Remineralisation of teeth
Remineralisation is a natural process and does not have to involve fluoride.
Tooth remineralisation is a naturally occurring process in the oral cavity.[2] It is defined as a process in which calcium and phosphate ions are sourced to promote ion deposition into crystal voids in demineralised enamel. Remineralisation remains imperative towards the management of non-cavitated carious lesions and prevention of disease progression within the oral cavity. The process also has the ability to contribute towards restoring strength and function within tooth structure.[3]
Tooth demineralization is a chemical process by which minerals (mainly calcium) are removed from any of the hard tissues—enamel, dentine, and cementum.[4] The process of demineralization begins at the crystal surface found inside the hard tooth tissue and may progress into cavitation unless arrested or overriden by remineralisation. The effect of demineralisation can be reversed if there is sufficient time to allow remineralisation to occur to counteract the acids in the oral cavity.[5] Together, demineralisation and remineralisation contribute towards a dynamic process.[6]
Tooth decay process
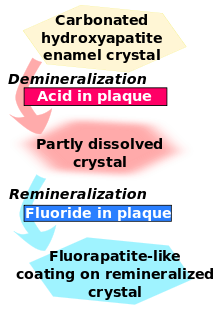
The initiation of the caries process is triggered by an increase in the acidity of bacterial plaque. The process of dental caries occurs when the acid-producing bacteria found in dental plaque on teeth feed on fermentable carbohydrates and produce organic acids as by-products.[7] The acids diffuse into the tooth surface and dissolve the carbonated hydroxyapatite mineral that consecutively forms a carious lesion. When food or drinks containing sugars enter the mouth, the bacteria within the plaque rapidly convert the sugars into acid. The plaque can hold the acid in contact with the tooth surface for up to 2 hours before it is neutralised by saliva. During the time that the plaque is acidic, some of the calcium and phosphate minerals are dissolved out of the enamel into the plaque and once the plaque acid has been neutralised the minerals can return to the enamel surface. However the capacity for remineralisation is limited and if sugars enter the mouth too frequently a net loss of mineral from the enamel surface results in a cavity through which bacteria can penetrate and infect the inner structure of the tooth.[4] Although a key feature of tooth decay is the increase of bacteria such as Streptococcus mutans and Lactobacillus in dental plaque, it is not considered as an infectious disease.[4]
Tooth decay can be managed by modifying behaviour and controlling its causative factors, i.e. reducing the intake frequency of fermentable carbohydrates from food. This will reduce the chance of the dental biofilm developing into cariogenic biofilm. The bacteria in cariogenic biofilm produce organic acids when carbohydrates, especially sugar, are eaten. When enough acid is produced so that the pH goes below 5.5, the acid dissolves carbonated hydroxyapatite, the main component of tooth enamel, in a process known as demineralisation.[8] After the sugar is gone, the mineral loss can be recovered—or remineralised—from ions dissolved in the saliva. Cavities result when the rate of demineralisation exceeds the rate of remineralisation and the latticework is destroyed, typically in a process that requires many months or years.[9]
Natural Tooth Remineralisation
Role of saliva
Saliva, being the watery substance that constantly circulates the oral cavity, is capable of impacting both the remineralisation and demineralisation processes. It is secreted through the major salivary glands including the parotid, submandibular, sublingual and Von Ebner's glands as well as the hundreds of minor salivary glands that are located throughout the oral cavity.[10]
Remineralization occurs on a daily basis after an acidogenic challenge through the presence of saliva.[11] Calcium, phosphate and fluoride found in saliva, are required for effective remineralization and maintenance of the enamel surface integrity.[11] Therefore, as saliva is rich in calcium and phosphate ions, It can act as a natural buffer to neutralise acid and allow demineralised tooth tissues to be remineralised.[4] If there is reduced saliva flow or reduced saliva quality, this will increase the risk of demineralization and create the need for treatment in order to prevent demineralisation progression.[4]
Saliva function can be organised into five major categories that serve to maintain oral health and create an appropriate ecologic balance:
- Lubrication and protection
- Buffering action and clearance
- Maintenance of tooth integrity
- Antibacterial activity
- Taste and digestion.[4]
As the demineralisation process continues, the pH of the mouth becomes more acidic which promotes the development of caries. Dissolved minerals then diffuse out of the tooth structure and into the saliva surrounding the tooth. The buffering capacity of saliva greatly impacts the pH of plaque surrounding the enamel, thereby inhibiting caries progression. Plaque thickness and the number of bacteria present determine the effectiveness of salivary buffers.[4] The high salivary concentrations of calcium and phosphate which are maintained by salivary proteins may account for the development and remineralisation of enamel. The presence of fluoride in saliva speeds up crystal precipitation forming a fluorapatite- like coating which will be more resistant to caries.[4]
Tooth Remineralisation Treatments & Preventative Strategies
Besides professional dental care, there are other ways for promoting tooth remineralisation:
Fluoride
Fluoride therapy
Fluoride is a mineral found naturally in rock, air, soil, plants and water and it assists by:
- Protecting children and adults against tooth decay
- Repairing early white spot lesions found on the tooth surface that may develop into cavities (holes in teeth).
- Helps prevent premature tooth loss of baby teeth due to decay and overall assists in guiding the adult teeth to correct tooth eruption.
- Aids in the prevention of invasive dental treatment therefore reducing the amount of money spent on dental treatment
- Provides an overall community advantage, especially individuals from low socioeconomic communities, who have less access to other forms of fluoride treatments
- Evidence confirms that water fluoridation is a safe and effective way to help protect teeth against decay
- The addition of fluoride to the water does not alter the taste or smell of the drinking water
Fluoride therapy is often used to promote remineralisation. This produces the stronger and more acid-resistant fluorapatite, rather than the natural hydroxyapatite. Both materials are made of calcium. In fluorapatite, fluoride takes the place of a hydroxide.[12]
Effect of fluoride
The presence of fluoride in saliva and plaque fluid interacts with remineralisation process in many ways and thus exerts a topical or surface effect. A person living in an area with fluoridated water may experience rises of fluoride concentration in saliva to about 0.04 mg/L several times during a day.[13] Technically, this fluoride does not prevent cavities but rather controls the rate at which they develop making them take a lot longer and making them easier to prevent via normal brushing as it will take a higher amount of acid, usually built up over a number of days, to destroy the created fluorapatite.[14] When fluoride ions are present in plaque fluid along with dissolved hydroxyapatite, and the pH is higher than 4.5,[15] a fluorapatite-like remineralised veneer is formed over the remaining surface of the enamel; this veneer is much more acid-resistant than the original hydroxyapatite, and is formed more quickly than ordinary remineralised enamel would be.[1] The cavity-prevention effect of fluoride is partly due to these surface effects, which occur during and after tooth eruption.[16] Fluoride interferes with the process of tooth decay as fluoride intake during the period of enamel development for up to 7 years of age; the fluoride alters the structure of the developing enamel making it more resistant to acid attack. In children and adults when teeth are subjected to the alternating stages of demineralisation and remineralisation, the presence of fluoride intake encourages remineralisation and ensures that the enamel crystals that are laid down are of improved quality.[17] Fluoride is commonly found in toothpastes. Fluoride can be delivered to many parts of the oral cavity during brushing, including the tooth surface, saliva, soft tissues and remaining plaque biofilm.[18] Some remineralisation methods may work for "white spot lesions" but not necessarily "intact tooth surfaces".[19]
Fluoridated toothpaste
Regular use of a fluoridated toothpaste has been shown to provide a significant source of fluoride to the mouth by the means of direct fluoride contact to tooth structure.[20] The types of fluoride added to toothpaste include: sodium fluoride, sodium monofluorophosphate (MFP), and stannous fluoride.[21]
As stated previously, fluoride has been proven to positively affect the remineralisation process. Therefore, by using an adequately fluoridated toothpaste regularly, this assists the remineralisation process of any hard tooth tissues.
Fluoride varnish
Fluoride varnishes were developed late 1960s and early 1970s and since then they have been used both as a preventative agent in public health programs and as a specific treatment for patients at risk of caries by the 1980s, mostly in European countries.[20] Fluoride varnishes were developed primarily to overcome their shortcoming which is to prolong the contact time between fluoride and tooth surfaces.[20] Furthermore, when compared to other existing topical fluoride the advantages of fluoride varnishes application are being a quick and easy procedure for the clinicians, reduced discomfort for the receiving patients, and greater acceptability by the patients. Fluoride varnishes are a concentrated topical fluoride containing 5% sodium fluoride (NaF) except the fulour protector.[20] There are many types of fluoride varnishes and among them the popular brands are Duraphat and Fluor Protector. Currently, the anti-caries effect fluoride varnishes are backed up by Cochrane systematic reviews, 2002 which was updated in 2013 included 22 trails with 12,455 children aged 1–15 years old. The conclusion made is similar to its previous review, a 46% reduction in D(M)FS and 33% reduction in d (e/m)fs in permanent teeth and deciduous teeth respectively [20]
Water fluoridation
Community water fluoridation is the addition of fluoride in the drinking water with the aim of reducing tooth decay by adjusting the natural fluoride concentration of water to that recommended for improving oral health. The NHMRC released the public statement of efficacy and safety of fluoridation 2007 to set the recommended water fluoridation to the target range of 0.6 to 1.1 mg/L, depending on climate, to balance reduction of dental caries (tooth decay) and occurrence of dental fluorosis (mottling of teeth). Moreover the public statement states that the fluoridation of drinking water is an effective way to ensure the community is exposed to fluoride and can benefit from its preventative role in tooth decay.[22]
Plaque control
Oral hygiene practices involve the mechanical removal of plaque from hard tissue surfaces [23] Cariogenic bacteria levels in the plaque determine whether caries will occur or not, therefore, effective removal of plaque is paramount.[24] The removal of plaque inhibits demineralisation of teeth, and reversely increases opportunities for remineralisation.
Diet
Demineralization is caused by bacteria excreting acids as a product of their metabolism of carbohydrates. This occurs through the ingestion of acidic foods.[4] By reducing the intake frequency of acidic foods and fermentable carbohydrates in an individual's diet, the capacity for remineralization is increased and demineralization is decreased. Diet control is an important aspect in promoting remineralization to occur naturally. A decrease in the pH levels of the oral cavity is due to the organic acids that are produced by the presence of dietary carbohydrates. A loss of the tooth enamel structure and cavitation may occur if the demineralization phase continues for a long period of time. This disturbance of demineralisation caused by fermentable carbohydrates may continue until the pH returns to a normal level (pH of around 7).[25]
Increased sugar consumption in the means of foods and drinks containing high levels of sugar are known to be associated with high rates of dental decay. As a result, members of the dental team routinely assess patients' diets and highlight areas where this could be improved to reduce the risk of dental decay. A balanced diet is an important contributing factor towards oral health and general health. It is common knowledge that certain dietary habits contribute to disease, whether patients take note of advice which is given to them and change their diet as a result, is less certain.[26]
Recent studies on diet and caries have been confounded by the widespread use of fluoride toothpastes. Studies have argued that with greater exposure to fluoride, the sugar consumption/caries relationship may be weaker in the modern age than previously thought, with fluoride raising the threshold of sugar intake at which caries progresses to cavitation. It has been concluded in modern societies that a significant relationship between sugars and caries persists despite the regular widespread use of fluoride toothpaste.[27] Several reviews conclude that high sugar consumption continues to be the main threat for dental health of whole populations in some developed and many developing countries. Therefore, a key strategy to further reducing levels of caries in individuals as well as for populations, is by means of reducing the frequency of sugar intakes in the diet.
Foods high in refined carbohydrates, such as concentrated fruit snack bars, sweets, muesli bars, sweet biscuits, some breakfast cereals and sugary drinks including juices can contribute to dental decay, especially if eaten often and over long periods as the sugar nourishes the cariogenic bacteria in mouth. The bacteria produce acid, which destroys teeth. Highly refined packaged foods such as savory crackers and chips can also have high levels of carbohydrates. It is important to check the nutritional information panel on packaged foods to determine which foods and drinks have high carbohydrate concentrations.[28]
To prevent demineralisation in the mouth, it is important for an individual to ensure they have a well-balanced diet, including foods containing calcium and foods that are low in acids and sugars. The individual should have a diet high in fresh fruits and vegetables, wholegrain cereals, legumes, seeds and nuts. Sugary snacks including lollies, fruit bars, muesli bars, biscuits, dried fruit, cordials, juices and soft drinks should be limited as they contribute to dental decay and dental erosion. Additionally, excessive starchy foods (such as bread, pasta, and crackers), fruits and milk products consumed frequently can cause the growth of dental plaque and bacteria.[28] Therefore healthy eating, healthy drinking and proper maintenance of oral hygiene is the best way to promote and maintain sound tooth structure for an individual.
Xylitol
Xylitol is a natural sweetener, also known as a sugar alcohol.[11] Xylitol inhibits acid production by oral bacteria and promotes remineralisation of the teeth.[11] It can be found in various products which include chewing gums and lozenges. Xylitol has been found to reduce mutans strepococci in plaque and saliva and reduce the binding of these to the acquired enamel pellicle.[11] This in turn leads to less aherent plaque and a decrease in acid production.[11] In addition, chewing xylitol gum will stimulate increased salivary flow which in turn increases the amount of calcium in the saliva and enhances the oral clearance.
Additional saliva flow which includes chewing products such as gums that contain no fermentable carbohydrates can aid in the modulation of plaque pH. Sugar free xylitol is recommended for uses to prevent caries formation. Indeed, research has shown that the use of gum containing xylitol reduces plaque accumulation and gingival inflammation and enhances remineralisation process.[29]
See also
References
- 1 2 Featherstone, J. D. B. (2008). "Dental caries: A dynamic disease process". Australian Dental Journal. 53 (3): 286–291. doi:10.1111/j.1834-7819.2008.00064.x. PMID 18782377.
- ↑ Fejerskov, O., Nyvad, Bente, & Kidd, Edwina A. M. (2015). Dental caries : The disease and its clinical management (Third ed.).
- ↑ Cochrane NJ, Cai F, Huq NL, Burrow MF, Reynolds EC. New approaches to enhanced remineralization of tooth enamel. Journal of Dental Research. 2010 Nov 1;89(11):1187-97.
- 1 2 3 4 5 6 7 8 9 Li X, Wang J, Joiner A, Chang J. The remineralisation of enamel: a review of the literature. Journal of dentistry. 2014 Jun 30;42:S12-20.
- ↑ Garcia- Godoy, F. & Hicks, J. (2008). Maintaining the integrity of the enamel surface. American Dental Association, 139(3).
- ↑ Hicks J, Garcia-Godoy F, Flaitz C. Biological factors in dental caries: role of saliva and dental plaque in the dynamic process of demineralization and remineralization (part 1). Journal of Clinical Pediatric Dentistry. 2004 Sep 1;28(1):47-52.
- ↑ Featherstone JD. Dental caries: a dynamic disease process. Australian dental journal. 2008 Sep 1;53(3):286-91.
- ↑ Fejerskov O, Nyvad B, Kidd EA: Pathology of dental caries; in Fejerskov O, Kidd EAM (eds): Dental caries: The disease and its clinical management. Oxford, Blackwell Munksgaard, 2008, vol 2, pp 20-48.
- ↑ Soi S, Roy AS, Vinayak V. Fluorides and Their Role in Demineralization and Remineralization. Principal’s Message.:19.
- ↑ Nanci, A., & Ten Cate, A. (2008). Ten Cate's oral histology. St. Louis, Mo.: Mosby Elsevier.
- 1 2 3 4 5 6 García-Godoy, Franklin; Hicks, M. John (2008-05-01). "Maintaining the integrity of the enamel surface: The role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization". The Journal of the American Dental Association. 139, Supplement 2: 25S–34S. doi:10.14219/jada.archive.2008.0352.
- ↑ Better health channel. "Dental care - fluoride", April 2012. retrieved on 2016-04-15.
- ↑ Pizzo, G.; Piscopo, M. R.; Pizzo, I.; Giuliana, G. (2007). "Community Water Fluoridation and Caries Prevention: A Critical Review" (PDF). Clinical Oral Investigations. 11 (3): 189–193. doi:10.1007/s00784-007-0111-6. PMID 17333303.
- ↑ Aoba, T.; Fejerskov, O. (2002). "Dental Fluorosis: Chemistry and Biology". Critical Reviews in Oral Biology & Medicine. 13 (2): 155–70. doi:10.1177/154411130201300206. PMID 12097358.
- ↑ Cury, J. A.; Tenuta, L. M. A. (2008). "How to Maintain a Cariostatic Fluoride Concentration in the Oral Environment". Advances in Dental Research. 20 (1): 13–16. doi:10.1177/154407370802000104. PMID 18694871.
- ↑ Hellwig, E.; Lennon, Á. M. (2004). "Systemic versus Topical Fluoride". Caries Research. 38 (3): 258–262. doi:10.1159/000077764. PMID 15153698.
- ↑ Dr RS Levine. "The British Fluoridation Society", A guide to the action of fluoride in the prevention of dental decay, 2016. retrieved on 2016-05-3.
- ↑ Li, Xiaoke; Wang, Jinfang; Joiner, Andrew; Chang, Jiang. "The remineralisation of enamel: a review of the literature". Journal of Dentistry. 42: S12–S20. doi:10.1016/s0300-5712(14)50003-6.
- ↑ Iijima, Y. (2008). "Early detection of white spot lesions with digital camera and remineralization therapy". Australian Dental Journal. 53 (3): 274–280. doi:10.1111/j.1834-7819.2008.00062.x. PMID 18782375.
- 1 2 3 4 5 Beltrán-Aguilar, Goldstein, & Lockwood. (2000). Fluoride Varnishes: A Review of Their Clinical Use, Cariostatic Mechanism, Efficacy and Safety: A Review of Their Clinical Use, Cariostatic Mechanism, Efficacy and Safety. The Journal of the American Dental Association, 131(5), 589-596.
- ↑ Wiegand A, Bichsel D, Magalhães AC, Becker K, Attin T. Effect of sodium, amine and stannous fluoride at the same concentration and different pH on in vitro erosion. Journal of Dentistry. 2009 Aug 31;37(8):591-5.
- ↑ National health and medical research council. "Health effects of water fluoridation", 2016-04-06. retrieved on 2016-04-11.
- ↑ Darby ML, Walsh M. Dental hygiene: theory and practice. Elsevier Health Sciences; 2014 Apr 15.
- ↑ Hicks, John; Garcia-Godoy, Franklin; Flaitz, Catherine (2003-01-01). "Biological factors in dental caries: role of saliva and dental plaque in the dynamic process of demineralization and remineralization (part 1)". The Journal of Clinical Pediatric Dentistry. 28 (1): 47–52. doi:10.17796/jcpd.28.1.yg6m443046k50u20. ISSN 1053-4628. PMID 14604142.
- ↑ Arathi Rao, Neeraj Malhotra. "The Role of Remineralizing Agents in dentistry: A Review". Volume 32, Number 6. 2011. retrieved on 2016-05-22.
- ↑ Moynihan, Paula; Erik Petersen, Poul (2004). "Diet, nutrition and the prevention of dental diseases" (PDF). Public Health Nutrition. 7 (1a): 201–226. doi:10.1079/PHN2003589. Retrieved 22 May 2016.
- ↑ Cury, J; Tenuta, L (24 Jan 2014). "Evidence-based recommendation on toothpaste use". Brazilian Oral Research. 28. doi:10.1590/S1806-83242014.50000001. Retrieved 23 May 2016.
- 1 2 "Eating habits for a healthy smile and body" (PDF). The Journal Of The American Dental Association. 141 (12): 1544. Jan–Feb 2011. doi:10.1079/PHN2003589. Retrieved 22 May 2016.
- ↑ Humphrey, S. & Williamson, R. (2001). A review of saliva: Normal composition, flow, and function. The Journal Of Prosthetic Dentistry, 85(2), 162-169.
Further reading
- Chow, L. (2010). "Diffusion of Ions Between Two Solutions Saturated With Respect to Hydroxyapatite: A Possible Mechanism for Subsurface Demineralization of Teeth" (PDF). Journal of Research of the National Institute of Standards and Technology. National Institute of Science and Technology. 115 (4): 217–224. doi:10.6028/jres.115.015. PMC 2966276
 . PMID 21037801.
. PMID 21037801.