Pyrazinamide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Rifater |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682402 |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | J04AK01 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | >90% |
| Metabolism | Hepatic |
| Biological half-life | 9 to 10 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number |
98-96-4 |
| PubChem (CID) | 1046 |
| IUPHAR/BPS | 7287 |
| DrugBank |
DB00339 |
| ChemSpider |
1017 |
| UNII |
2KNI5N06TI |
| KEGG |
D00144 |
| ChEBI |
CHEBI:45285 |
| ChEMBL |
CHEMBL614 |
| NIAID ChemDB | 007697 |
| ECHA InfoCard | 100.002.470 |
| Chemical and physical data | |
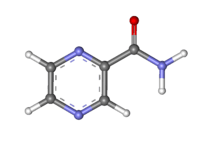
| Formula | C5H5N3O |
| Molar mass | 123.113 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Pyrazinamide is a drug used to treat tuberculosis. The drug is largely bacteriostatic, but can be bacteriocidal on actively replicating tuberculosis bacteria.
It is on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.[1]
Medical uses
Pyrazinamide is only used in combination with other drugs such as isoniazid and rifampicin in the treatment of Mycobacterium tuberculosis. It is never used on its own. It has no other indicated medical uses. In particular, it is not used to treat other mycobacteria; Mycobacterium bovis and Mycobacterium leprae are innately resistant to pyrazinamide. Pyrazinamide is used in the first two months of treatment to reduce the duration of treatment required.[2] Regimens not containing pyrazinamide must be taken for nine months or more.
Pyrazinamide in conjunction with rifampin is a preferred treatment for latent tuberculosis.[3]
Pyrazinamide is a potent antiuricosuric drug[4] and consequently has an off-label use in the diagnosis of causes of hypouricemia and hyperuricosuria.[5] It acts on URAT1.[5]
Adverse effects
The most common (approximately 1%) side effect of pyrazinamide is joint pains (arthralgia), but this is not usually so severe that patients need to stop taking the pyrazinamide.[6][7] Pyrazinamide can precipitate gout flares by decreasing renal excretion of uric acid.[8]
The most dangerous side effect of pyrazinamide is hepatotoxicity, which is dose related. The old dose for pyrazinamide was 40–70 mg/kg daily and the incidence of drug-induced hepatitis has fallen significantly since the recommended dose has been reduced. In the standard four-drug regimen (isoniazid, rifampicin, pyrazinamide, ethambutol), pyrazinamide is the most common cause of drug-induced hepatitis.[9] It is not possible to clinically distinguish pyrazinamide-induced hepatitis from hepatitis caused by isoniazid or rifampicin; test dosing is required (this is discussed in detail in tuberculosis treatment)
Other side effects include nausea and vomiting, anorexia, sideroblastic anemia, skin rash, urticaria, pruritus, dysuria, interstitial nephritis, malaise; rarely porphyria, and fever.
Pharmacokinetics
Pyrazinamide is well absorbed orally. It crosses inflamed meninges and is an essential part of the treatment of tuberculous meningitis. It is metabolised by the liver and the metabolic products are excreted by the kidneys.
Pyrazinamide is routinely used in pregnancy in the UK and the rest of the world; the WHO recommend its use in pregnancy; and there is extensive clinical experience to show that it is safe. In the U.S., pyrazinamide is not used in pregnancy, citing insufficient evidence of safety.[10] Pyrazinamide is removed by haemodialysis and therefore doses should always be given at the end of a dialysis session.
Mechanism of action
Pyrazinamide is a prodrug that stops the growth of Mycobacterium tuberculosis.
Pyrazinamide diffuses into the granuloma of M. tuberculosis, where the tuberculosis enzyme pyrazinamidase converts pyrazinamide to the active form pyrazinoic acid.[11] Under acidic conditions of pH 5 to 6, the pyrazinoic acid that slowly leaks out converts to the protonated conjugate acid, which is thought to diffuse easily back into the bacilli and accumulate. The net effect is that more pyrazinoic acid accumulates inside the bacillus at acid pH than at neutral pH.[12][11]
Pyrazinoic acid was thought to inhibit the enzyme fatty acid synthase (FAS) I, which is required by the bacterium to synthesise fatty acids[13] although this has been discounted.[14][15] It was also suggested that the accumulation of pyrazinoic acid disrupts membrane potential and interferes with energy production, necessary for survival of M. tuberculosis at an acidic site of infection. Pyrazinoic acid also binds to the ribosomal protein S1 (RpsA) and inhibits trans-translation, which may explain the ability of the drug to kill dormant mycobacteria.[16]
Resistance
Mutations in the pncA gene of tuberculosis, which encodes a pyrazinamidase and converts pyrazinamide to its active form, is responsible for the appearance of most pyrazinamide resistant M. tuberculosis strains.[17] A few pyrazinamidase resistant strains with mutations in the rpsA gene have also been identified.[16] There are currently three main methods of testing for pyrazinamide resistance: 1) phenotypic tests where a tuberculosis strain is grown in the presence of increasing concentrations of pyrazinamide, 2) measuring levels of pyrazinamidase enzyme produced by the tuberculosis strain, or 3) looking for mutations in the pncA gene of tuberculosis.[11]
Global resistance of tuberculosis to pyrazinamide has been estimated to be in 16% of all cases, and 60% of people with multi drug-resistant tuberculosis.[11]
Abbreviations
The abbreviations PZA and Z are standard, and used commonly in the medical literature, although best practice discourages the abbreviating of drug names to prevent mistakes.
Presentation
Pyrazinamide is a generic drug, and is available in a wide variety of presentations. Pyrazinamide tablets form the bulkiest part of the standard tuberculosis treatment regimen. Pyrazinamide tablets are so large, some people find them impossible to swallow: pyrazinamide syrup is an option.
Pyrazinamide is also available as part of fixed-dose combinations with other TB drugs such as isoniazid and rifampicin (Rifater is an example).
History
Pyrazinamide was first discovered and patented in 1936 but not used against tuberculosis until 1952.[18] Its discovery as an anti-tubercular agent was remarkable since it has no activity against tuberculosis in-vitro, due to not being active at a neutral pH, so would ordinarily not be expected to work in-vivo.[19] However, it was known that nicotinamide had activity against tuberculosis and pyrazinamide was thought to have a similar effect. Experiments in mice at Lederle and Merck confirmed its ability to kill tuberculosis and it was rapidly used in humans.[19]
References
- ↑ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ Hong Kong Chest Service, Medical Research Council (1981). "Controlled trial of four thrice weekly regimens and a daily regimen given for 6 months for pulmonary tuberculosis". Lancet. 1 (8213): 171–4. doi:10.1016/S0140-6736(02)95623-0. PMID 6109855.
- ↑ Centers for Disease Control and Prevention (2000). "Targeted tuberculin testing and treatment of latent tuberculosis infection". MMWR. 49 (RR–6): 31–32. PMID 10881762.
- ↑ Spaia S, Magoula I, Tsapas G, Vayonas G (2000). "Effect of pyrazinamide and probenecid on peritoneal urate transport kinetics during continuous ambulatory peritoneal dialysis". Perit Dial Int. 20 (1): 47–52. PMID 10716583.
- 1 2 Ichida K, Hosoyamada M, Hisatome I, Enomoto A, Hikita M, Endou H, Hosoya T (January 2004). "Clinical and molecular analysis of patients with renal hypouricemia in Japan-influence of URAT1 gene on urinary urate excretion". J. Am. Soc. Nephrol. 15 (1): 164–73. doi:10.1097/01.ASN.0000105320.04395.D0. PMID 14694169.
- ↑ East and Central African/Medical Research Council Fifth Collaborative Study (1983). "Controlled clinical trial of 4 short-course regimens of chemotherapy (three 6-month and one 9-month) for pulmonary tuberculosis". Tubercle. 64 (3): 153–166. doi:10.1016/0041-3879(83)90011-9. PMID 6356538.
- ↑ British Thoracic Society (1984). "A controlled trial of 6 months chemotherapy in pulmonary tuberculosis, final report: results during the 36 months after the end of chemotherapy and beyond". Br J Dis Chest. 78 (4): 330–336. doi:10.1016/0007-0971(84)90165-7. PMID 6386028.
- ↑ American Thoracic Society; CDC; Infectious Diseases Society of America. (Jun 20, 2003). "Treatment of tuberculosis.". MMWR Recomm Rep. 52 (RR-11): 1–77. PMID 12836625.
- ↑ Yee D, et al. (2003). "Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis". Am J Respir Crit Care Med. 167 (11): 1472–7. doi:10.1164/rccm.200206-626OC. PMID 12569078.
- ↑ American Thoracic Society, Centers for Disease Control, Infectious Diseases Society of America (2003). "Treatment of Tuberculosis". Am J Respir Crit Care Med. 167: 602–662. doi:10.1164/rccm.167.4.603.
- 1 2 3 4 Whitfield, Michael G.; Soeters, Heidi M.; Warren, Robin M.; York, Talita; Sampson, Samantha L.; Streicher, Elizabeth M.; Helden, Paul D. van; Rie, Annelies van (2015-07-28). "A Global Perspective on Pyrazinamide Resistance: Systematic Review and Meta-Analysis". PLOS ONE. 10 (7): e0133869. doi:10.1371/journal.pone.0133869. ISSN 1932-6203. PMC 4517823
 . PMID 26218737.
. PMID 26218737. - ↑ Zhang Y, Mitchison D (January 2003). "The curious characteristics of pyrazinamide: a review". Int. J. Tuberc. Lung Dis. 7 (1): 6–21. PMID 12701830.
- ↑ Zimhony O, Cox JS, Welch JT, Vilchèze C, Jacobs WR (2000). "Pyrazinamide inhibits the eukaryotic-like fatty acid synthetase I (FASI) of Mycobacterium tuberculosis" (abstract). Nature Medicine. 6 (9): 1043–47. doi:10.1038/79558. PMID 10973326.
- ↑ Boshoff HI, Mizrahi V, Barry CE (2002). "Effects of Pyrazinamide on Fatty Acid Synthesis by Whole Mycobacterial Cells and Purified Fatty Acid Synthase I". Journal of Bacteriology. 184 (8): 2167–72. doi:10.1128/JB.184.8.2167-2172.2002. PMC 134955
 . PMID 11914348.
. PMID 11914348. - ↑ Zhang, Ying; Mitchison, Denis; Shi, Wanliang; Zhang, Wenhong. "Mechanisms of Pyrazinamide Action and Resistance". Microbiology Spectrum. 2 (4). doi:10.1128/microbiolspec.mgm2-0023-2013.
- 1 2 Shi W, Zhang X, Jiang X, Yuan H, Lee JS, Barry CE, et al. (2011). "Pyrazinamide inhibits trans-translation in Mycobacterium tuberculosis". Science. 333 (6049): 1630–1632. doi:10.1126/science.1208813. PMC 3502614
 . PMID 21835980.
. PMID 21835980. - ↑ Scorpio A, Zhang Y (1996). "Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus". Nature Medicine. 2 (6): 662–7. doi:10.1038/nm0696-662. PMID 8640557.
- ↑ Zhang, Ying; Mitchison, Denis; Shi, Wanliang; Zhang, Wenhong. "Mechanisms of Pyrazinamide Action and Resistance". Microbiology Spectrum. 2 (4). doi:10.1128/microbiolspec.mgm2-0023-2013.
- 1 2 Zhang, Y.; Mitchison, D. (2003-01-01). "The curious characteristics of pyrazinamide: a review". The International Journal of Tuberculosis and Lung Disease: The Official Journal of the International Union Against Tuberculosis and Lung Disease. 7 (1): 6–21. ISSN 1027-3719. PMID 12701830.