. PMID 25662055.
- 1 2 3 Kuschyk, J. (2014). "Der Besondere Stellenwert der Kardialen Kontraktilitätsmodulation in der Devicetherapie". Herzmedizin. Retrieved Jun 6, 2014.
- 1 2 3 clinicaltrials.gov Announcement of a study that will further investigate safety and efficacy of CCM devices
- 1 2 3 4 5 6 7 8 9 10 Kuck, K.-H.; et al. (Jan 2014). "New devices in heart failure: an European Heart Rhythm Association report: developed by the European Heart Rhythm Association; endorsed by the Heart Failure Association" (PDF). Europace. 16 (1): 109–128. doi:10.1093/europace/eut311. PMID 24265466. Retrieved Oct 13, 2014.
- ↑ Abraham, W.T.; et al. (Sep 2011). "Subgroup Analysis of a Randomized Controlled Trial Evaluating the Safety and Efficacy of Cardiac Contractility Modulation in Advanced Heart Failure". J Card Fail. 17 (9): 710–717. doi:10.1016/j.cardfail.2011.05.006. PMID 21872139.
- 1 2 3 4 5 6 7 8 9 10 Burkhoff, D. (Dec 2011). "Does Contractility Modulation Have a Role in the Treatment of Heart Failure?". Curr Heart Fail Rep. 8 (4): 260–265. doi:10.1007/s11897-011-0067-3. PMID 21656201.
- 1 2 3 4 5 6 7 8 9 Butter, C. (Mar 2011). "Verbesserung der linksventrikulären Kontraktilität durch Stimulation in der absoluten Refraktärperiode. Kardiale Kontraktilitätsmodulation.". Herzschr Elektrophys. 22 (1): 27–33. doi:10.1007/s00399-011-0120-7. PMID 21365468.
- ↑ Nagele, H.; S. Behrens; C. Eisermann (Dec 2008). "Cardiac contractility modulation in non-responders to cardiac resynchronization therapy" (PDF). Europace. 10 (12): 1375–1380. doi:10.1093/europace/eun257. PMID 18776196. Retrieved Oct 11, 2014.
- 1 2 3 4 5 McMurray, J.J.V.; et al. (2012). "ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012" (PDF). European Heart Journal. 33 (14): 1787–1847. doi:10.1093/eurheartj/ehs104. PMID 22611136. Retrieved Oct 10, 2014.
- ↑ Röger, S.; et al. (Aug 2014). "Long term impact of cardiac contractility modulation on QRS duration". J Electrocardiol. 47: 936–40. doi:10.1016/j.jelectrocard.2014.08.011. PMID 25201417.
- ↑ ESC National Cardiac Societies endorsing ESC guidelines on the Website of the ESC Archived April 25, 2013, at the Wayback Machine.
- ↑ Coats, A.J.S.; L.G. Shewan (Oct 2013). "Inconsistencies in the development of the ESC Clinical Practice Guidelines for Heart Failure". Int J Cardiol. 168 (3): 1724–1727. doi:10.1016/j.ijcard.2013.05.045. PMID 23735338.
- 1 2 Neelagaru, S.B.; et al. (Oct 2006). "Nonexcitatory, cardiac contractility modulation electrical impulses: Feasibility study for advanced heart failure in patients with normal QRS duration". Heart Rhythm. 3 (10): 1140–1147. doi:10.1016/j.hrthm.2006.06.031. PMID 17018340.
- 1 2 3 Borggrefe, M.; et al. (Apr 2008). "Randomized, double blind study of non-excitatory, cardiac contractility modulation electrical impulses for symptomatic heart failure" (PDF). Eur Heart J. 29 (8): 1019–1028. doi:10.1093/eurheartj/ehn020. PMID 18270213. Retrieved Oct 16, 2014.
- 1 2 3 Kadish, A.; et al. (Feb 2011). "A randomized controlled trial evaluating the safety and efficacy of cardiac contractility modulation in advanced heart failure". Am Heart J. 161 (2): 329–337. doi:10.1016/j.ahj.2010.10.025. PMID 21315216.
- 1 2 Kwong, J.S.; J.E. Sanderson; C.M. Yu (Sep 2012). "Cardiac contractility modulation for heart failure: a meta-analysis of randomized controlled trials". Pacing Clin Electrophysiol. 35 (5): 1111–1118. doi:10.1111/j.1540-8159.2012.03449.x. PMID 22734676.
- 1 2 3 Kuschyk, J.; S. Röger; M. Borggrefe (Oct 2014). "Kardiale Kontraktilitätsmodulation zur Behandlung der symptomatischen Herzinsuffizienz". Der Kardiologe. 8 (5): 407–414. doi:10.1007/s12181-014-0595-7. Retrieved Dec 1, 2014.
- ↑ Kuschyk, J.; M. Borggrefe (2013). "Elektrische Therapie der Herzinsuffizienz". Kardio up. 9 (1): 37–56. doi:10.1055/s-0032-1326192. Retrieved Nov 6, 2014.
- ↑ Research of the Pubmed data base for the search term "Cardiac Contractility Modulation" in the title of publications performed on Oct 16, 2014
- 1 2 Pakarinen, S.; L. Oikarinen; L. Toivonen (Jan 2010). "Short-term implantation-related complications of cardiac rhythm management device therapy: a retrospective single-centre 1-year survey" (PDF). Europace. 12 (1): 103–108. doi:10.1093/europace/eup361. PMID 19914920. Retrieved Nov 6, 2014.
- ↑ Pocock, S.J.; et al. (May 2013). "Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies". Eur Heart J. 34 (19): 1404–1413. doi:10.1093/eurheartj/ehs337. PMID 23095984. Retrieved Feb 20, 2015.
- ↑ "MAGGIC" Heart Failure Risc Calculator according to Pocock et al. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies, Eur Heart J (2013) 34(19) 1404-1413 (linked above)
- ↑ Schau, T.; et al. (Apr 2011). "Long-term outcome of cardiac contractility modulation in patients with severe congestive heart failure" (PDF). Europace. 13 (10): 1436–1444. doi:10.1093/europace/eur153. PMID 21712286. Retrieved Feb 20, 2015.
- 1 2 3 Tips by the American Heart Associuation "Living With Your Pacemaker"
- 1 2 Röger, S.; et al. (Apr 2014). "Cardiac contractility modulation: first experience in heart failure patients with reduced ejection fraction and permanent atrial fibrillation". Europace. 16: 1205–9. doi:10.1093/europace/euu050. PMID 24706089.
- 1 2 3 Safety recommendations of the American Heart Association for patients with artificial pacemakers
- ↑ Safety recommendations of the American Heart Association for patients with implantable cardioverter defibrillators (ICDs)
- ↑ Dill, T. (Jul 2008). "Contraindications to magnetic resonance imaging" (PDF). Heart. 94 (7): 943–948. doi:10.1136/hrt.2007.125039. PMID 18552230. Retrieved Feb 22, 2015.
- 1 2 3 Lyon, A.R.; M.A. Samara; D.S. Feldman (Oct 2013). "Cardiac contractility modulation therapy in advanced systolic heart failure". Nat. Rev. Cardiol. 10 (10): 584–598. doi:10.1038/nrcardio.2013.114. PMID 23939481.
- ↑ Imai, M.; et al. (May 2007). "Therapy with cardiac contractility modulation electrical signals improves left ventricular function and remodeling in dogs with chronic heart failure" (PDF). J Am Coll Cardiol. 49 (21): 2120–2128. doi:10.1016/j.jacc.2006.10.082. PMID 17531662. Retrieved Oct 11, 2014.
- ↑ Gupta, R.C.; et al. (Feb 2009). "Cardiac Contractility Modulation Electrical Signals Normalize Activity, Expression, and Phosphorylation of the Na+-Ca2+ Exchanger in Heart Failure". Journal of Cardiac Failure. 15 (1): 48–56. doi:10.1016/j.cardfail.2008.08.011. PMID 19181294.
- ↑ Mond, H.G.; Proclemer, A. (Aug 2011). "The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia's project.". Pacing Clin Electrophysiol. 34 (8): 1013–1027. doi:10.1111/j.1540-8159.2011.03150.x. PMID 21707667.
- 1 2 Announcement of the launch of the OPTIMIZER IVs CCM device on Implantable-Device.com
- ↑ CCM device application draft
- ↑ Patent for CCM: Apparatus and method for controlling the delivery of contractility modulating non-excitatory signals to the heart
- ↑ Mohri, S.; et al. (May 2002). "Cardiac contractility modulation by electric currents applied during the refractory period" (PDF). Am J Physiol Heart Circ Physiol. 282 (5): H1642–H1647. doi:10.1152/ajpheart.00959.2001. PMID 11959626. Retrieved Oct 9, 2014.
- ↑ Antoni, H.; R. Jacob; R. Kaufmann (1969). "Mechanical response of the frog and mammalian myocardium to changes in the action potential duration by constant current pulses". Pflugers Arch. 306 (1): 33–57. PMID 4975967.
- ↑ Wood, E.H.; R.L. Heppner; S. Weidmann (Mar 1969). "Inotropic effects of electric currents. I. Positive and negative effects of constant electric currents or current pulses applied during cardiac action potentials. II. Hypotheses: calcium movements, excitation-contraction coupling and inotropic effects.". Circ Res. 24 (3): 409–445. doi:10.1161/01.RES.24.3.409. PMID 5766519. Retrieved Oct 9, 2014.
- 1 2 Burkhoff, D.; et al. (Jan 2001). "Electric currents applied during the refractory period can modulate cardiac contractility in vitro and in vivo". Heart Fail Rev. 6 (1): 27–34. PMID 11248765.
- ↑ Sabbah, H.N.; et al. (Jan 2001). "Cardiac contractility modulation with the impulse dynamics signal: studies in dogs with chronic heart failure". Heart Fail Rev. 6 (1): 45–53. PMID 11248767.
- ↑ Pappone, C.; et al. (Jan 2001). "Electrical modulation of cardiac contractility: clinical aspects in congestive heart failure". Heart Fail Rev. 6 (1): 55–60. PMID 11248768.
- ↑ Pappone, C.; et al. (Dec 2002). "Cardiac contractility modulation by electric currents applied during the refractory period in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy". Am J Cardiol. 90 (12): 1307–1313. doi:10.1016/s0002-9149(02)02868-0. PMID 12480039.
- ↑ Stix, G.; et al. (Apr 2014). "Chronic electrical stimulation during the absolute refractory period of the myocardium improves severe heart failure" (PDF). Eur Heart J. 25 (8): 650–655. doi:10.1016/j.ehj.2004.02.027. PMID 15084369. Retrieved Oct 10, 2014.
- ↑ Bohdjalian, A.; et al. (Sep 2009). "Improvement in glycemic control by gastric electrical stimulation (TANTALUS) in overweight subjects with type 2 diabetes". Surg Endosc. 23 (9): 1955–1960. doi:10.1007/s00464-008-0222-4. PMID 19067068.