Receptive aphasia
| Receptive aphasia | |
|---|---|
 | |
| Broca's area and Wernicke's area | |
| Classification and external resources | |
| Specialty | psychiatry |
| ICD-10 | F80.2 |
| ICD-9-CM | 784.3 |
| MeSH | D001041 |
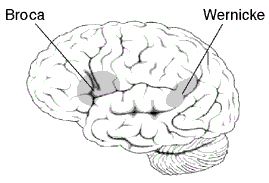
Receptive aphasia, also known as Wernicke's aphasia, fluent aphasia, or sensory aphasia, is a type of aphasia in which an individual is unable to understand language in its written or spoken form. Even though they can speak using grammar, syntax, rate, and intonation, they typically have difficulty expressing themselves meaningfully through speech. Receptive aphasia was named after Carl Wernicke who recognized this condition.[1] People with receptive aphasia are typically unaware of how they are speaking and do not realize their speech may lack meaning.[2] This is due to poor comprehension skills and the inability to understand their own speech because of overall self-monitoring deficits.[3] They typically remain unaware of even their most profound language deficits. When experienced with Broca's aphasia, the patient displays global aphasia.
Like many acquired language disorders, receptive aphasia can be experienced in many different ways and to many different degrees. While the typical case shows severely disturbed language comprehension, many individuals are still able to maintain conversations. Many may only experience difficulties with things such as accents and fast speech with the occasional speech error and can often carry out simple commands. Not all individuals show a complete loss of language comprehension. A common symptom of receptive aphasia is misinterpreting the meaning of words, gestures, pictures. For example, a patient with receptive aphasia may take the expression "it's raining cats and dogs" literally instead of figuratively.[2] What is described here is what is referred to as a "textbook" example with the typical, fully expressed symptoms.[4] Many diagnosed with Wernicke's aphasia have effortless speech and have difficulty with repetition in words and sentences. A person with Wernicke's aphasia may speak over others during conversation, which is "press of speech", and may not be aware that their message does not have a full meaning.[5]
Signs and symptoms
Receptive aphasia results from damage to Wernicke's area located posterior to the lateral sulcus in the left hemisphere of the brain. This area is adjacent to the auditory cortex. The damage is most often the result of a stroke, although damage to Wernicke's area through blunt force trauma from accidents is another possible cause.[4] While the onset of the disorder is typically very sudden, it is possible for the symptoms to begin gradually, with nonsensical utterances and word-finding issues appearing in the individual's speech.[4]
With receptive aphasia an individual primarily loses their ability to comprehend language. This typically takes the form of both an inability to understand speech as well as written text. They also lose the ability to understand their own spoken language. This inability to understand language is usually accompanied with symptoms of anosognosia: the individual is unaware of the disorder.[6] When attempting to communicate with others they often rely on situational cues in order to maintain the conversation. Individuals typically retain almost all of their cognitive abilities outside of those related to understanding language. Receptive aphasia, unlike expressive aphasia often occurs without any motor deficits.
Individuals with receptive aphasia often display symptoms of anomia (word-finding issues) and paraphasia, perhaps because of their difficulty understanding their own speech. A person with receptive aphasia speaks with normal prosody and intonation but uses random words, invents words, leaves out key words, substitutes words or verb tenses, pronouns, or prepositions, and utters sentences that do not make sense. Their expressive language is often devoid of any meaning. Other symptoms can include a loss of verbal pragmatic skills and conversational turn-taking.[7] A person with receptive aphasia is usually unaware of how much they are speaking, so they may continue to talk even when they should pause to allow others to speak; this is often referred to as "press of speech."[2] Despite their difficulties in forming sentences that make sense, they do speak fluently. Sentences are typically grammatically correct. This fluent but nonsensical speech is often referred to as "word salad". The juxtaposition between fluent speech and the lack of meaning is characteristic of receptive aphasia.[8][9] Patients also display logorrhoea, a nonstop output of words during spontaneous speech. The rate of speech errors produced is variable, with some patients showing only 10% of productions being errors and others showing up to 80% of speech production being incorrect.[4]
Below is an example of an interaction between an individual with severe receptive aphasia and a clinician:
- Q. "What is your speech problem?"
- A. "Because no one gotta scotta gowan thwa, thirst, gell, gerst, derund, gystrol, that's all."
- Q. "What does "swell-headed" mean?"
- A. "She is selfice on purpiten."[4]
Below is an example of spontaneous speech from the same individual showing logorrhea symptoms:
- "Then he graf, so I'll graf, I'm giving ink, no gerfergen, in pane, I can't grasp, I haven't grob the grabben, I'm going to the glimmeril, let me go."
- "What my fytisset for, whattim tim saying got dok arne gimmin my suit, suit ti Friday ... I ayre here what takes zwei the cuppen seffer effer sepped ... I spoke on she asked for clubbin hond here, you what, what kind of a siz sizzen ... and she speaks all the friend and all is in my herring."[4]
As a result, these individuals often display logorrhea, a nonstop output of speech.[7]
Words that are affective and more associated with emotions are retained.[10] The ability to utter profanity is therefore unaffected due to the typical association of profanity with emotional outbursts and emphasis, rather than with the meaning of the word itself.
If Wernicke's area is damaged in the non-dominant hemisphere, the syndrome resulting will be sensory dysprosody—the inability to perceive the pitch, rhythm, and emotional tone of speech. This difference in impairment between left and right hemisphere lesions is caused by functional asymmetry; the designation of specific brain functions to either the left or right hemisphere. The main lateralized speech functions of the right hemisphere are the regulation, perception, and production of melodic speech—thereby causing right-hemisphere lesions to impair prosody. Furthermore, dysprosody also impairs the ability to interpret melodies, the ability to differentiate between male and female voices, and the ability to recognize familiar noises. Dysprosodic patients also experience exaggerated pathological emotional outbursts, despite showing less emotion through facial expressions. Dysprosody is believed to be an impairment to the ability to encode non-verbal information, as opposed to a cognitive deficit or an inability to experience emotion.[11]
Patients who communicated using sign language before the onset of the aphasia experience analogous symptoms.[12]
Causes
Receptive aphasia is traditionally associated with neurological damage to Wernicke's area in the brain[13] (Brodmann area 22, in the posterior part of the superior temporal gyrus of the dominant hemisphere). Since Wernicke's area is responsible for "reading, thinking of what to write, and processing information", that is where we see many of the deficits associated with damage to this area.[14] However, the key deficits of receptive aphasia do not come from damage to Wernicke's area;[13] instead, most of the core difficulties are proposed to come from damage to the medial temporal lobe and underlying white matter. Receptive aphasia results from damage in the posterior one-third of the superior gyrus of the temporal lobe of the left hemisphere. Damage in this area not only destroys local language regions but also cuts off most of the occipital, temporal, and parietal regions from the core language region.[15] While Wernicke's area is the site of language recognition, perception, interpretations, and understanding, that does not mean that it is wholly responsible for the comprehension of semantic meaning. Attempts to localize "receptive" language modules are generally futile, given the full range of interpretations of "receptive functionality". As Dennis C. Tanner states, "Although there may be … areas important in perceiving vowels and consonants, pinpointing the brain cells … [for] understanding the implications of a Robert Frost poem is absurd." The reason for this is due to the many levels of semantic understanding—auditory perception, speech discrimination, denotative extraction, and dynamic symbolism. The process of full-depth semantic decoding has the capacity to engage virtually the whole brain. Therefore, it is more apt to think of Wernicke's area as an important conduit for a larger, all-encompassing process.[16]
Assessment
Receptive aphasia can be difficult to diagnose as the symptoms can be mistaken as a confused state due to stroke or blunt force trauma. In order for receptive aphasia to be diagnosed a complete language examination, especially of the auditory system, must be done. There are various diagnostic tests and measures used to determine whether a patient should be diagnosed with receptive aphasia.[4]
Some examples of these assessments can be seen below:
- Formal screening and bedside tests of aphasia are shorter examinations that determine the presence or absence of aphasia. Some examples of these tests are: the Bedside Evaluation Screening Test, Second Edition (BEST-2; Fitch-West & Sands, 1998); the Aphasia Screening Test (AST; Whurr, 1996); and the Quick Assessment for Aphasia (Tanner & Culbertson, 1999).[17]
- Once a physician determines that aphasia is a possible diagnosis, more comprehensive evaluations are done to determine the type of aphasia. These assessments are standardized aphasia test batteries and include: the Boston Diagnostic Aphasia Examination (BDAE-3; Goodglass et al., 2000); the Porch Index of Communicative Abilities (PICA; Porch, 1981); and the Western Aphasia Battery (WAB; Kertesz, 1982).[17]
- In order to diagnose a patient with receptive aphasia, auditory comprehension should be assessed thoroughly because it is one of the most affected areas. Auditory comprehension can be assessed using the Functional Auditory Comprehension Test (FACT; LaPointe & Horner, 1978), the Revised Token Test (McNeil & Prescott, 1978) and through real-life conversations with patients.[18]
- In addition to the aforementioned tests, reading comprehension and written language can be used to indicate the presence of receptive aphasia, although there are limited standardized assessment devices in this area.[18]
During assessment, clinicians evaluate the patient's initial functioning and performance on the above tasks to form a baseline for treatment. This baseline can help them decide what type of treatment they can use and compare the patient's future progress with their initial abilities.[17]
Treatment
Many sources agree that patients often do not seek treatment due to their anosognosia and therefore lack of awareness that they could benefit from therapy.[14][17] This apparent lack of concern surrounding their symptoms needs to be addressed before treatment can be initiated. In order for the treatment to be helpful, patients need to be cooperative and engaged in their therapy. Because each case of receptive aphasia presents itself differently, the treatment options are varied and use multiple techniques. Speech-language pathologists work to create therapeutic programs that are functional and effective for receptive aphasia patients. The patient's likelihood and prognosis of recovery is dependent upon their severity of symptoms and whether they maintained any auditory comprehension abilities. Across the range of symptoms in receptive aphasia, a patient's auditory comprehension deficits and poor self-monitoring must be initially addressed so that the patient can participate in language-based activities.[17][18]
Furthermore, the type of auditory deficit found in a case of Wernicke's aphasia has been shown to be responsive to treatment of short term memory and working memory. Short term memory is used for verbal comprehension when a sentence must be mentally "repeated" in order to fully understand its content. Working memory is for a "second pass", after meaning is encoded. This is done in order to identify pronouns, to "act out" the meaning of the sentence mentally, to check that action for plausibility against long term memory, and to check meaning against syntax. After treatment to increase both short term memory and working memory, a patient with an auditory deficit characteristic of Wernicke's aphasia was able to recall far more words than previously possible, and began to include verbs in her recollections when prior to treatment she had included virtually no verbs. This variety of treatment focused on increasing memory in order to aid sentence comprehension appears promising.[19]
Comprehension training
Comprehension deficits as well as issues of pressure of speech can be improved through comprehension training. Comprehension training confronts the issues of pressure of speech by redirecting patients attention to listening rather than speaking. In this training the clinician will give the patient short instructions with contextual cues (such as facial expressions and gestures) and remind the patient to stop speaking while listening to these instructions through the use of these cues.[18] The comprehension tasks used in this training involve listening to short, context-dependent instructions given by a clinician and initially responding by pointing to an object or picture. These tasks become gradually more difficult as therapy continues. The main goal of this therapy is to enhance patient's attention towards incoming information while simultaneously slowing and monitoring his or her own speech output.[17] Therapists using this contextual approach have found they can increase speech comprehension from 2% to 90%.[14]
Schuell's stimulation
Schuell's stimulation is a well-known treatment, and is the most effective treatment. This treatment involves introducing the patient to strong, controlled, and intensive auditory stimulation. This immersion into intensive auditory stimulation is believed to increase neuronal firing causing an increase in neural activation. This neural activation is used as a facilitator to increase brain reorganization and therefore recovery of language in the patient.[17]
Redistribution of brain activation allows uninjured parts of the brain, such as the frontal and right hemisphere to compensate for the injuries found in Wernicke's area. On comprehension tasks, the average person shows activation in Broca and Wernicke's areas in the left hemisphere of the brain with little activation in the right hemisphere. In contrast, a patient with receptive aphasia shows activation in the right hemisphere of the brain, providing evidence that neuroplasticity plays a role in recovery.[17][18][20]
Social approach
The social approach involves a collaborative effort on behalf of patients and clinicians to determine goals for therapy and also determining the most important functional outcomes that could improve the patient's everyday life. A conversational approach which is thought to provide opportunities for development and use of strategies to overcome barriers to communication.The main goals of this treatment are to improve the patient's conversational confidence and skills using conversational coaching, supported conversations, and partner training.[17]
- Conversational coaching involves aphasic patients and their speech language pathologists, who serve as a "coach" discussing strategies to approach various communicative scenarios. The "coach" will help the patient develop a script for a scenario (such as ordering food at a restaurant), and help the patient practice and perform the scenario in and out of the clinic while evaluating the outcome.
- Supported conversation also involves using a communicative partner who supports the patient's learning by providing contextual cues, slowing their own rate of speech, and increasing their message's redundancy to promote the patient's comprehension.
- Promoting Aphasics Communicative Effectiveness (PACE) encourages conversation outside the clinic.
Successful treatment incorporates these various treatment programs and approaches to facilitate patient's learning. In order to improve self-monitoring speech language pathologists will slow their own rate of speech, pausing between meaningful segments and encourage patients to do the same, slowing down their own speech, listening to themselves speak and monitoring their speech output.[17]
It is also important to include patient's families in treatment programs so they can have speaking partners where they communicate the most, at home. Clinicians can teach family members how to support one another and adjust their speaking patterns to further facilitate their loved one's treatment and rehabilitation.[17]
Luria's theory
Alexander Luria proposed that this type of aphasia has three characteristics.[21]
- A deficit in the categorization of sounds. In order to hear and understand what is said, one must be able to recognize the different sounds of spoken language. For example, hearing the difference between bad and bed is easy for native English speakers. The Dutch language, however, makes a much greater difference in pronunciation between these vowels, and therefore the Dutch have difficulties hearing the difference between them in English pronunciation. This problem is exactly what patients with Wernicke's aphasia have in their own language: they cannot isolate significant sound characteristics and classify them into known meaningful systems.
- A defect in speech. A patient with Wernicke's aphasia can and may speak a great deal, but he or she confuses sound characteristics, producing "word salad" in extreme cases: intelligible words that appear to be strung together randomly.
- An impairment in writing. A person who cannot discern sounds cannot be expected to write.
See also
- Aphasia
- Expressive aphasia
- Schizophasia
- Conduction aphasia
- Logorrhea
- Agraphia
- Paragrammatism
- Transcortical sensory aphasia
- Wernicke-Korsakov syndrome
- Broca's aphasia
References
- ↑ Wernicke's APHASIA. Caspari, Isabelle LaPointe, Leonard L. , (2005).Aphasia and related neurogenic language disorders (3rd ed.)., (pp. 142–154). New York, NY, US: Thieme New York, xix, 274 pp
- 1 2 3 ASHA: American Speech and Language Association http://www.asha.org/Practice-Portal/Clinical-Topics/Aphasia/Common-Classifications-of-Aphasia/[]
- ↑ "American Speech-Language Hearing Association". American Speech-Language Hearing Association Practice Portal. American Speech-Language Hearing Association. Retrieved 12/1/16. Check date values in:
|access-date=(help) - 1 2 3 4 5 6 7 Brown, Jason (1972). Aphasia, Apraxia, and Agnosia Clinical and Theoretical Aspects. Springfield, Illinois: Charles C Thomas Publisher. pp. 56–71. ISBN 0-398-02211-9.
- ↑ "Common Classifications of Aphasia". www.asha.org. Retrieved 2016-12-03.
- ↑ Manasco, M. Hunter (2014). Neurogenic Communication Disorders. Jones & Bartlett Learning. p. 83. ISBN 978-0-7637-9417-0.
- 1 2 Manasco, Hunter. "The Aphasias". Introduction to Neurogenic Communication Disorders. p. 93.
- ↑ Elias, Lorin; Saucer, Debourah (2006). Neuropsychology: Clinical and Experimental Foundations. Boston: Pearson. ISBN 0-205-34361-9.
- ↑ Parker, Timothy (2012). Foundations of Biological Psychology. Ronkonkoma: Linus Publications. ISBN 1-60797-325-1.
- ↑ Jay, Timothy (2003). The Psychology of Language. New Jersey: Prentice Hall. p. 35. ISBN 0-13-026609-4.
- ↑ Dyukova, G. M.; Glozman, Zh. M.; Titova, E. Yu.; Kriushev, E. S.; Gamaleya, A. A. (2010). "Speech Disorders in Right-Hemisphere Stroke". Neuroscience and Behavioral Physiology. 40 (6): 593–602. doi:10.1007/s11055-010-9301-9. PMID 20532830.
- ↑ http://pages.slc.edu/~ebj/IM_97/Lecture10/L10.html[]
- 1 2 Kolb & Whishaw: Fundamentals of Human Neuropsychology (2003) page 505
- 1 2 3 http://www.theaphasiacenter.com/2012/01/what-is-wernickes-aphasia/
- ↑ Kolb & Whishaw: Fundamentals of Human Neuropsychology (2003) page 506
- ↑ Tanner, Dennis C. (2007). "A redefining Wernicke's area: receptive language and discourse semantics". Journal of Allied Health. 36 (2): 63–6. PMID 17633961.
- 1 2 3 4 5 6 7 8 9 10 11 LaPointe, Leonard (2005). Aphasia and Related Neurogenic Language Disorders (Third ed.). Thieme. pp. 149–152. ISBN 1-58890-226-9.
- 1 2 3 4 5 Vinson, Betsy (2012). Language Disorders Across the Lifespan. Clifton Park, NY: Delmar, Cengage Learning. pp. 572–576. ISBN 978-1-4354-9859-4.
- ↑ Francis, Dawn; Clark, Nina; Humphreys, Glyn (2003). "The treatment of an auditory working memory deficit and the implications for sentence comprehension abilities in mild "receptive" aphasia". Aphasiology. 17 (8): 723–50. doi:10.1080/02687030344000201.
- ↑ Code, Chris (1987). Language Aphasia and the Right Hemisphere. Great Britain: John Wiley & Sons Ltd. p. 110. ISBN 0471911585.
- ↑ Kolb & Whishaw: Fundamentals of Human Neuropsychology (2003), pages 503-504. The whole paragraph on Luria's theory is written with help of this reference.
Further reading
- Klein, Stephen B., and Thorne. Biological Psychology. New York: Worth, 2007. Print.
- Saladin, Kenneth S. Anatomy & Physiology: the Unity of Form and Function. New York: McGraw-Hill Higher Education, 2010. Print.
External links
- Aphasia Center of California in Oakland, CA, U.S.