Sublingual gland
| Sublingual Gland | |
|---|---|
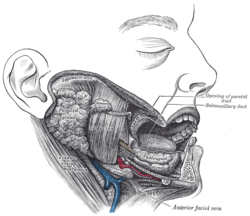 Dissection, showing salivary glands of right side. (Sublingual gland visible near bottom right.) | |
 | |
| Details | |
| System | Digestive system |
| Artery | Sublingual artery (branch of lingual artery of external carotid artery) |
| Nerve | Submandibular ganglion |
| Lymph | Submandibular lymph nodes |
| Identifiers | |
| Latin | Glandula sublingualis |
| MeSH | A03.556.500.760.687 |
| TA | A05.1.02.008 |
| FMA | 59791 |
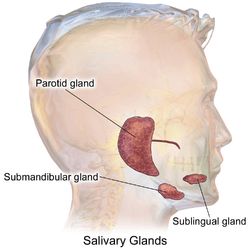
The paired sublingual glands are major salivary glands in the mouth. They are the smallest, most diffuse, and the only unencapsulated major salivary glands. They provide only 3-5% of the total salivary volume.[1]
Structure
They lie anterior to the submandibular gland inferior to the tongue, as well as beneath the mucous membrane of the floor of the mouth. Each gland is effectively palpated on the floor of the mouth posterior to each mandibular canine. Placing one index finger intraorally and the fingertips of the opposite hand extraorally, the compressed gland is manually palpated between the inner and outer fingers.[2]
They are drained by 8-20 excretory ducts called the ducts of Rivinus.[3] The largest of all, the sublingual duct (of Bartholin) joins the submandibular duct to drain through the sublingual caruncle. The sublingual caruncle is a small papilla near the midline of the floor of the mouth on each side of the lingual frenum.[2] Most of the remaining small sublingual ducts open separately into the mouth on an elevated crest of mucous membrane, the plica sublingualis, formed by the gland and located on either side of the frenulum linguae.
Histology
The sublingual gland consists mostly of mucous acini capped with serous demilunes and is therefore categorized as a mixed mucous gland with a mucous product predominating. Striated and intercalated ducts are also present.[1]
Innervation and blood supply
The chorda tympani nerve (from the facial nerve via the submandibular ganglion) is secretomotor and provides parasympathetic supply to the sublingual glands. The path of the nerve is as follows: junction between pons and medulla, through internal acoustic meatus and facial canal to chorda tympani, through middle ear cavity, out petrous temporal to join the lingual nerve, travels with lingual nerve to synapse at the submandibular ganglion, then postganglionic fibers travels to the sublingual gland.
The gland receives its blood supply from the sublingual and submental arteries.[3] Lymph from the sublingual salivary gland drains into the submandibular lymph nodes.[2]
Development
The sublingual salivary glands appear in the eighth week of prenatal development, two weeks later than the other two major salivary glands. They develop from epithelial buds in the sulcus surrounding the sublingual folds on the floor of the mouth, lateral to the developing submandibular gland. These buds branch and form into cords that canalize to form the sublingual ducts associated with the gland. The rounded terminal ends of the cords form acini.[1]
Clinical significance
Ranulas are the most common pathologic lesion associated with the sublingual glands.[4]
Additional images
 Mandible. Inner surface. Side view.
Mandible. Inner surface. Side view.- Sublingual gland
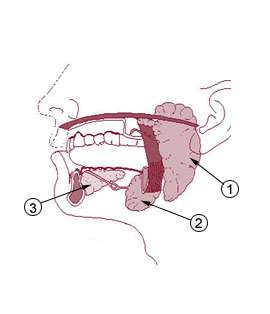
- Sublingual gland
- Sublingual gland
References
- 1 2 3 Illustrated Dental Embryology, Histology, and Anatomy, Bath-Balogh and Fehrenbach, Elsevier, 2011, page 136-137
- 1 2 3 Illustrated Anatomy of the Head and Neck, Fehrenbach and Herring, Elsevier, 2012, p. 156
- 1 2 Ten Cate's Oral Histology, Nanci, Elsevier, 2013, page 255
- ↑ Hupp JR, Ellis E, Tucker MR (2008). Contemporary oral and maxillofacial surgery (5th ed.). St. Louis, Mo.: Mosby Elsevier. pp. 410–411. ISBN 9780323049030.
External links
- Anatomy photo:34:st-0701 at the SUNY Downstate Medical Center - "Oral Cavity: Glands"
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (VII)
- Anatomy diagram: 25420.000-1 at Roche Lexicon - illustrated navigator, Elsevier
- Salivary gland infections from Medline Plus
- Salivary gland cancer from American Cancer Society