Tennis elbow
| Tennis Elbow | |
|---|---|
|
| |
| Left elbow-joint, showing posterior and radial collateral ligaments. (Lateral epicondyle visible at center.) | |
| Classification and external resources | |
| Specialty | Orthopedics, sports medicine |
| ICD-10 | M77.1 |
| ICD-9-CM | 726.32 |
| DiseasesDB | 12950 |
| MedlinePlus | 000449 |
| eMedicine | orthoped/510 pmr/64 sports/59 |
| Patient UK | Tennis elbow |
| MeSH | D013716 |
Tennis elbow or lateral epicondylitis is a condition in which the outer part of the elbow becomes sore and tender. The forearm muscles and tendons become damaged from overuse — repeating the same strenuous motions again and again. This leads to pain and tenderness on the outside of the elbow.[1]
Any activity, including playing tennis, which involves the repetitive use of the extensor muscles of the forearm can cause acute or chronic tendonitis of the tendinous insertion of these muscles at the lateral epicondyle of the elbow. The condition is common in carpenters and laborers who swing a hammer or other tool with the forearm,continuing activity after onset of the condition and avoiding mandatory rest may lead to permanent onset of pain and only treatable via surgery. Dr. F. Runge (a German physician)[2] is usually credited for the first description of the condition in 1873;[3] he called it "writer's cramp" (Schreibekrampf). Later, it was called "washer women's elbow".[4] As it also occurred in tennis, it soon was called "tennis elbow" after British surgeon Henry Morris published an article in The Lancet describing “the lawn tennis arm,” 1883.[5][6] The term "tennis elbow" first appeared in an 1883 paper by H.P. Major as "lawn-tennis elbow".[7][8]
Signs and symptoms
- Pain on the outer part of the elbow (lateral epicondyle)
- Point tenderness over the lateral epicondyle—a prominent part of the bone on the outside of the elbow
- Pain from gripping and movements of the wrist, especially wrist extension and lifting movements
- Pain from activities that use the muscles that extend the wrist (e.g. pouring a container of liquid, lifting with the palm down, sweeping, especially where wrist movement is required)
Symptoms associated with tennis elbow include, but are not limited to: radiating pain from the outside of the elbow to the forearm and wrist, pain during extension of wrist, weakness of the forearm, a painful grip while shaking hands or torquing a doorknob, and not being able to hold relatively heavy items in the hand. The pain is similar to the condition known as golfer's elbow, but the latter occurs at the medial side of the elbow.[9]
Causes
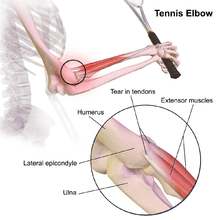
Tennis elbow is a type of repetitive strain injury, resulting from tendon overuse and failed healing of the tendon. In addition, the extensor carpi radialis brevis muscle plays a key role.[10][11]
Early experiments suggested that tennis elbow was primarily caused by overexertion. However, studies show that trauma such as direct blows to the epicondyle, a sudden forceful pull, or forceful extension cause more than half of these injuries.[12] It has also been known that incorrectly playing tennis may cause early stages of tennis elbow as shock is received when mishitting the ball.
Cyriax[12] proposes one explanation of how tennis elbow may come about. The hypothesis states that there are microscopic and macroscopic tears between the common extensor tendon and the periosteum of the lateral humeral epicondyle. An operation conducted in this study showed that 28 out of 39 patients showed tearing at the tendon cuff. Kaplan stated that the radial nerve was significantly involved in tennis elbow. He noted the constriction of the radial nerve by adhesions to the capsule of the radiohumeral joint and the short extensor muscle of the wrist. He found evidence that many differed in how they contracted tennis elbow. Disorders such as calcification of the rotator cuff, bicipital tendinitis, or carpal tunnel syndrome may increase chances of tennis elbow.
Pathophysiology
Histological findings include granulation tissue, microrupture, degenerative changes, and there is no traditional inflammation. As a consequence, “lateral elbow tendinopathy or tendinosis” is used instead of “lateral epicondylitis”.[10]
Examination of tennis elbow tissue reveals noninflammatory tissue, and therefore, the term “angio-fibroblastic tendinosis” is used.[13]
Longitudinal sonogram of the lateral elbow displays thickening and heterogeneity of the common extensor tendon that is consistent with tendinosis, as the ultrasound reveals calcifications, intrasubstance tears, and marked irregularity of the lateral epicondyle. Although the term “epicondylitis” is frequently used to describe this disorder, most histopathologic findings of studies have displayed no evidence of an acute, or a chronic inflammatory process. Histologic studies have demonstrated that this condition is the result of tendon degeneration, which causes normal tissue to be replaced by a disorganized arrangement of collagen. Therefore, the disorder is more appropriately referred to as “tendinosis” or “tendinopathy” rather than “tendinitis.”[14]
Colour Doppler ultrasound reveals structural tendon changes, with vascularity and hypo-echoic areas that correspond to the areas of pain in the extensor origin.[15]
The pathophysiology of lateral epicondylitis is degenerative. Non-inflammatory, chronic degenerative changes of the origin of the extensor carpi radialis brevis (ECRB) muscle are identified in surgical pathology specimens.[16] It is unclear if the pathology is affected by prior injection of corticosteroid.
Tennis players generally believe tennis elbow is caused by the repetitive nature of hitting thousands of tennis balls, which leads to tiny tears in the forearm tendon attachment at the elbow.[17]

The extensor digiti minimi also has a small origin site medial to the elbow that this condition can affect. The muscle involves the extension of the little finger and some extension of the wrist allowing for adaption to "snap" or flick the wrist—usually associated with a racquet swing. Most often, the extensor muscles become painful due to tendon breakdown from over-extension. Improper form or movement allows for power in a swing to rotate through and around the wrist—creating a moment on that joint instead of the elbow joint or rotator cuff. This moment causes pressure to build impact forces to act on the tendon causing irritation and inflammation.
The following speculative rationale is offered by proponents of an overuse theory of etiology: The extensor carpi radialis brevis has a small origin and does transmit large forces through its tendon during repetitive grasping. It has also been implicated as being vulnerable during shear stress during all movements of the forearm.
While it is commonly stated that lateral epicondylitis is caused by repetitive microtrauma/overuse, this is a speculative etiological theory with limited scientific support that is likely overstated.[16] Other speculative risk factors for lateral epicondylitis include taking up tennis later in life, unaccustomed strenuous activity, decreased mental chronometry and speed and repetitive eccentric contraction of muscle (controlled lengthening of a muscle group).
Prevention
Another factor of tennis elbow injury is experience and ability. The proportion of players who reported a history of tennis elbow had an increased number of playing years. As for ability, poor technique increases the chance for injury much like any sport. Therefore, an individual must learn proper technique for all aspects of their sport. The competitive level of the athlete also affects the incidence of tennis elbow. Class A and B players had a significantly higher rate of tennis elbow occurrence compared to class C and novice players. However, an opposite, but not statistically significant, trend is observed for the recurrence of previous cases, with an increasingly higher rate as ability level decreases.[9]
Other ways to prevent tennis elbow:
- Decrease the amount of playing time if already injured or feeling pain in outside part of the elbow.
- Stay in overall good physical shape.
- Strengthen the muscles of the forearm: (pronator quadratus, pronator teres, and supinator muscle)—the upper arm: (biceps, triceps)—and the shoulder (deltoid muscle) and upper back (trapezius). Increased muscular strength increases stability of joints such as the elbow.
- Like other sports, use equipment appropriate to your ability, body size, and muscular strength.[9]
- Avoid any repetitive lifting or pulling of heavy objects (especially over your head) [18]
Vibration dampeners (otherwise known as "gummies") are not believed to be a reliable preventative measure. Rather, proper weight distribution in the racket is thought to be a more viable option in negating shock.[19]
Diagnosis
To diagnose tennis elbow, the physician performs a battery of tests in which he places pressure on the affected area while asking the patient to move the elbow, wrist, and fingers. X-rays can confirm and distinguish possibilities of existing causes of pain that are unrelated to tennis elbow, such as fracture or arthritis. Medical ultrasonography and magnetic resonance imaging (MRI) are other valuable tools for diagnosis but are frequently avoided due to the high cost.[9] MRI screening can confirm excess fluid and swelling in the affected region in the elbow, such as the connecting point between the forearm bone and the extensor carpi radialis brevis.
Diagnosis is made by clinical signs and symptoms that are discrete and characteristic. With the elbow fully extended, the patient feels points of tenderness over the affected point on the elbow—which is the origin of the extensor carpi radialis brevis muscle from the lateral epicondyle (extensor carpi radialis brevis origin). There is also pain with passive wrist flexion and resistive wrist extension (Cozen's test).[20] Resisted middle finger extension might indicate the involvement of Extensor Digitorum also. These tests shall be used to measure the prognosis of the condition.
Depending upon severity and quantity of multiple tendon injuries that have built up, the extensor carpi radialis brevis may not be fully healed by conservative treatment. Nirschl defines four stages of lateral epicondylitis, showing the introduction of permanent damage beginning at Stage 2.
- Inflammatory changes that are reversible
- Nonreversible pathologic changes to origin of the extensor carpi radialis brevis muscle
- Rupture of ECRB muscle origin
- Secondary changes such as fibrosis or calcification.[21]
Treatment
Evidence for the treatment of lateral epicondylitis before 2010 was poor.[22] There were clinical trials addressing many proposed treatments, but the trials were of poor quality.[23]
A 2009 study looked at using eccentric exercise with a rubber bar in addition to standard treatment: the trial was stopped after 8 weeks because the improvement using the bar for therapy was so significant.[24][25] Based on small sample size and a follow-up only 7 weeks from commencement of treatment, the study shows short-term improvements. This along with other studies allowed doctors to conclude that approximately 80-95% of all tennis elbow cases can be treated without surgery. However, long-term results have not yet been determined.
In some cases, severity of tennis elbow symptoms mend without any treatment, within six to 24 months. Tennis elbow left untreated can lead to chronic pain that degrades quality of daily living.[9]
Physical
There are several recommendations regarding prevention, treatment, and avoidance of recurrence that are largely speculative including stretches and progressive strengthening exercises to prevent re-irritation of the tendon[26][27] and other exercise measures.[28]
One way to help treat minor cases of tennis elbow is to simply relax the affected arm. The rest will allow the stress and tightness within the forearm to slowly relax and eventually have the arm in working condition once again in a day or two, depending on the case.
Evidence from the Tyler study suggests that eccentric exercise using a rubber bar is highly effective at eliminating pain and increasing strength.[24][25][29] The exercise involves grasping a rubber bar, twisting it, then slowly untwisting it.[24][30]
Moderate evidence exists demonstrating that joint manipulation directed at the elbow and wrist and spinal manipulation directed at the cervical and thoracic spinal regions results in clinical changes to pain and function.[31][32] There is also moderate evidence for short-term and mid-term effectiveness of cervical and thoracic spine manipulation as an add-on therapy to concentric and eccentric stretching plus mobilisation of wrist and forearm. Although not yet conclusive, the short-term analgesic effect of manipulation techniques may allow more vigorous stretching and strengthening exercises, resulting in a better and faster recovery process of the affected tendon in lateral epicondylitis.[33]
Low level laser therapy, administered at specific doses and wavelengths directly to the lateral elbow tendon insertions, offers short-term pain relief and less disability in tennis elbow, both alone and in conjunction with an exercise regimen.[34] Of late, dry needling has been gaining popularity in various types of tendinopathies and pain of muscular origin. Even in lateral epicondylitis, dry needling is widely employed by many physical therapists across the world. It is believed that dry needling would cause a tiny local injury in order to bring about various desirable growth factors in the vicinity. Dry needling is also aimed at eliciting local twitch response (LTR) in the extensor muscles, as in some cases of tennis elbow the extensor muscles of the forearm would harbor trigger points, which itself could be a major source of pain.
Orthotic devices


Orthosis is a device externally used on the limb to improve the function or reduce the pain. Orthotics are useful therapeutic interventions for initial therapy of tennis elbow. There are two main types of orthoses prescribed for this problem: counterforce elbow orthoses and wrist extension orthoses.
Counterforce orthosis has a circumferential structure surrounding the arm. This orthosis usually has a strap which applies a binding force over the origin of the wrist extensors. The applied force by orthosis reduces the elongation within the musculotendinious fibers. Wrist extensor orthosis maintains the wrist in the slight extension. This position reduces the overloading strain at the lesion area.
Studies indicated both type of orthoses improve the hand function [35] and reduce the pain [36] in people with tennis elbow.
Medication
Although anti-inflammatories are a commonly prescribed treatment for tennis elbow, the evidence for their effect is usually anecdotal with only limited studies showing a benefit.[37] A systematic review found that topical non-steroidal anti-inflammatory drugs (NSAIDs) may improve pain in the short term (up to 4 weeks) but was unable to draw firm conclusions due to methodological issues.[38] Evidence for oral NSAIDs is mixed.[38]
Evidence is poor for an improvement from injections of any type, be it corticosteroids, botulinum toxin, prolotherapy or other substances.[39] Corticosteroid injection may be effective in the short term[40] however are of little benefit after a year, compared to a wait-and-see approach.[41] A recent randomized control trial comparing the effect of corticosteroid injection, physiotherapy, or a combination of corticosteroid injection and physiotherapy found that patients treated with corticosteroid injection versus placebo had lower complete recovery or improvement at 1 year (Relative risk 0.86). Patients that received corticosteroid injection also had a higher recurrence rate at 1 year versus placebo (54% versus 12%, relative risk 0.23).[42] Complications from repeated steroid injections include skin problems such as hypopigmentation and fat atrophy leading to indentation of the skin around the injection site.[40] Botulinum toxin type A to paralyze the forearm extensor muscles in those with chronic tennis elbow that has not improved with conservative measures may be reasonable.[43]
Surgery
In recalcitrant cases, surgery may be an option.[44][45][46] Surgical methods include:[47]
- Lengthening, release, debridement, or repair of the origin of the extrinsic extensor muscles of the hand at the lateral epicondyle
- Rotation of the anconeus muscle
- Denervation of the lateral epicondyle
- Decompression of the posterior interosseous nerve
Surgical techniques for lateral epicondylitis can be done by open surgery, percutaneous surgery or arthroscopic surgery, with no evidence that any particular type is better or worse than another.[45]
Prognosis
Response to initial therapy is common, but so is relapse (25% to 50%) and/or prolonged, moderate discomfort (40%).
Epidemiology
In tennis players, about 39.7% have reported current or previous problems with their elbow. Less than one quarter (24%) of these athletes under the age of 50 reported that the tennis elbow symptoms were "severe" and "disabling," while 42% were over the age of 50. More women (36%) than men (24%) considered their symptoms severe and disabling. Tennis elbow is more prevalent in individuals over 40, where there is about a four-fold increase among men and two-fold increase among women. Tennis elbow equally affects both sexes and, although men have a marginally higher overall prevalence rate as compared to women, this is not consistent within each age group, nor is it a statistically significant difference.[48]
Playing time is a factor in tennis elbow occurrences. However, increased incidence with increased playing time is statistically significant only for respondents under 40. Individuals over 40 who played over two hours had a two-fold increase in chance of injury. Those under 40 had a 3.5 times increase compared to those who played less than two hours per day.[9]
See also
- Golfer's elbow
- Olecranon bursitis
- Tendinitis
- Tendinosis
- Repetitive strain injury
- Radial tunnel syndrome
References
- ↑ American Academy of Orthopedic Surgery Information
- ↑ "TENNIS ELBOW-CAP". The Lancet. 128 (3301): 1083. 1886. doi:10.1016/s0140-6736(00)49587-5.
- ↑ Runge F (1873). "Zur Genese und Behandlung des Schreibekrampfes.". Berliner Klin Wochenschr. 10: 245–248.
- ↑ Science and Racket Sports Edited by: T. Reilly, M. Hughes and A.Lees. Published by E & FN Spon ISBN 0-419-18500-3.
- ↑ Flatt Adrian E (Oct 2008). "Tennis elbow". Proc (Bayl Univ Med Cent). 21 (4): 400–402. PMC 2566914
 . PMID 18982084.
. PMID 18982084. - ↑ "TENNIS ELBOW-CAP". The Lancet. 128 (3301): 1083. 1886. doi:10.1016/s0140-6736(00)49587-5.
- ↑ Major HP (1883). "Lawn-tennis elbow". BMJ. 2: 557.
- ↑ Kaminsky SB, Baker CL; Baker (December 2003). "Lateral epicondylitis of the elbow". Techniques in Hand & Upper Limb Surgery. 7 (4): 179–89. doi:10.1097/00130911-200312000-00009. PMID 16518219.
- 1 2 3 4 5 6 "Tennis Elbow - MayoClinic.com." Mayo Clinic Medical Information and Tools for Healthy Living - MayoClinic.com. 15 Oct. 2008. Web. 10 Oct. 2010.
- 1 2 du Toit, C; Stieler, M; Saunders, R; Bisset, L; Vicenzino, B (2008). "Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow". British Journal of Sports Medicine. 42 (11): 572–576. doi:10.1136/bjsm.2007.043901. ISSN 0306-3674.
- ↑ Nirschl RP, Ashman ES (2004). "Tennis elbow tendinosis (epicondylitis)". Instr Course Lect. 53: 587–98. PMID 15116648.
- 1 2 KURPPA, K., WARIS, P. and ROKKANEN, P. Tennis elbow: Lateral elbow pain syndrome. Scand j. work environ. & health 5 (1979): suppl. 3, 15-18. A review of the etiology, occurrence and pathogenesis of "tennis elbow" is presented.
- ↑ Nirschl RP (October 1992). "Elbow tendinosis/tennis elbow". Clin Sports Med. 11 (4): 851–70. PMID 1423702.
- ↑ McShane JM, Nazarian LN, Harwood MI (October 2006). "Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow". J Ultrasound Med. 25 (10): 1281–9. PMID 16998100.
- ↑ Zeisig, Eva; Öhberg, Lars; Alfredson, Håkan (2006). "Sclerosing polidocanol injections in chronic painful tennis elbow-promising results in a pilot study". Knee Surgery, Sports Traumatology, Arthroscopy. 14 (11): 1218–1224. doi:10.1007/s00167-006-0156-0. ISSN 0942-2056.
- 1 2 Boyer MI, Hastings H (1999). "Lateral tennis elbow: "Is there any science out there?"". Journal of Shoulder and Elbow Surgery. 8 (5): 481–91. doi:10.1016/S1058-2746(99)90081-2. PMID 10543604.
- ↑ What is tennis elbow? from the BBC Sport Academy website
- ↑ http://www.dovemed.com/tennis-elbow/
- ↑ http://www.racquetresearch.com/sevencri.htm#What Causes Tennis Elbow?
- ↑ Tennis elbow from the MedlinePlus Medical Encyclopedia
- ↑ Owens, Brett D; Moriatis Wolf, Jennifer; Murphy, Kevin P (2009-11-03). "Lateral Epicondylitis: Workup". eMedicine Orthopedic Surgery. Retrieved 2010-04-19.
- ↑ Bisset L, Paungmali A, Vicenzino B, Beller E (July 2005). "A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia". British Journal of Sports Medicine. 39 (7): 411–22; discussion 411–22. doi:10.1136/bjsm.2004.016170. PMC 1725258
 . PMID 15976161.
. PMID 15976161. - ↑ Cowan J, Lozano-Calderón S, Ring D (August 2007). "Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example". The Journal of Bone and Joint Surgery. 89 (8): 1693–9. doi:10.2106/JBJS.F.00858. PMID 17671006.
- 1 2 3 Tyler Timothy F.; Thomas Gregory C.; Nicholas Stephen J.; McHuch Malachy P. "Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis:a radomized trial". Journal of Shoulder and Elbow Surgery. 19 (6): 917–922. doi:10.1016/j.jse.2010.04.041.
- 1 2 Reynolds, Gretchen, "Phys Ed:An Easy Fix for Tennis Elbow?", The New York Times, August 25, 2009, 11:54 pm
- ↑ Stasinopoulos D, Stasinopoulou K, Johnson MI (December 2005). "An exercise programme for the management of lateral elbow tendinopathy". British Journal of Sports Medicine. 39 (12): 944–7. doi:10.1136/bjsm.2005.019836. PMC 1725102
 . PMID 16306504.
. PMID 16306504. - ↑ Tennis elbow
- ↑ http://www.tenniselbowsolutions.co.uk/cure-your-tennis-elbow.html
- ↑ Gretchen Reynolds (August 25, 2009). "Phys Ed: An Easy Fix for Tennis Elbow?". New York Times.
- ↑
- ↑ Vicenzino B, Cleland JA, Bisset L (2007). "Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary". Journal of Manual & Manipulative Therapy. 15 (1): 50–56. doi:10.1179/106698107791090132. PMC 2565595
 . PMID 19066643.
. PMID 19066643. - ↑ Herd CR, Meserve BB (2008). "A Systematic Review of the Effectiveness of Manipulative Therapy in Treating Lateral Epicondylalgia". Journal of Manual & Manipulative Therapy. 16 (4): 225–37. doi:10.1179/106698108790818288. PMC 2716156
 . PMID 19771195.
. PMID 19771195. - ↑ Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BM (2013). "Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review.". Br J Sports Med. 47 (17): 1112–9. doi:10.1136/bjsports-2012-091990. PMID 23709519.
- ↑ Bjordal JM, Lopes-Martins RA, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, Johnson MI (2008). "A systematic review with procedural assessments and meta-analysis of Low Level Laser Therapy in lateral elbow tendinopathy (tennis elbow)". BMC Musculoskeletal Disorders. 9: 75. doi:10.1186/1471-2474-9-75. PMC 2442599
 . PMID 18510742.
. PMID 18510742. - ↑ "The Immediate Effect of Orthotic Management on Grip Strength of Patients With Lateral Epicondylosis". Journal of Orthopaedic & Sports Physical Therapy. 39 (6): 484–489. 2009-06-01. doi:10.2519/jospt.2009.2988. ISSN 0190-6011.
- ↑ Sadeghi-Demneh, Ebrahim; Jafarian, Fahimehsadat (2013-01-01). "The Immediate Effects of Orthoses on Pain in People with Lateral Epicondylalgia". Pain Research and Treatment. 2013: 1–6. doi:10.1155/2013/353597. PMC 3854508
 . PMID 24349776.
. PMID 24349776. - ↑ Jayanthi, Neeru. "Epicondylitis (tennis and golf elbow)". UpToDate. UpToDate, Inc. Retrieved 17 August 2015.
- 1 2 Pattanittum, P; Turner, T; Green, S; Buchbinder, R (May 31, 2013). "Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults.". The Cochrane database of systematic reviews. 5: CD003686. doi:10.1002/14651858.CD003686.pub2. PMID 23728646.
- ↑ Krogh, TP; Bartels, EM; Ellingsen, T; Stengaard-Pedersen, K; Buchbinder, R; Fredberg, U; Bliddal, H; Christensen, R (June 2013). "Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials.". The American journal of sports medicine. 41 (6): 1435–46. doi:10.1177/0363546512458237. PMID 22972856.
- 1 2 Coombes, BK; Bisset, L; Vicenzino, B (Nov 20, 2010). "Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials". Lancet. 376 (9754): 1751–67. doi:10.1016/S0140-6736(10)61160-9. PMID 20970844.
- ↑ Haines T, Stringer B (April 2007). "Corticosteroid injections or physiotherapy were not more effective than "wait-and-see" for tennis elbow at one year". Evidence-based Medicine. 12 (2): 39. doi:10.1136/ebm.12.2.39. PMID 17400631.
- ↑ Coombes, BK; Bisset, L; Brooks, P; Khan, A; Vicenzino, B (Feb 6, 2013). "Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial.". JAMA: the Journal of the American Medical Association. 309 (5): 461–9. doi:10.1001/jama.2013.129. PMID 23385272.
- ↑ Kalichman, L; Bannuru, RR; Severin, M; Harvey, W (June 2011). "Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis". Seminars in arthritis and rheumatism. 40 (6): 532–8. doi:10.1016/j.semarthrit.2010.07.002. PMID 20822798.
- ↑ Monto, R (September 2014). "Tennis elbow repair with or without suture anchors: a randomized clinical trial". Techniques in Shoulder and ELbow Surgery. 15 (3): 92–97. doi:10.1097/BTE.0000000000000027.
- 1 2 Lo, MY; Safran, MR (October 2007). "Surgical treatment of lateral epicondylitis: a systematic review". Clinical orthopaedics and related research. 463: 98–106. doi:10.1097/BLO.0b013e3181483dc4. PMID 17632419.
- ↑ Solheim E, Hegna J, Øyen J. Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows. Arthroscopy. 2013 May;29(5):854–9.
- ↑ Faro, Frances; Wolf, Jennifer Moriatis (2007). "Lateral Epicondylitis: Review and Current Concepts". The Journal of Hand Surgery. 32 (8): 1271–1279. doi:10.1016/j.jhsa.2007.07.019. ISSN 0363-5023.
- ↑ Gruchow, William, and Douglas Pelletier. "An epidemiologic study of tennis elbow: Incidence, recurrence, and effectiveness of prevention strategies." American Journal of Sports Medicine. 7.4 (1979): 234-238. Print.
Further reading
- Wilson JJ, Best TM (September 2005). "Common overuse tendon problems: A review and recommendations for treatment". American Family Physician. 72 (5): 811–8. PMID 16156339.