Airway management
| Airway management | |
|---|---|
| Intervention | |
|
Photograph of an anesthesiologist using the Glidescope video laryngoscope to intubate the trachea of a morbidly obese elderly person with challenging airway anatomy | |
| MeSH | D058109 |
Airway management includes a set of maneuvers and medical procedures performed to both prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere.[1] This is accomplished by either clearing a previously obstructed airway, which can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration), or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation.
Airway management is commonly divided into two categories: basic and advanced.
Basic techniques are generally non-invasive and do not require specialized medical equipment or advanced training. These include head maneuvers to optimize ventilation, abdominal thrusts, and back blows.
Advanced techniques require specialized medical training and equipment, and are further categorized anatomically into supraglottic devices (such as oropharyngeal and nasopharyngeal airways), infraglottic techniques (such as tracheal intubation), and surgical methods (such as cricothyrotomy).[2]
Airway management is a primary consideration in cardiopulmonary resuscitation, anaesthesia, emergency medicine, intensive care medicine, and first aid. It represents the "A" In the ABC treatment mnemonic.[3]
Basic airway management
Basic airway management is mainly used in first aid since it is non-invasive, simple to perform and unlike advanced airway management does not rely on the use of medical equipment. Basic airways management can be divided into treatment and prevention.
Treatment

Treatment includes a number of procedures aiming at removing foreign bodies from the airways. Most modern protocols, including those of the American Heart Association, American Red Cross and the European Resuscitation Council,[4] recommend several stages, designed to apply increasingly more pressure. Basic treatment includes a number of procedures aiming at removing foreign bodies from the airways. Most protocols recommend encouraging the victim to cough, followed by hard back slaps and if none of these things work; abdominal thrusts (Heimlich maneuver) or chest thrusts. Some guidelines recommend alternating between abdominal thrusts and back slaps.[4]
The American Medical Association advocates sweeping the fingers across the back of the throat to attempt to dislodge airway obstructions, once the choking victim becomes unconscious.[5] However, many modern protocols recommend against the use of the finger sweep since, if the patient is conscious, they will be able to remove the foreign object themselves, or if they are unconscious, the rescuer should simply place them in the recovery position as this allows (to a certain extent) the drainage of fluids out of the mouth instead of down the trachea due to gravity. There is also a risk of causing further damage (for instance inducing vomiting) by using a finger sweep technique.

Multiple evidence suggest, that one of promising approaches for self treatment during choking could be by applying the head-down (inversed) position[6]
Prevention

Prevention techniques focuses on preventing the tongue from falling back and obstructing the airways, such as head-tilt/chin-lift and jaw-thrust maneuvers, while use of the recovery position mainly prevents aspiration of things like stomach content or blood. If head-tilt chin-lift and jaw-thrust maneuvers are performed with any objects in the airways it may dislodge them further down the airways and thereby cause more blockage and harder removal.
The head-tilt/chin-lift is the primary maneuver used in any patient in whom cervical spine injury is not a concern. The simplest way of ensuring an open airway in an unconscious patient is to use a head-tilt/chin-lift technique, thereby lifting the tongue from the back of the throat. This is taught on most first aid courses as the standard way of clearing an airway.
The jaw-thrust maneuver is an effective airway technique, particularly in the patient in whom cervical spine injury is a concern. The jaw thrust is a technique used on patients with a suspected spinal injury and is used on a supine patient. The practitioner uses their index and middle fingers to physically push the posterior (back) aspects of the mandible upwards while their thumbs push down on the chin to open the mouth. When the mandible is displaced forward, it pulls the tongue forward and prevents it from occluding the entrance to the trachea.

The recovery position refers to one of a series of variations on a lateral recumbent or three-quarters prone position of the body, in to which an unconscious but breathing casualty can be placed. Use of the recovery position prevents aspiration.
Most airway maneuvers are associated with some movement of the cervical spine.[7][8] Even though collars for holding the head in-line can cause problems maintaining an airway and maintaining a blood pressure,[9] it is unrecommended to remove the collar without adequate personnel to manually hold the head in place.[10]
Advanced airway management
Unlike basic airway management such as head-tilt or jaw-thrust maneuver, advanced airway management relies on the use of medical equipment. Advanced airway management can be performed "blind" or with visualization of the glottis e.g. by the use of a laryngoscope. It is frequently performed in critically injured, ill or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.
In roughly increasing order of invasiveness are the use of supraglottic devices such as oropharyngeal or nasopharyngeal airways, followed by infraglottic techniques such as tracheal intubation and finally surgical methods
Removal of foreign objects

The ingestion and aspiration of foreign objects poses a common and dangerous problem in young children. It remains one of the leading cause of death in children under the age of 5.[11] Common food items (baby carrots, peanuts, etc.) and household objects (coins, metals, etc.) may lodge in various levels of the airway tract and cause significant obstruction of the airway. Complete obstruction of the airway represents a medical emergency. During such crisis, caretakers may attempt back blows, abdominal thrust, or the Heimlich maneuver to dislodge the inhaled object and reestablish airflow into the lungs.[12]
In the hospital setting, healthcare practitioners will make the diagnosis of foreign body aspiration from the medical history and physical exam findings. In some cases, providers will order chest radiographs, which may show signs of air-trapping in the affected lung. In advanced airway management, the inhaled foreign objects, however, are either removed by blind suction or under direct inspection of the airway with a laryngoscope or bronchoscope. If removal is not possible, other surgical methods should be considered.[13]
Supraglottic techniques
Supraglottic techniques includes the use of supraglottic tubes, such as oropharyngeal (OPA) and Nasopharyngeal airways (NPA), and supraglottic devices such as laryngeal masks. Common for all supraglottic devices are that they are introduced into the pharynx, ensuring the upper respiratory tract remains open, without passing through the glottis and thereby entering the trachea.
A nasopharyngeal airway is a soft rubber or plastic hollow tube that is passed through the nose into the posterior pharynx. Patients tolerate NPAs more easily than OPAs, so NPAs can be used when the use of an OPA is difficult, such as when the patient's jaw is clenched or the patient is semiconscious and cannot tolerate an OPA.[14] NPAs are generally not recommended if there is suspicion of a fracture to the base of the skull, due to the possibility of the tube entering the cranium.[15] However, the actual risks of this complication occurring compared to the risks of damage from hypoxia if an airway is not used are debatable.[15][16]

Oropharyngeal airways are rigid plastic curved devices, which are inserted through the patient's mouth. They prevent the patient's tongue from covering the epiglottis and thereby obstructing the airway. An oropharyngeal airway should only be used in a deeply unresponsive patient because in a responsive patient they can cause vomiting and aspiration by stimulating the gag reflex.[17]
Supraglottic airways (or extraglottic devices[18]) are a family of devices that are inserted through the mouth to sit on top of the larynx. Supraglottic airways are used in the majority of operations performed under general anaesthesia.[19] Compared to a cuffed tracheal tube (see below), they give less protection against aspiration but are easier to insert and cause less laryngeal trauma.[18] The best-known example is the Laryngeal Mask Airway or LMA™. A laryngeal mask airway is an airway placed into the mouth and set over the glottis and inflated.[20] Other variations include devices with oesophageal access ports, so that a separate tube can be inserted from the mouth to the stomach to decompress accumulated gases and drain liquid contents.[18] Some devices can have an endotracheal tube passed through them into the trachea.[18]
Infraglottic techniques

Unlike supraglottic devices; infraglottic devices pass through the glottis and thereby enter the trachea. Tracheal intubation, often simply referred to as intubation, is the placement of a flexible plastic or rubber tube into the trachea to maintain an open airway or to serve as a conduit through which to administer certain drugs. The most widely used route is orotracheal, in which an endotracheal tube is passed through the mouth and vocal apparatus into the trachea. In a nasotracheal procedure, an endotracheal tube is passed through the nose and vocal apparatus into the trachea.Alternatives to standard endotracheal tubes includes laryngeal tube and combitube.
Surgical methods
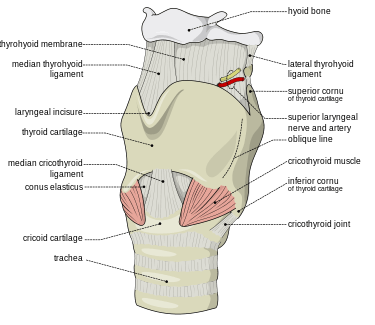
Surgical methods for airway management rely on making a surgical incision below the glottis in order to achieve direct access to the lower respiratory tract, bypassing the upper respiratory tract. Surgical airway management is often performed as a last resort in cases where orotracheal and nasotracheal intubation are impossible or contraindicated. Surgical airway management is also used when a person will need a mechanical ventilator for a longer period. Surgical methods for airway management include cricothyrotomy and tracheostomy.
A cricothyrotomy is an incision made through the skin and cricothyroid membrane to establish a patent airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or massive facial trauma.[21] A cricothyrotomy is nearly always performed as a last resort in cases where orotracheal and nasotracheal intubation are impossible or contraindicated. Cricothyrotomy is easier and quicker to perform than tracheotomy, does not require manipulation of the cervical spine and is associated with fewer immediate complications.[22]
A tracheotomy is a surgically created opening from the skin of the neck down to the trachea.[23] A tracheotomy may be considered where a person will need to be on a mechanical ventilator for a longer period.[23] The advantages of a tracheotomy include less risk of infection and damage to the trachea during the immediate post-surgical period.[23] Although rare, some long term complications of tracheotomies include tracheal stenosis and tracheoinnominate fistulas.[24]
Airway management in specific situations
Cardiopulmonary resuscitation
The optimal method of airway management during CPR is not well established at this time given that the majority of studies on the topic are observational in nature. These studies, however, guide current recommendations until prospective, randomized controlled trials are conducted.
Current studies suggest that for out-of-hospital cardiac arrest, basic airway interventions (head-tilt–chin-lift maneuvers, with bag-valve-mask only or mouth-to-mouth ventilations, with or without nasopharyngeal and/or oropharyngeal airways) resulted in greater short-term and long-term survival, as well as improved neurological outcomes in comparison to advanced airway interventions (endotracheal intubation, laryngeal mask airway, all types of supraglottic airways (SGA), and trans-tracheal or trans-cricothyroid membrane airways).[25][26] Given that these are observational studies, caution must be given to the possibility of confounding by indication. That is, patients requiring an advanced airway may have had a poorer prognosis in relation to those requiring basic interventions to begin with.
For the management of in-hospital cardiac arrest however, studies currently support the establishment of an advanced airway. It is well documented that quality chest compressions with minimal interruption result in improved survival.[27] This is suggested to be due, in part, to decreased no-flow-time in which vital organs, including the heart are not adequately perfused. Establishment of an advanced airway (endotracheal tube, laryngeal mask airway) allows for asynchronous ventilation, reducing the no-flow ratio, as compared to the basic airway (bag-valve mask) for which compressions must be paused to adequately ventilate the patient.[28]
Bystanders without medical training who see an individual suddenly collapse should call for help and begin chest compressions immediately. The American Heart Association currently supports "Hands-only"™ CPR, which advocates chest compressions without rescue breaths for teens or adults.[29] This is to minimize the reluctance to start CPR due to concern for having to provide mouth-to-mouth resuscitation.
Trauma
In prehospital environments, airway management is controversial, with intubation and supraglottic airways each having advantages and disadvantages. Trauma victims are often not fasting so there is an increased risk of aspiration, but blood and other material may make it difficult to see the larynx to intubate.[18]
References
- ↑ Bingham, Robert M.; Proctor, Lester T. (2008-08-01). "Airway management". Pediatric Clinics of North America. 55 (4): 873–886, ix–x. doi:10.1016/j.pcl.2008.04.004. ISSN 0031-3955. PMID 18675024.
- ↑ Tintinalli, Judith (2016). Tintinalli's Emergency Medicine: A Comprehensive Study Guide. McGraw Hill. pp. 178–198. ISBN 978-0-07-180913-9
- ↑ Wright, Pearce (2003-08-13). "Obituary: Peter Safar". London: The Guardian. Retrieved 2014-12-06
- 1 2 Nolan, JP; Soar, J; Zideman, DA; Biarent, D; Bossaert, LL; Deakin, C; Koster, RW; Wyllie, J; Böttiger, B; ERC Guidelines Writing Group. "European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary". Resuscitation. 81 (10): 1226. doi:10.1016/j.resuscitation.2010.08.021. PMID 20956052.
- ↑ American Medical Association (2009-05-05). American Medical Association Handbook of First Aid and Emergency Care. Random House. ISBN 978-1-4000-0712-7.
- ↑ Luczak (2016.02.015). "Head-down self-treatment of choking". Resuscitation. doi:10.1016/j.resuscitation.2016.02.015. Check date values in:
|date=(help) - ↑ Donaldson WF, Heil BV, Donaldson VP, Silvaggio VJ (1997). "The effect of airway maneuvers on the unstable C1-C2 segment. A cadaver study.". Spine (Phila Pa 1976). 22 (11): 1215–8. doi:10.1097/00007632-199706010-00008. PMID 9201858.
- ↑ Brimacombe J, Keller C, Künzel KH, Gaber O, Boehler M, Pühringer F (2000). "Cervical spine motion during airway management: a cinefluoroscopic study of the posteriorly destabilized third cervical vertebrae in human cadavers". Anesth Analg. 91 (5): 1274–8. doi:10.1213/00000539-200011000-00041. PMID 11049921.
- ↑ Kolb JC, Summers RL, Galli RL (1999). "Cervical collar-induced changes in intracranial pressure". Am J Emerg Med. 17 (2): 135–7. doi:10.1016/S0735-6757(99)90044-X. PMID 10102310.
- ↑ Mobbs RJ, Stoodley MA, Fuller J (2002). "Effect of cervical hard collar on intracranial pressure after head injury". ANZ J Surg. 72 (6): 389–91. doi:10.1046/j.1445-2197.2002.02462.x. PMID 12121154.
- ↑ "National Safety Council Accident Facts.". February 2000.
- ↑ Manning PB, Wesley JR, Polley TZ, et al. Esophageal and tracheobronchial foreign bodies in infants and children. Pediatr Surg Int 1987;2:346.
- ↑ TONY CAPIZZANI, RONALD B. HIRSCHL, ROBERT E. CILLEY (2011). Greenfield's Surgery: Scientific Principles and Practice, 5e. Lippincott Williams & Wilkins. pp. Chapter 2016 (Pediatric Chest).
- ↑ Roberts K, Whalley H, Bleetman A (2005). "The nasopharyngeal airway: dispelling myths and establishing the facts". Emerg Med J. 22 (6): 394–6. doi:10.1136/emj.2004.021402. PMC 1726817
 . PMID 15911941.
. PMID 15911941. - 1 2 Ellis, D. Y. (2006). "Intracranial placement of nasopharyngeal airways: Is it all that rare?". Emergency Medicine Journal. 23 (8): 661–661. doi:10.1136/emj.2006.036541.
- ↑ Roberts, K.; Whalley, H.; Bleetman, A. (2005). "The nasopharyngeal airway: Dispelling myths and establishing the facts". Emergency Medicine Journal. 22 (6): 394–396. doi:10.1136/emj.2004.021402. PMC 1726817
 . PMID 15911941.
. PMID 15911941. - ↑ "Guedel airway". AnaesthesiaUK. 14 May 2010. Retrieved 23 May 2013.
- 1 2 3 4 5 Hernandez, MR; Klock, A; Ovassapian, A (2011). "Evolution of the Extraglottic Airway: A Review of Its History, Applications, and Practical Tips for Success". Anesthesia and Analgesia. 114 (2): 349–68. doi:10.1213/ANE.0b013e31823b6748. PMID 22178627.
- ↑ Cook, T; Howes, B. (2010). "Supraglottic airway devices: recent advances". Continuing Education in Anaesthesia, Critical Care and Pain. 11 (2): 56. doi:10.1093/bjaceaccp/mkq058.
- ↑ Davies PR, Tighe SQ, Greenslade GL, Evans GH (1990). "Laryngeal mask airway and tracheal tube insertion by unskilled personnel". The Lancet. 336 (8721): 977–979. doi:10.1016/0140-6736(90)92429-L. PMID 1978159. Retrieved 25 July 2010.
- ↑ Mohan, R; Iyer, R; Thaller, S (2009). "Airway management in patients with facial trauma". Journal of Craniofacial Surgery. 20 (1): 21–3. doi:10.1097/SCS.0b013e318190327a. PMID 19164982.
- ↑ Katos, MG; Goldenberg, D (2007). "Emergency cricothyrotomy". Operative Techniques in Otolaryngology. 18 (2): 110–4. doi:10.1016/j.otot.2007.05.002.
- 1 2 3 Gomes Silva, B. N.; Andriolo, R. G. B.; Saconato, H.; Atallah, Á. N.; Valente, O. (2012). Gomes Silva, Brenda Nazaré, ed. "Early versus late tracheostomy for critically ill patients". The Cochrane Library. doi:10.1002/14651858.CD007271.pub2.
- ↑ REDDY, RISHINDRA M. (2011). Greenfield's Surgery: Scientific Principles and Practice, 5e. Lippincott Williams & Wilkins. pp. Chapter 80. CHEST WALL, PLEURA, MEDIASTINUM, AND NONNEOPLASTIC LUNG DISEASE.
- ↑ Fouche, Pieter F.; Simpson, Paul M.; Bendall, Jason; Thomas, Richard E.; Cone, David C.; Doi, Suhail A. R. (2014-04-03). "Airways in Out-of-hospital Cardiac Arrest: Systematic Review and Meta-analysis". Prehospital Emergency Care. 18 (2): 244–256. doi:10.3109/10903127.2013.831509. ISSN 1090-3127. PMID 24111481.
- ↑ Bernhard, Michael; Benger, Jonathan R. "Airway management during cardiopulmonary resuscitation". Current Opinion in Critical Care. 21 (3): 183–187. doi:10.1097/mcc.0000000000000201.
- ↑ Wik, Lars. "Rediscovering the importance of chest compressions to improve the outcome from cardiac arrest". Resuscitation. 58 (3): 267–269. doi:10.1016/s0300-9572(03)00267-3.
- ↑ Yeung, Joyce; Chilwan, Mehboob; Field, Richard; Davies, Robin; Gao, Fang; Perkins, Gavin D. "The impact of airway management on quality of cardiopulmonary resuscitation: An observational study in patients during cardiac arrest". Resuscitation. 85 (7): 898–904. doi:10.1016/j.resuscitation.2014.02.018.
- ↑ Sayre, Michael R.; Berg, Robert A.; Cave, Diana M.; Page, Richard L.; Potts, Jerald; White, Roger D. (2008-04-22). "Hands-Only (Compression-Only) Cardiopulmonary Resuscitation: A Call to Action for Bystander Response to Adults Who Experience Out-of-Hospital Sudden Cardiac Arrest". Circulation. 117 (16): 2162–2167. doi:10.1161/CIRCULATIONAHA.107.189380. ISSN 0009-7322. PMID 18378619.
Further reading
| The Wikibook First Aid has a page on the topic of: Airway Management |
- Daniel Limmer; Keith J. Karren; Brent Q. Hafen; John Mackay; Michelle Mackay (2006). Emergency Medical Responder (Second Canadian Version). Brady. pp. 92–97. ISBN 0-13-127824-X.