Urinary retention
| Urinary retention | |
|---|---|
 | |
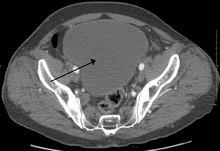
| Urinary retention with greatly enlarged bladder at CT. | |
| Classification and external resources | |
| Specialty | Urology |
| ICD-10 | R33 |
| ICD-9-CM | 788.2 |
| DiseasesDB | 13582 |
| Patient UK | Urinary retention |
| MeSH | D016055 |
Urinary retention, also known as ischuria, is an inability to completely empty the bladder. It is a common complication of benign prostatic hyperplasia (BPH), though it can also be caused by:
- Nerve dysfunction
- Tethered spinal cord syndrome
- Constipation
- Infection
- Medications (including anticholinergics, antidepressants, COX-2 inhibitors, amphetamines, and opioids)
Diagnosis and treatment may require a catheter or prostatic stent.
Signs and symptoms
Urinary retention is characterised by poor urinary stream with intermittent flow, straining, a sense of incomplete voiding, and hesitancy (a delay between trying to urinate and the flow actually beginning). As the bladder remains full, it may lead to incontinence, nocturia (need to urinate at night), and high frequency. Acute retention, causing complete anuria, is a medical emergency, as the bladder can stretch to an enormous size, and possibly tear if not dealt with quickly. If the bladder distends enough, it becomes painful. In such a case, there may be suprapubic constant, dull, pain. The increase in bladder pressure can also prevent urine from entering the ureters or even cause urine to pass back up the ureters and get into the kidneys, causing hydronephrosis, and possibly pyonephrosis, kidney failure, and sepsis. A person should go straight to an emergency department or A&E service as soon as possible if unable to urinate with a painfully full bladder.
Causes
In the bladder
- Detrusor sphincter dyssynergia
- Neurogenic bladder (commonly pelvic splanchic nerve damage, cauda equina syndrome, descending cortical fibers lesion, pontine micturation or storage center lesions, demyelinating diseases or Parkinson's disease)
- Iatrogenic (caused by medical treatment/procedure) scarring of the bladder neck (commonly from removal of indwelling catheters or cystoscopy operations)
- Damage to the bladder
In the prostate
- Benign prostatic hyperplasia (BPH)
- Prostate cancer and other pelvic malignancies
- Prostatitis
- Congenital urethral valves
- Phimosis or pinhole meatus
- Circumcision
- Obstruction in the urethra, for example a stricture (usually caused either by injury or STD), a metastasis or a precipitated pseudogout crystal in the urine
- STD lesions (gonorrhoea causes numerous strictures, leading to a "rosary bead" appearance, whereas chlamydia usually causes a single stricture)
Other
- Tethered spinal cord syndrome
- Psychogenic causes (psychosocial stresses, fear associated with urination, Paruresis ("shy bladder syndrome")- in extreme cases, urinary retention can result)
- Consumption of some psychoactive substances, mainly stimulants, such as MDMA and amphetamine.
- Use of NSAIDs or drugs with anticholinergic properties.
- Stones or metastases can theoretically appear anywhere along the urinary tract, but vary in frequency depending on anatomy
- Muscarinic antagonist such as Atropine and Scopolamine
Diagnosis
Analysis of urine flow may aid in establishing the type of micturition (urination) abnormality. Common findings, determined by ultrasound of the bladder, include a slow rate of flow, intermittent flow, and a large amount of urine retained in the bladder after urination. A normal test result should be 20-25 mL/s peak flow rate. A post-void residual urine greater than 50 ml is a significant amount of urine and increases the potential for recurring urinary tract infections. In adults older than 60 years, 50-100 ml of residual urine may remain after each voiding because of the decreased contractility of the detrusor muscle. In chronic retention, ultrasound of the bladder may show massive increase in bladder capacity (normal capacity is 400-600 ml).
Determining the serum prostate-specific antigen (PSA) may help diagnose or rule out prostate cancer, though this is also raised in BPH and prostatitis. A TRUS biopsy of the prostate (trans-rectal ultra-sound guided) can distinguish between these prostate conditions. Serum urea and creatinine determinations may be necessary to rule out backflow kidney damage. Cystoscopy may be needed to explore the urinary passage and rule out blockages.
In acute cases of urinary retention where associated symptoms in the lumbar spine are present such as pain, numbness (saddle anesthesia), parasthesias, decreased anal sphincter tone, or altered deep tendon reflexes, an MRI of the lumbar spine should be considered to further assess Cauda Equina Syndrome.
Complications

Urinary retention often occurs without warning. It is basically the inability to pass urine. In some people, the disorder starts gradually but in others it may appear suddenly. Acute urinary retention is a medical emergency and requires prompt treatment. The pain can be excruciating when urine is not able to flow out. Moreover, one can develop severe sweating, chest pain, anxiety and high blood pressure. Other patients may develop a shock-like condition and may require admission to a hospital. Serious complications of untreated urinary retention include bladder damage and chronic kidney failure.[1] Urinary retention is a disorder treated in a hospital, and the quicker one seeks treatment, the fewer the complications.
In the longer term, obstruction of the urinary tract may cause:
- Bladder stones
- Atrophy of the detrusor muscle (atonic bladder is an extreme form)
- Hydronephrosis (congestion of the kidneys)
- Hypertrophy of the detrusor muscle (the muscle that squeezes the bladder to empty it during urination)
- Diverticula (formation of pouches) in the bladder wall (which can lead to stones and infection)
Treatment
In acute urinary retention, urinary catheterization, placement of a prostatic stent or suprapubic cystostomy relieves the retention. In the longer term, treatment depends on the cause. BPH may respond to alpha blocker and 5-alpha-reductase inhibitor therapy, or surgically with prostatectomy or transurethral resection of the prostate (TURP). Older patients with ongoing problems may require continued intermittent self catheterization.[2] 5-alpha-reductase inhibitor increase the chance of normal urination following catheter removal.[3] In case, if catheter can't be negotiated, suprapubic puncture can be done with lumbar puncture needle.
Medication
Some people with BPH are treated with medications. These include tamsulosin to relax smooth muscles in the bladder neck, and finasteride and dutasteride to decrease prostate enlargement. The drugs only work for mild cases of BPH but also have mild side effects. Some of the medications decrease libido and may cause dizziness, fatigue and lightheadedness.
Catheter
Acute urinary retention is treated by placement of a urinary catheter (small thin flexible tube) into the bladder. This can be either an intermittent catheter or a Foley catheter that is placed with a small inflatable bulb that holds the catheter in place.
Intermittent catheterization can be done by a health care professional or by the person themselves (clean intermittent self catheterization). Intermittent catheterization performed at the hospital is a sterile technique. Patients can be taught to use a self catheterization[4] technique in one simple demonstration, and that reduces the rate of infection from long-term Foley catheters. Self catheterization requires doing the procedure every 3 or 4 hours 4-6 times a day.
For acute urinary retention, treatment requires urgent placement of a urinary catheter. A permanent urinary catheter may cause discomfort and pain that can last several days.
Surgery
The chronic form of urinary retention may require some type of surgical procedure. While both procedures are relatively safe, complications can occur.
In most patients with benign prostate hyperplasia (BPH), a procedure known as transurethral resection of the prostate (TURP) may be performed to relieve bladder obstruction.[5] Surgical complications from TURP include a bladder infection, bleeding from the prostate, scar formation, inability to hold urine, and inability to have an erection. The majority of these complications are short lived, and most individuals recover fully within 6–12 months.[6]
Sitting voiding position
A meta-analysis on the influence of voiding position on urodynamics in healthy males and males with LUTS showed that in the sitting position, the residual urine in the bladder was significantly reduced. The other parameters, namely the maximum urinary flow and the voiding time were increased and decreased respectively. For healthy males, no influence was found on these parameters, meaning that they can urinate in either position.[7]
Epidemiology
Urinary retention is a common disorder in elderly males. The most common cause of urinary retention is BPH. This disorder starts around age 50 and symptoms may appear after 10–15 years. BPH is a progressive disorder and narrows the neck of the bladder leading to urinary retention. By the age of 70, almost 10 percent of males have some degree of BPH and 33% have it by the eighth decade of life. While BPH rarely causes sudden urinary retention, the condition can become acute in the presence of certain medications (blood pressure pills, anti histamines, antiparkinson medications), after spinal anaesthesia or stroke.
In young males, the most common cause of urinary retention is infection of the prostate (acute prostatitis). The infection is acquired during sexual intercourse and presents with low back pain, penile discharge, low grade fever and an inability to pass urine. The exact numbers of individuals with acute prostatitis is unknown, because many do not seek treatment. In the USA, at least 1-3 percent of males under the age of 40 develop urinary difficulty as a result of acute prostatitis. Most physicians and other health care professionals are aware of these disorders. Worldwide, both BPH and acute prostatitis have been found in males of all races and ethnic backgrounds. Cancers of the urinary tract can cause urinary obstruction but the process is more gradual. Cancer of the bladder, prostate or ureters can gradually obstruct urine output. Cancers often present with blood in the urine, weight loss, lower back pain or gradual distension in the flanks.[8]
References
- ↑ General information on urinary retention 2010-02-10
- ↑ "Clean Intermittent Self-Catheterization".
- ↑ Zeif HJ, Subramonian K (2009). "Alpha blockers prior to removal of a catheter for acute urinary retention in adult men". Cochrane Database Syst Rev (4): CD006744. doi:10.1002/14651858.CD006744.pub2. PMID 19821385.
- ↑ Sherman, Neil D. (August 17, 2006). "Clean Intermittent Self-Catheterization". A.D.A.M., Inc.
- ↑ eMedicine Health. "Inability to urinate" 2010-02-10.
- ↑ National kidney and urologic diseases information clearinghouse. "Urinary retention overview" 2010-02-10.
- ↑ Phillips, Robert S.; de Jong, Ype; Pinckaers, Johannes Henricus Francisca Maria; ten Brinck, Robin Marco; Lycklama à Nijeholt, Augustinus Aizo Beent; Dekkers, Olaf Matthijs (2014). "Urinating Standing versus Sitting: Position Is of Influence in Men with Prostate Enlargement. A Systematic Review and Meta-Analysis". PLoS ONE. 9 (7): e101320. doi:10.1371/journal.pone.0101320. PMC 4106761
 . PMID 25051345.
. PMID 25051345. - ↑ Urologic Emergencies Urology Channel portal. 2010-02-10