Sudden death of athletes
The prevention of sudden death of athletes, defined as natural, unexpected, death within one hour of the onset of symptoms and subsequent cardiac arrest,[1] remains a challenge. The prevalence of any single, associated condition is very low, probably less than 0.3% and the sensitivity and specificity of tests commonly used to screen leaves much to be desired.
Wider definitions of sudden death are also in use but not usually applied to the athletic situation.
The single most important predictor is exercise fainting or near fainting, which should require explanation and investigation.[2]
While most causes relate to congenital or acquired cardiovascular disease, an exception is commotio cordis, in which the heart is structurally normal but a potentially fatal loss of rhythm occurs because of the accident of timing of a blow to the chest. Survival is about 15% and time to CPR and defibrillation may determine this.

Incidence
Sudden death occurs in approximately one in 200,000 athletes annually.[3] The victim is usually male and, in the US, two-thirds occur in football and basketball. This reflects the popularity of these sports and the number of athletes involved in them and elsewhere in the world, soccer is most commonly associated. From statistics derived from NCAA data, one death per 25,000 collegiate athletes over a five-year period was attributable to medical causes.[4]
A series of observational studies have reported on death rates in athletes for causes other than trauma. Van Camp reported rates of approximately 7:1,000,000 and 1:1,000,000 for male and female high school and colleges students respectively, during organized athletic activity.[5] Philips reported rates of 1:735,000 US Air Force recruits aged 17 to 28 during training.[6] The sudden death rate amongst Rhode Island joggers was reported as 1:280,000 for those under 30 years of age, by Ragosta,[7] and 1:7,260 for those 30–65 years according to Thompson.[8] Finally, Maron reported rates of 1:50,000 race finishers in marathons, where the mean age was 37.[9]
To place in context, sudden cardiac death in the US (population 300 million), is estimated to occur 180,000 – 250,000 times per year. [10] While the predominant cause is coronary artery and other vascular disease, about 20% of cases show no obvious structural cardiovascular abnormality and remain undiagnosed after autopsy. Interest in these 'autopsy-negative' deaths in the past ten years has centered around the 'ion channelopathies'. These channels are pores controlling the movement of sodium, potassium and calcium ions into cardiac cells, cumulatively responsible for creating and controlling the electrical signals which control the heart's rhythm. Abnormalities in this system are known to cause relatively rare genetic diseases such as 'Long QT syndrome', 'Brugada syndrome' and 'Catecholaminergic polymorphic ventricular tachycardia', all associated with sudden death. Consequently, more patients with autopsy-negative sudden cardiac death (no genetic abnormalities identified) may comprise a larger part of the 'channelopathies' than previously anticipated and it has been estimated that their incidence may be as high as 11/100,000, in a survey of unexpected sudden cardiac death in England, involving presumed healthy individuals aged 16–64 years.[11][12]
Age
Age 35 serves as a watershed as to the likely cause of sudden death. Before age 35, congenital abnormalities of the heart and blood vessels predominate. These are usually asymptomatic prior to the fatal event although not invariably so. Congenital cardiovascular problems are reported to occur disproportionately in African-American athletes.
After age 35, acquired coronary artery disease predominates (80%),[3] and this is true regardless of the athlete's former level of fitness.
Causes
| Cause | Incidence | |
|---|---|---|
| Hypertrophic cardiomyopathy | 26.4% | Genetically determined |
| Commotio cordis | 19.9% | Structurally normal heart |
| Coronary artery anomalies | 13.7% | Exact mechanisms unknown - some association with other congenital cvs abnormalities |
| Left ventricular hypertrophy of undetermined origin | 7.5% | Probable variant of hypertrophic cardiomyopathy |
| Myocarditis | 5.2% | |
| Ruptured aortic aneurysm (Marfan syndrome) | 3.2% | Genetically determined |
| Arrhythmogenic right ventricular cardiomyopathy | 2.8% | Genetically determined |
| Tunneled coronary artery | 2.8% | |
| Aortic valve stenosis | 2.6% | |
| Atherosclerotic coronary artery disease | 2.6% | Mainly acquired |
Screening
Screening is problematic because of low prevalence and indifferent performance of various tests that have been used. Nevertheless, sudden death attracts much public and legislator attention because of its visible and tragic nature. As an example, the Texas Legislature appropriated funds for a pilot study of statewide screening in 2007.

The study employed a combination of questionnaire, examination, and electrocardiography, in all students and echocardiography in a majority selected because of abnormal findings in the preceding three. 35% of the student population studied were flagged as potentially at risk but there were many false positive results with actual disease being confirmed in only 1.23%. Further, a substantial number of that 1.23% declined follow-up evaluation.[15] It should be stressed that this is a single pilot program and original research, but it is indicative of the problems associated with screening and concordant with other experience.
Genetics
Cardiomyopathy

Cardiomyopathies are generally inherited as autosomal dominants although recessive forms have been described, and dilated cardiomyopathy can also be inherited in an X linked pattern. Consequently, in addition to tragedy involving an athlete who succumbs, there are wider implications. Within many families of index cases, more than 300 causative mutations have been identified although there is no clear understanding of how these mutations (which affect the same myosin molecule) can lead to the dramatically different clinical characteristics and outcomes associated with hypertrophic cardiomyopathy(HCM) and dilated cardiomyopathy(DCM).[16]
Since HCM, as an example, is typically an autosomal dominant trait, children of an HCM parent have a 50% chance of inheriting the mutation. In individuals without a family history, the most common cause of the disease is a 'de novo' mutation of the gene that produces the β-myosin heavy chain. Not all mutations, it should be noted, have the same potential for a disastrous outcome. For example, troponin T mutations are associated with a 50% mortality before the age of 40, while β-myosin mutations are less threatening.
The role of 'channelopathies' leading to 'Brugada syndrome', 'long QT syndrome' and 'Catecholaminergic polymorphic ventricular tachycardia' has been referred to in 'incidence'.
Heritable connective tissue disease. Heritable connective tissue diseases are rare, each disorder estimated at one to ten per 100,000 of which 'Marfan syndrome' is the most common.
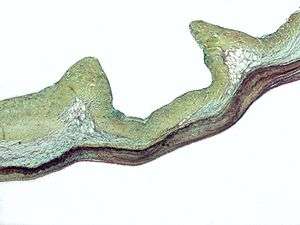
It is carried by the FBN1 gene on chromosome 15, which encodes the connective protein fibrillin-1,[17][18] inherited as a dominant trait. This protein is essential for synthesis and maintenance of elastic fibers. Since these fibers are particularly abundant in the aorta, ligaments and the ciliary zonules of the eye, these areas are among the worst affected. Everyone has a pair of FBN1 genes and because transmission is dominant, those who have inherited one affected FBN1 gene from either parent will have Marfan syndrome. Although it is most frequently inherited as an 'autosomal dominant', there is no family history in 25% of cases.[19]
Recruiting practices aimed at attracting athletes who are unusually tall or who have an unusually wide arm span (phenotypic characteristics of Marfan Syndrome) have the potential to alter the expected prevalence of the syndrome within certain sports.
Testing
Once a disease causing mutation has been identified in an index case, the main task is genetic identification of carriers within a pedigree, a process known as “cascade testing.” Family members with the same mutation may show different severities of disease, a phenomenon known as variable penetrance. As a result, some may remain asymptomatic, with little lifelong evidence of disease. Nevertheless, their children remain at risk of inheriting the disorder and potentially being more severely affected.[20]
Notable athletes who have succumbed
- Pheidippides
- Hank Gathers
- Reggie Lewis
- Marc-Vivien Foé
- Pete Maravich
- Flo Hyman
- Jim Fixx
- Sergei Grinkov
- Darryl Kile
- Miklós Fehér
- Alexander Dale Oen
- Eddie Guerrero
References
- ↑ van der Werf C, van Langen IM, Wilde AA (February 2010). "Sudden death in the young: what do we know about it and how to prevent?". Circ Arrhythm Electrophysiol. 3 (1): 96–104. doi:10.1161/CIRCEP.109.877142. PMID 20160177.
- ↑ Hastings JL, Levine BD (March 2012). "Syncope in the athletic patient". Prog Cardiovasc Di. 54 (5): 438–44. doi:10.1016/j.pcad.2012.02.003. PMID 22386295.
- 1 2 Ferreira M, Santos-Silva PR, de Abreu LC, Valenti VE, Crispim V, Imaizumi C, Filho CF, Murad N, Meneghini A, Riera AR, de Carvalho TD, Vanderlei LC, Valenti EE, Cisternas JR, Moura Filho OF, Ferreira C (Aug 3, 2010). "Sudden cardiac death athletes: a systematic review". Sports Med Arthrosc Rehabil Ther Technol. 2:19. doi:10.1186/1758-2555-2-19. PMC 2923123
 . PMID 20682064.
. PMID 20682064. - ↑ Harmon KG, Asif IM, Klossner D, Drezner JA (Apr 4, 2011). "Incidence of sudden cardiac death in national collegiate athletic association athletes". Circulation. 123(15): (15): 1594–600. doi:10.1161/CIRCULATIONAHA.110.004622. PMID 21464047.
- ↑ Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG (1995). "Nontraumatic sports death in high school and college athletes". Med Sci Sports Exerc. 27 (5): 641–7. doi:10.1249/00005768-199505000-00005. PMID 7674867.
- ↑ Phillips M, Robinowitz M, Higgins JR, Boran KJ, Reed T, Virmani R (1986). "Sudden cardiac death in Air Force recruits. A 20-year review". JAMA. 256 (19): 2696–9. doi:10.1001/jama.1986.03380190066026. PMID 3773175.
- ↑ Ragosta M, Crabtree J, Sturner WQ, Thompson PD (1984). "Death during recreational exercise in the State of Rhode Island". Med Sci Sports Exerc. 16 (4): 339–42. doi:10.1249/00005768-198408000-00003. PMID 6493012.
- ↑ Thompson PD, Funk EJ, Carleton RA, Sturner WQ (1982). "Incidence of death during jogging in Rhode Island from 1975 through 1980". JAMA. 247 (18): 2535–8. doi:10.1001/jama.1982.03320430039028. PMID 6978411.
- ↑ Maron BJ, Poliac LC, Roberts WO (1996). "Risk for sudden cardiac death associated with marathon running". J Am Coll Cardiol. 28 (2): 428–31. doi:10.1016/0735-1097(96)00137-4. PMID 8800121.
- ↑ Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, Mariani R, Gunson K, Jui J (Nov–Dec 2008). "Epidemiology of sudden cardiac death: clinical and research implications". Prog Cardiovasc Dis. 51 (3): 213–28. doi:10.1016/j.pcad.2008.06.003. PMC 2621010
 . PMID 19026856.
. PMID 19026856. - ↑ Westfal RE, Reissman S, Doering G (Jul 1996). "Out-of-hospital cardiac arrests: an 8-year New York City experience". Am J Emerg Med. 14 (4): 364–8. doi:10.1016/S0735-6757(96)90050-9. PMID 8768156.
- ↑ de Vreede-Swagemakers JJ, Gorgels AP, Dubois-Arbouw WI, van Ree JW, Daemen MJ, Houben LG, Wellens HJ (Nov 1997). "Out-of-hospital cardiac arrest in the 1990's: a population-based study in the Maastricht area on incidence, characteristics and survival". J Am Coll Cardiol. 30 (6): 1500–5. doi:10.1016/s0735-1097(97)00355-0. PMID 9362408.
- ↑ Maron BJ, Haas TS, Ahluwalia A, Rutten-Ramos SC (Mar 2013). "Incidence of cardiovascular sudden deaths in Minnesota high school athletes". Heart Rhythm. 10 (3): 374–7. doi:10.1016/j.hrthm.2012.11.024. PMID 23207138.
- ↑ Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S (Apr 2014). "Incidence and causes of sudden death in U.S. college athletes". J Am Coll Cardiol. 63 (16): 1636–43. doi:10.1016/j.jacc.2014.01.041. PMID 24583295.
- ↑ Zeltser I, Cannon B, Silvana L, Fenrich A, George J, Schleifer J, Garcia M, Barnes A, Rivenes S, Patt H, Rodgers G, Scott W (Jun 15, 2012). "Lessons learned from preparticipation cardiovascular screening in a state funded program". Am J Cardiol. 110 (6): 902–8. doi:10.1016/j.amjcard.2012.05.018. PMID 22704711.
- ↑ Moore JR, Leinwand L, Warshaw DM (Jul 20, 2012). "Understanding cardiomyopathy phenotypes based on the functional impact of mutations in the myosin motor". Circ Res. 111 (3): 375–85. doi:10.1161/CIRCRESAHA.110.223842. PMID 22821910.
- ↑ Kainulainen K, Karttunen L, Puhakka L, Sakai L, Peltonen L (January 1994). "Mutations in the fibrillin gene responsible for dominant ectopia lentis and neonatal Marfan syndrome". Nat. Genet. 6 (1): 64–9. doi:10.1038/ng0194-64. PMID 8136837.
- ↑ Dietz HC, Loeys B, Carta L, Ramirez F (November 2005). "Recent progress towards a molecular understanding of Marfan syndrome". Am J Med Genet C Semin Med Genet. 139C (1) (1): 4–9. doi:10.1002/ajmg.c.30068. PMID 16273535.
- ↑ Armon K, Bale P (June 2012). "Identifying heritable connective tissue disorders in childhood". Practitioner. 256 (1752): 19–23, 2–3. PMID 22916581.
- ↑ Raju H, Alberg C, Sagoo GS, Burton H, Behr ER (Nov 21, 2011). "Inherited cardiomyopathies". BMJ. 343: d6966. doi:10.1136/bmj.d6966. PMID 22106372.