Foodborne illness
 | |
| Terms | |
|---|---|
| Foodborne illness | |
| Hazard analysis and critical control points (HACCP) • Hazard analysis and risk-based preventive controls (HARPC) | |
| Critical control point | |
| Critical factors | |
| FAT TOM | |
| pH | |
| Water activity (aw) | |
| Bacterial pathogens | |
| Clostridium botulinum | |
| Escherichia coli | |
| Listeria | |
| Salmonella | |
| Vibrio cholerae | |
| Viral pathogens | |
| Enterovirus | |
| Hepatitis A | |
| Norovirus | |
| Rotavirus | |
| Parasitic pathogens | |
| Cryptosporidium | |
| Entamoeba histolytica | |
| Giardia | |
| Trichinella | |
Foodborne illness (also foodborne disease and colloquially referred to as food poisoning)[1] is any illness resulting from the food spoilage of contaminated food, pathogenic bacteria, viruses, or parasites that contaminate food,[2] as well as chemical or natural toxins such as poisonous mushrooms and various species of beans that have not been boiled for at least 10 minutes.
Symptoms vary depending on the cause, and are described below in this article. A few broad generalizations can be made, e.g.: The incubation period ranges from hours to days, depending on the cause and on how much was consumed. The incubation period tends to cause sufferers to not associate the symptoms with the item consumed, and so to cause sufferers to attribute the symptoms to gastroenteritis for example. Symptoms often include vomiting, fever, and aches, and may include diarrhea. Bouts of vomiting can be repeated with an extended delay in between, because even if infected food was eliminated from the stomach in the first bout, microbes (if applicable) can pass through the stomach into the intestine via cells lining the intestinal walls and begin to multiply. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade deeper body tissues.
Causes

Foodborne illness usually arises from improper handling, preparation, or food storage. Good hygiene practices before, during, and after food preparation can reduce the chances of contracting an illness. There is a consensus in the public health community that regular hand-washing is one of the most effective defenses against the spread of foodborne illness. The action of monitoring food to ensure that it will not cause foodborne illness is known as food safety. Foodborne disease can also be caused by a large variety of toxins that affect the environment.[3]
Foodborne illness can also be caused by pesticides or medicines in food and naturally toxic substances such as poisonous mushrooms or reef fish.
Bacteria
Bacteria are a common cause of foodborne illness. In the United Kingdom during 2000, the individual bacteria involved were the following: Campylobacter jejuni 77.3%, Salmonella 20.9%, Escherichia coli O157:H7 1.4%, and all others less than 0.56%.[4] In the past, bacterial infections were thought to be more prevalent because few places had the capability to test for norovirus and no active surveillance was being done for this particular agent. Toxins from bacterial infections are delayed because the bacteria need time to multiply. As a result, symptoms associated with intoxication are usually not seen until 12–72 hours or more after eating contaminated food. However, in some cases, such as Staphylococcal food poisoning, the onset of illness can be as soon as 30 minutes after ingesting contaminated food.[5]
Most common bacterial foodborne pathogens are:
- Campylobacter jejuni which can lead to secondary Guillain–Barré syndrome and periodontitis[6]
- Clostridium perfringens, the "cafeteria germ"[7]
- Salmonella spp. – its S. typhimurium infection is caused by consumption of eggs or poultry that are not adequately cooked or by other interactive human-animal pathogens[8][9][10]
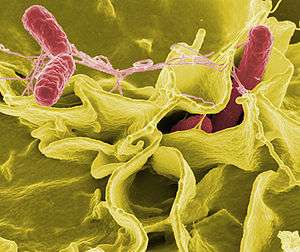 Salmonella
Salmonella - Escherichia coli O157:H7 enterohemorrhagic (EHEC) which can cause hemolytic-uremic syndrome
Other common bacterial foodborne pathogens are:
- Bacillus cereus
- Escherichia coli, other virulence properties, such as enteroinvasive (EIEC), enteropathogenic (EPEC), enterotoxigenic (ETEC), enteroaggregative (EAEC or EAgEC)
- Listeria monocytogenes
- Shigella spp.
- Staphylococcus aureus
- Staphylococcal enteritis
- Streptococcus
- Vibrio cholerae, including O1 and non-O1
- Vibrio parahaemolyticus
- Vibrio vulnificus
- Yersinia enterocolitica and Yersinia pseudotuberculosis
Less common bacterial agents:
- Brucella spp.
- Corynebacterium ulcerans
- Coxiella burnetii or Q fever
- Plesiomonas shigelloides
Enterotoxins
In addition to disease caused by direct bacterial infection, some foodborne illnesses are caused by enterotoxins (exotoxins targeting the intestines). Enterotoxins can produce illness even when the microbes that produced them have been killed. Symptom appearance varies with the toxin but may be rapid in onset, as in the case of enterotoxins of Staphylococcus aureus in which symptoms appear in one to six hours.[11] This causes intense vomiting including or not including diarrhea (resulting in staphylococcal enteritis), and staphylococcal enterotoxins (most commonly staphylococcal enterotoxin A but also including staphylococcal enterotoxin B) are the most commonly reported enterotoxins although cases of poisoning are likely underestimated.[12] It occurs mainly in cooked and processed foods due to competition with other biota in raw foods, and humans are the main cause of contamination as a substantial percentage of humans are persistent carriers of S. aureus.[12] The CDC has estimated about 240,000 cases per year in the United States.[13]
The rare but potentially deadly disease botulism occurs when the anaerobic bacterium Clostridium botulinum grows in improperly canned low-acid foods and produces botulin, a powerful paralytic toxin.
Pseudoalteromonas tetraodonis, certain species of Pseudomonas and Vibrio, and some other bacteria, produce the lethal tetrodotoxin, which is present in the tissues of some living animal species rather than being a product of decomposition.
Emerging foodborne pathogens
Many foodborne illnesses remain poorly understood.
- Aeromonas hydrophila, Aeromonas caviae, Aeromonas sobria
Preventing bacterial food poisoning

Prevention is mainly the role of the state, through the definition of strict rules of hygiene and a public services of veterinary surveying of animal products in the food chain, from farming to the transformation industry and delivery (shops and restaurants). This regulation includes:
- traceability: in a final product, it must be possible to know the origin of the ingredients (originating farm, identification of the harvesting or of the animal) and where and when it was processed; the origin of the illness can thus be tracked and solved (and possibly penalized), and the final products can be removed from the sale if a problem is detected;
- enforcement of hygiene procedures such as HACCP and the "cold chain";
- power of control and of law enforcement of veterinarians.
In August 2006, the United States Food and Drug Administration approved Phage therapy which involves spraying meat with viruses that infect bacteria, and thus preventing infection. This has raised concerns, because without mandatory labelling consumers would not be aware that meat and poultry products have been treated with the spray.[14]
At home, prevention mainly consists of good food safety practices. Many forms of bacterial poisoning can be prevented by cooking it sufficiently, and either eating it quickly or refrigerating it effectively.[2] Many toxins, however, are not destroyed by heat treatment.
Techniques that help prevent food borne illness in the kitchen are hand washing, rinsing produce,[15] preventing cross-contamination, proper storage, and maintaining cooking temperatures. In general, freezing or refrigerating prevents virtually all bacteria from growing, and heating food sufficiently kills parasites, viruses, and most bacteria. Bacteria grow most rapidly at the range of temperatures between 40 °F and 140 °F, called the "danger zone". Storing food below or above the "danger zone" can effectively limit the production of toxins. For storing leftovers, the food must be put in shallow containers for quick cooling and must be refrigerated within two hours. When food is reheated, it must reach an internal temperature of 165 °F (74 °C) or until hot or steaming to kill bacteria.[16]
Mycotoxins and alimentary mycotoxicoses
The term alimentary mycotoxicoses refers to the effect of poisoning by Mycotoxins (The term 'mycotoxin' is usually reserved for the toxic chemical products produced by fungi that readily colonize crops) through food consumption. Mycotoxins sometimes have important effects on human and animal health. For example, an outbreak which occurred in the UK in 1960 caused the death of 100,000 turkeys which had consumed aflatoxin-contaminated peanut meal. In the USSR in World War II, 5,000 people died due to Alimentary Toxic Aleukia (ALA).[17] The common foodborne Mycotoxins include:
- Aflatoxins – originated from Aspergillus parasiticus and Aspergillus flavus. They are frequently found in tree nuts, peanuts, maize, sorghum and other oilseeds, including corn and cottonseeds. The pronounced forms of Aflatoxins are those of B1, B2, G1, and G2, amongst which Aflatoxin B1 predominantly targets the liver, which will result in necrosis, cirrhosis, and carcinoma.[18][19] In the US, the acceptable level of total aflatoxins in foods is less than 20 μg/kg, except for Aflatoxin M1 in milk, which should be less than 0.5 μg/kg.[20] The official document can be found at FDA's website.[21][22]
- Altertoxins – are those of Alternariol (AOH), Alternariol methyl ether (AME), Altenuene (ALT), Altertoxin-1 (ATX-1), Tenuazonic acid (TeA) and Radicinin (RAD), originated from Alternaria spp. Some of the toxins can be present in sorghum, ragi, wheat and tomatoes.[23][24][25] Some research has shown that the toxins can be easily cross-contaminated between grain commodities, suggesting that manufacturing and storage of grain commodities is a critical practice.[26]
- Citrinin
- Citreoviridin
- Cyclopiazonic acid
- Cytochalasins
- Ergot alkaloids / Ergopeptine alkaloids – Ergotamine
- Fumonisins – Crop corn can be easily contaminated by the fungi Fusarium moniliforme, and its Fumonisin B1 will cause Leukoencephalomalacia (LEM) in horses, Pulmonary edema syndrome (PES) in pigs, liver cancer in rats and Esophageal cancer in humans.[27][28] For human and animal health, both the FDA and the EC have regulated the content levels of toxins in food and animal feed.[29][30]
- Fusaric acid
- Fusarochromanone
- Kojic acid
- Lolitrem alkaloids
- Moniliformin
- 3-Nitropropionic acid
- Nivalenol
- Ochratoxins – In Australia, The Limit of Reporting (LOR) level for Ochratoxin A (OTA) analyses in 20th Australian Total Diet Survey was 1 µg/kg,[31] whereas the EC restricts the content of OTA to 5 µg/kg in cereal commodities, 3 µg/kg in processed products and 10 µg/kg in dried vine fruits.[32]
- Oosporeine
- Patulin – Currently, this toxin has been advisably regulated on fruit products. The EC and the FDA have limited it to under 50 µg/kg for fruit juice and fruit nectar, while limits of 25 µg/kg for solid-contained fruit products and 10 µg/kg for baby foods were specified by the EC.[32][33]
- Phomopsins
- Sporidesmin A
- Sterigmatocystin
- Tremorgenic mycotoxins – Five of them have been reported to be associated with molds found in fermented meats. These are Fumitremorgen B, Paxilline, Penitrem A, Verrucosidin, and Verruculogen.[34]
- Trichothecenes – sourced from Cephalosporium, Fusarium, Myrothecium, Stachybotrys and Trichoderma. The toxins are usually found in molded maize, wheat, corn, peanuts and rice, or animal feed of hay and straw.[35][36] Four trichothecenes, T-2 toxin, HT-2 toxin, diacetoxyscirpenol (DAS) and deoxynivalenol (DON) have been most commonly encountered by humans and animals. The consequences of oral intake of, or dermal exposure to, the toxins will result in Alimentary toxic aleukia, neutropenia, aplastic anemia, thrombocytopenia and/or skin irritation.[37][38][39] In 1993, the FDA issued a document for the content limits of DON in food and animal feed at an advisory level.[40] In 2003, US published a patent that is very promising for farmers to produce a trichothecene-resistant crop.[41]
- Zearalenone
- Zearalenols
Viruses
Viral infections make up perhaps one third of cases of food poisoning in developed countries. In the US, more than 50% of cases are viral and noroviruses are the most common foodborne illness, causing 57% of outbreaks in 2004. Foodborne viral infection are usually of intermediate (1–3 days) incubation period, causing illnesses which are self-limited in otherwise healthy individuals; they are similar to the bacterial forms described above.
- Enterovirus
- Hepatitis A is distinguished from other viral causes by its prolonged (2–6 week) incubation period and its ability to spread beyond the stomach and intestines into the liver. It often results in jaundice, or yellowing of the skin, but rarely leads to chronic liver dysfunction. The virus has been found to cause infection due to the consumption of fresh-cut produce which has fecal contamination.[42][43]
- Hepatitis E
- Norovirus
- Rotavirus
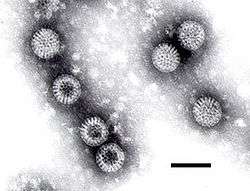 Rotavirus
Rotavirus
Parasites
Most foodborne parasites are zoonoses.
- Platyhelminthes:
- Diphyllobothrium sp.
- Nanophyetus sp.
- Taenia saginata
- Taenia solium
- Fasciola hepatica
- Nematode:
- Protozoa:
- Acanthamoeba and other free-living amoebae
- Cryptosporidium parvum
- Cyclospora cayetanensis
- Entamoeba histolytica
- Giardia lamblia
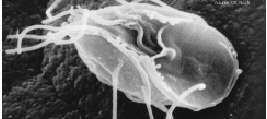 Giardia lamblia
Giardia lamblia - Sarcocystis hominis
- Sarcocystis suihominis
- Toxoplasma gondii
Natural toxins
Several foods can naturally contain toxins, many of which are not produced by bacteria. Plants in particular may be toxic; animals which are naturally poisonous to eat are rare. In evolutionary terms, animals can escape being eaten by fleeing; plants can use only passive defenses such as poisons and distasteful substances, for example capsaicin in chili peppers and pungent sulfur compounds in garlic and onions. Most animal poisons are not synthesised by the animal, but acquired by eating poisonous plants to which the animal is immune, or by bacterial action.
- Alkaloids
- Ciguatera poisoning
- Grayanotoxin (honey intoxication)
- Mushroom toxins
- Phytohaemagglutinin (red kidney bean poisoning; destroyed by boiling)
- Pyrrolizidine alkaloids
- Shellfish toxin, including paralytic shellfish poisoning, diarrhetic shellfish poisoning, neurotoxic shellfish poisoning, amnesic shellfish poisoning and ciguatera fish poisoning
- Scombrotoxin
- Tetrodotoxin (fugu fish poisoning)
Some plants contain substances which are toxic in large doses, but have therapeutic properties in appropriate dosages.
- Foxglove contains cardiac glycosides.
- Poisonous hemlock (conium) has medicinal uses.
Other pathogenic agents
- Prions, resulting in Creutzfeldt–Jakob disease
"Ptomaine poisoning"
In 1883, the Italian professor Salmi, of Bologna, introduced the generic name ptomaine (from Greek ptōma, "fall, fallen body, corpse") for alkaloids found in decaying animal and vegetable matter, especially (as reflected in their names) putrescine and cadaverine.[44] The 1892 Merck's Bulletin stated, "We name such products of bacterial origin ptomaines; and the special alkaloid produced by the comma bacillus is variously named Cadaverine, Putrescine, etc."[45] While The Lancet stated, "The chemical ferments produced in the system, the...ptomaines which may exercise so disastrous an influence."[46] It is now known that the "disastrous...influence" is due to the direct action of bacteria and only slightly to the alkaloids. Thus, the use of the phrase "ptomaine poisoning" is now obsolete.
Tainted potato salad sickening hundreds at a Communist political convention in Massillon, Ohio,[47] and aboard a Washington DC cruise boat in separate incidents during a single week in 1932 drew national attention to the dangers of so-called "ptomaine poisoning" in the pages of the American news weekly, Time.[48] Another newspaper article from 1944 told of more than 150 persons being hospitalized in Chicago with ptomaine poisoning apparently from rice pudding served by a chain of restaurants.[49]
Mechanism
Incubation period
The delay between consumption of a contaminated food and appearance of the first symptoms of illness is called the incubation period. This ranges from hours to days (and rarely months or even years, such as in the case of listeriosis or bovine spongiform encephalopathy), depending on the agent, and on how much was consumed. If symptoms occur within one to six hours after eating the food, it suggests that it is caused by a bacterial toxin or a chemical rather than live bacteria.
The long incubation period of many foodborne illnesses tends to cause sufferers to attribute their symptoms to gastroenteritis.
During the incubation period, microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade the deeper body tissues. The symptoms produced depend on the type of microbe.[50]
Infectious dose
The infectious dose is the amount of agent that must be consumed to give rise to symptoms of foodborne illness, and varies according to the agent and the consumer's age and overall health. Pathogens vary in minimum infectious dose; for example, Shigella sonnei has a low estimated minimum dose of < 500 colony-forming units (CFU) while Staphylococcus aureus has a relatively high estimate.[51]
In the case of Salmonella a relatively large inoculum of 1 million to 1 billion organisms is necessary to produce symptoms in healthy human volunteers,[52] as Salmonellae are very sensitive to acid. An unusually high stomach pH level (low acidity) greatly reduces the number of bacteria required to cause symptoms by a factor of between 10 and 100.
Epidemiology
Asymptomatic subclinical infection may help spread these diseases, particularly Staphylococcus aureus, Campylobacter, Salmonella, Shigella, V. cholerae, and Yersini.[51] For example, as of 1984 it was estimated that in the United States, 200,000 people were asymptomatic carriers of Salmonella.[51]
United States
In the United States, using FoodNet data from 2000–2007, the CDCP estimated there were 47.8 million foodborne illnesses per year (16,000 cases for 100,000 inhabitants)[53] with 9.4 million of these caused by 31 known identified pathogens.[54]
- 127,839 were hospitalized (43 per 100,000 inhabitants).[55][56][57]
- 3,037 people died (1.0 per 100,000 inhabitants).[56][57]
|
|
France
This data pertains to reported medical cases of 23 specific pathogens, as opposed to total population estimates of all food-borne illness for the United States.
In France, for 750,000 cases (1210 per 100,000 inhabitants):
- 70,000 people consulted in the emergency department of an hospital (113 per 100,000 inhabitants.);
- 113,000 people were hospitalized (182 per 100,000 inhabitants);
- 460 people died (0.75 per 100,000 inhabitants).
|
|
Australia
A study by the Australian National University,[60] published in November 2014, found in 2010 that there were an estimated 4.1 million cases of foodborne gastroenteritis acquired in Australia on average each year, along with 5,140 cases of non-gastrointestinal illness. The study was funded by the Australian Department of Health, Food Standards Australia New Zealand and the NSW Food Authority.
The main causes were Norovirus, pathogenic Escherichia coli, Campylobacter spp. and non-typhoidal Salmonella spp., although the causes of approximately 80% of illnesses were unknown. Approximately 25% (90% CrI: 13%–42%) of the 15.9 million episodes of gastroenteritis that occur in Australia were estimated to be transmitted by contaminated food. This equates to an average of approximately one episode of foodborne gastroenteritis every five years per person. Data on the number of hospitalisations and deaths represent the occurrence of serious foodborne illness. Including gastroenteritis, non-gastroenteritis and sequelae, there were an estimated annual 31,920 (90% CrI: 29,500–35,500) hospitalisations due to foodborne illness and 86 (90% CrI: 70–105) deaths due to foodborne illness circa 2010. This study concludes that these rates are similar to recent estimates in the US and Canada.
A main aim of this study was to compare if foodborne illness incidence had increased over time. In this study, similar methods of assessment were applied to data from circa 2000, which showed that the rate of foodborne gastroenteritis had not changed significantly over time. Two key estimates were the total number of gastroenteritis episodes each year, and the proportion considered foodborne. In circa 2010, it was estimated that 25% of all episodes of gastroenteritis were foodborne. By applying this proportion of episodes due to food to the incidence of gastroenteritis circa 2000, there were an estimated 4.3 million (90% CrI: 2.2–7.3 million) episodes of foodborne gastroenteritis circa 2000, although credible intervals overlap with 2010. Taking into account changes in population size, applying these equivalent methods suggests a 17% decrease in the rate of foodborne gastroenteritis between 2000 and 2010, with considerable overlap of the 90% credible intervals.
This study replaces a previous estimate of 5.4 million cases of food-borne illness in Australia every year, causing:[61]
- 18,000 hospitalizations
- 120 deaths (0.5 deaths per 100,000 inhabitants)
- 2.1 million lost days off work
- 1.2 million doctor consultations
- 300,000 prescriptions for antibiotics.
Most foodborne disease outbreaks in Australia have been linked to raw or minimally cooked eggs or poultry.[62] The Australian Food Safety Information Council estimates that one third of cases of food poisoning occur in the home[63]
Comparison between countries
| Country | Annual deaths per 100,000 inhabitants | Annual hospitalization per 100,000 inhabitants |
|---|---|---|
| USA | 1.0 | 43 |
| France | 0.75 | 182 |
| Australia | 0.5 | 82 |
Outbreaks
The vast majority of reported cases of foodborne illness occur as individual or sporadic cases. The origin of most sporadic cases is undetermined. In the United States, where people eat outside the home frequently, 58% of cases originate from commercial food facilities (2004 FoodNet data). An outbreak is defined as occurring when two or more people experience similar illness after consuming food from a common source.
Often, a combination of events contributes to an outbreak, for example, food might be left at room temperature for many hours, allowing bacteria to multiply which is compounded by inadequate cooking which results in a failure to kill the dangerously elevated bacterial levels.
Outbreaks are usually identified when those affected know each other. However, more and more, outbreaks are identified by public health staff from unexpected increases in laboratory results for certain strains of bacteria. Outbreak detection and investigation in the United States is primarily handled by local health jurisdictions and is inconsistent from district to district. It is estimated that 1–2% of outbreaks are detected.
Society and culture
United Kingdom
In postwar Aberdeen (1964) a large-scale (>400 cases) outbreak of typhoid occurred, caused by contaminated corned beef which had been imported from Argentina.[64] The corned beef was placed in cans and because the cooling plant had failed, cold river water from the Plate estuary was used to cool the cans. One of the cans had a defect and the meat inside was contaminated. This meat was then sliced using a meat slicer in a shop in Aberdeen, and a lack of cleaning the machinery led to spreading the contamination to other meats cut in the slicer. These meats were then eaten by the people of Aberdeen who then became ill.
Serious outbreaks of foodborne illness since the 1970s prompted key changes in UK food safety law. These included the death of 19 patients in the Stanley Royd Hospital outbreak[65] and the bovine spongiform encephalopathy (BSE, mad cow disease) outbreak identified in the 1980s. The death of 17 people in the 1996 Wishaw outbreak of E. coli O157[66] was a precursor to the establishment of the Food Standards Agency which, according to Tony Blair in the 1998 white paper A Force for Change Cm 3830, "would be powerful, open and dedicated to the interests of consumers".[67]
In May 2015, for the second year running, England’s Food Standards Agency devoted its annual Food Safety Week to – “The Chicken Challenge”. The focus was on the handling of raw chicken in the home and in catering facilities in a drive to reduce the worryingly high levels of food poisoning from the campylobacter bacterium. Anne Hardy argues that widespread public education of food hygiene can be useful, particularly through media (T.V cookery programmes) and advertisement. She points to the examples set by Scandinavian societies.[68]
United States
In 2001, the Center for Science in the Public Interest petitioned the United States Department of Agriculture to require meat packers to remove spinal cords before processing cattle carcasses for human consumption, a measure designed to lessen the risk of infection by variant Creutzfeldt–Jakob disease. The petition was supported by the American Public Health Association, the Consumer Federation of America, the Government Accountability Project, the National Consumers League, and Safe Tables Our Priority.[69] This was opposed by the National Cattlemen's Beef Association, the National Renderers Association, the National Meat Association, the Pork Producers Council, sheep raisers, milk producers, the Turkey Federation, and eight other organizations from the animal-derived food industry.[70]
None of the US Department of Health and Human Services targets[71] regarding incidence of foodborne infections were reached in 2007.[72]
Organizations
The World Health Organization Department of Food Safety and Zoonoses (FOS) provides scientific advice for organizations and the public on issues concerning the safety of food. Its mission is to lower the burden of foodborne disease, thereby strengthening the health security and sustainable development of Member States. Foodborne and waterborne diarrhoeal diseases kill an estimated 2.2 million people annually, most of whom are children. WHO works closely with the Food and Agriculture Organization of the United Nations (FAO) to address food safety issues along the entire food production chain—from production to consumption—using new methods of risk analysis. These methods provide efficient, science-based tools to improve food safety, thereby benefiting both public health and economic development.
International Food Safety Authorities Network (INFOSAN)
The International Food Safety Authorities Network (INFOSAN) is a joint program of the WHO and FAO. INFOSAN has been connecting national authorities from around the globe since 2004, with the goal of preventing the international spread of contaminated food and foodborne disease and strengthening food safety systems globally. This is done by:
- Promoting the rapid exchange of information during food safety events;
- Sharing information on important food safety issues of global interest;
- Promoting partnership and collaboration between countries; and
- Helping countries strengthen their capacity to manage food safety risks.
Membership to INFOSAN is voluntary, but is restricted to representatives from national and regional government authorities and requires an official letter of designation. INFOSAN seeks to reflect the multidisciplinary nature of food safety and promote intersectoral collaboration by requesting the designation of Focal Points in each of the respective national authorities with a stake in food safety, and a single Emergency Contact Point in the national authority with the responsibility for coordinating national food safety emergencies; countries choosing to be members of INFOSAN are committed to sharing information between their respective food safety authorities and other INFOSAN members. The operational definition of a food safety authority includes those authorities involved in: food policy; risk assessment; food control and management; food inspection services; foodborne disease surveillance and response; laboratory services for monitoring and surveillance of foods and foodborne diseases; and food safety information, education and communication across the farm-to-table continuum.
Regulatory steps
Food may be contaminated during all stages of food production and retailing. In order to prevent viral contamination, regulatory authorities in Europe have enacted several measures:
- European Commission Regulation (EC) No 2073/2005 of November 15, 2005
- European Committee for Standardization (CEN): Standard method for the detection of norovirus and hepatitis A virus in food products (shellfish, fruits and vegetables, surfaces and bottled water)
- CODEX Committee on Food Hygiene (CCFH): Guideline for the application of general principles of food hygiene for the control of viruses in food[73]
See also
- 1984 Rajneeshee bioterror attack
- 2006 North American E. coli outbreak
- Food allergy
- Food hygiene
- Food microbiology
- Food quality
- Food safety
- Food spoilage
- Food testing strips
- Gastroenteritis
- List of foodborne illness outbreaks by country
- Mycotoxicology
- Refrigerate after opening
- STOP Foodborne Illness
- United States Disease Control and Prevention
- Zoonotic pathogens
- American Public Health Association v. Butz
References
- ↑ "food poisoning" at Dorland's Medical Dictionary
- 1 2 "Foodborne Illness - Frequently Asked Questions". US Centers for Disease Control and Prevention. Archived from the original on March 3, 2011. Retrieved 3 July 2016.
- ↑ For foodborne illness caused by chemicals, see Food contaminants.
- ↑ "Reducing the risk from E. coli 0157 – controlling cross-contamination". Food Standards Agency, United Kingdom. February 2011. Retrieved 14 August 2016.
- ↑ "Staphylococcal Food Poisoning". U.S. Centers for Disease Control and Prevention. Retrieved 3 July 2016.
- ↑ Humphrey T, O'Brien S, Madsen M (2007). "Campylobacters as zoonotic pathogens: a food production perspective". International Journal of Food Microbiology. 117 (3): 237–57. doi:10.1016/j.ijfoodmicro.2007.01.006. PMID 17368847.
- ↑ "Foodborne Illness: What Consumers Need to Know". USDA.gov. Retrieved 14 August 2016.
- ↑ Tribe, Ingrid G; Cowell, David; Cameron, Peter; Cameron, Scott (2002). "An outbreak of Salmonella Typhimurium phage type 135 infection linked to the consumption of raw shell eggs in an aged care facility". Communicable Diseases Intelligence. 26 (1): 38–9. PMID 11950200. Archived from the original on February 17, 2014.
- ↑ "Salmonella Infection (salmonellosis) and Animals". Centers for Disease Control and Prevention. Retrieved August 12, 2007.
- ↑ Doyle, M. P.; Erickson, M. C. (2006). "Reducing the carriage of foodborne pathogens in livestock and poultry". Poultry science. 85 (6): 960–73. doi:10.1093/ps/85.6.960. PMID 16776463.
- ↑ Food poisoning: Causes. Mayo Clinic.
- 1 2 Argudín M, Mendoza MC, Rodicio MR (2010). "Food poisoning and Staphylococcus aureus enterotoxins". Toxins (Basel). 2 (7): 1751–73. doi:10.3390/toxins2071751. PMC 3153270
 . PMID 22069659.
. PMID 22069659. - ↑ Staphylococcus aureus: A Problem When Food Is Left Out Too Long. Ohio State University Extension HYG-5564-11].
- ↑ "FDA Says Viruses Safe for Treating Meat". Archived from the original on August 25, 2006. Retrieved September 2, 2014.
- ↑ DeRusha, Jason. "Good Question: Does Washing Fruit Do Anything?". Retrieved 2016-09-18.
- ↑ How Temperatures Affect Food. U.D. Department of Agriculture
- ↑ Mount, Michael. "Fungi and Mycotoxins" (PDF). vetmed.ucdavis.edu. Retrieved August 11, 2007.
- ↑ "Aflatoxins". Center for Food Safety & Applied Nutrition. Retrieved August 12, 2007.
- ↑ "GASGA Technical Leaflet – 3 Mycotoxins in Grain". Food and Agriculture Organization of the United Nations. Retrieved August 12, 2007.
- ↑ "Chapter 2 Foodborne Hazards in Basic Food Safety for Health Workers" (PDF). World Health Organization. Retrieved August 12, 2007.
- ↑ "Sec. 683.100 Action Levels for Aflatoxins in Animal Feeds (CPG 7126.33)". Food and Drug Administration. Retrieved August 13, 2007.
- ↑ Henry, Michael H. "Mycotoxins in Feeds: CVM's Perspective". FDA.gov. Retrieved January 1, 2012.
- ↑ Webley DJ, Jackson KL, Mullins JD, Hocking AD, Pitt JI (1997). "Alternaria toxins in weather-damaged wheat and sorghum in the 1995–1996 Australian harvest". Australian Journal of Agricultural Research. 48 (8): 1249–56. doi:10.1071/A97005.
- ↑ Li F, Yoshizawa T (2000). "Alternaria mycotoxins in weathered wheat from China". J. Agric. Food Chem. 48 (7): 2920–4. doi:10.1021/jf0000171. PMID 10898645.
- ↑ Motta SD, Valente Soares LM (2001). "Survey of Brazilian tomato products for alternariol, alternariol monomethyl ether, tenuazonic acid and cyclopiazonic acid". Food Addit Contam. 18 (7): 630–4. doi:10.1080/02652030117707. PMID 11469319.
- ↑ Li FQ, Toyazaki N, Yoshizawa T (2001). "Production of alternaria mycotoxins by Alternaria alternata isolated from weather-damaged wheat". J. Food Prot. 64 (4): 567–71. PMID 11307900.
- ↑ Marasas WF (1995). "Fumonisins: their implications for human and animal health". Nat. Toxins. 3 (4): 193–8; discussion 221. doi:10.1002/nt.2620030405. PMID 7582616.
- ↑ Soriano, J.M. (2004). "Occurrence of fumonisins in foods". Food Research International. 37 (10): 985–1000. doi:10.1016/j.foodres.2004.06.009.
- ↑ "CVM and Fumonisins". Food and Drug Administration. Archived from the original on August 12, 2007. Retrieved August 13, 2007.
- ↑ "More contaminated maize meal products withdrawn from sale". Food Standards Agency. Retrieved August 12, 2007.
- ↑ "20th Australian Total Diet Survey – Part B". Food Standards Australia New Zealand. Retrieved August 13, 2007.
- 1 2 "Worldwide regulations for mycotoxins in food and feed in 2003". FAO FOOD AND NUTRITION PAPER 81. Retrieved August 13, 2007.
- ↑ "Patulin in Apple Juice, Apple Juice Concentrates and Apple Juice Products". Food and Drug Administration. Retrieved August 16, 2007.
- ↑ Sabater-Vilar M, Nijmeijer S, Fink-Gremmels J (2003). "Genotoxicity assessment of five tremorgenic mycotoxins (fumitremorgen B, paxilline, penitrem A, verruculogen, and verrucosidin) produced by molds isolated from fermented meats". J. Food Prot. 66 (11): 2123–9. PMID 14627292.
- ↑ Adejumo TO, Hettwer U, Karlovsky P (May 2007). "Occurrence of Fusarium species and trichothecenes in Nigerian maize". Int. J. Food Microbiol. 116 (3): 350–7. doi:10.1016/j.ijfoodmicro.2007.02.009. PMID 17412440.
- ↑ Mazur LJ, Kim J (2006). "Spectrum of noninfectious health effects from molds". Pediatrics. 118 (6): e1909–26. doi:10.1542/peds.2006-2829. PMID 17142508.
- ↑ Froquet R, Sibiril Y, Parent-Massin D (2001). "Trichothecene toxicity on human megakaryocyte progenitors (CFU-MK)". Hum Exp Toxicol. 20 (2): 84–9. doi:10.1191/096032701677428611. PMID 11327514.
- ↑ Joffe AZ, Yagen B (1977). "Comparative study of the yield of T-2 toxic produced by Fusarium poae, F. sporotrichioides and F. sporotrichioides var. tricinctum strains from different sources". Mycopathologia. 60 (2): 93–7. doi:10.1007/bf00490378. PMID 846559.
- ↑ Hay, R. J. (2007). "Fusarium infections of the skin". Current Opinion in Infectious Diseases. 20 (2): 115. doi:10.1097/QCO.0b013e328014392d.
- ↑ "Guidance for Industry and FDA – Letter to State Agricultural Directors, State Feed Control Officials, and Food, Feed, and Grain Trade Organizations". Food and Drug Administration. Archived from the original on June 9, 2007. Retrieved August 13, 2007.
- ↑ Hohn, Thomas M. "Trichothecene-resistant transgenic plants". U.S. Patent 6,646,184. Priority date March 31, 1999.
- ↑ Dubois E, Hennechart C, Deboosère N, et al. (April 2006). "Intra-laboratory validation of a concentration method adapted for the enumeration of infectious F-specific RNA coliphage, enterovirus, and hepatitis A virus from inoculated leaves of salad vegetables". Int. J. Food Microbiol. 108 (2): 164–71. doi:10.1016/j.ijfoodmicro.2005.11.007. PMID 16387377.
- ↑ Schmidt, Heather Martin. "Improving the microbilological quality and safety of fresh-cut tomatoes by low dose dlectron beam irradiation – Master thesis" (PDF). Retrieved August 11, 2007.
- ↑ Oxford English Dictionary (First ed.). London: Oxford University Press. 1933. p. 1557.
- ↑ Merck's Bulletin, Volume 5, William Henry Porter, 1892.
- ↑ Lancet, 3 Oct 1891, page 752
- ↑ "Report Next Week," Evening Independent (Massillon, OH), July 22, 1932, pg. 6
- ↑ "Medicine: Potato Salad," Time, August 1, 1932.
- ↑ "Poisoning Hits 150 in Chicago". Kenosha Evening News. May 27, 1944.
- ↑ "Food-Related Diseases". US Centers for Disease Control and Prevention.
- 1 2 3 Greig, Judy D. "Infective Doses and Pathogen Carriage". Public Health Agency of Canada.
- ↑ Owens, Michael D (January 2014) Salmonella Infection in Emergency Medicine. emedicine.com
- ↑ Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM (2011). "Foodborne illness acquired in the United States—unspecified agents". Emerging Infectious Diseases. 17 (1): 16–22. doi:10.3201/eid1701.P21101. PMC 3204615
 . PMID 21192849.
. PMID 21192849. - 1 2 3 Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, et al. (2011). "Foodborne illness acquired in the United States—major pathogens". Emerging Infectious Diseases. 17 (1): 7–15. doi:10.3201/eid1701.P11101. PMC 3375761
 . PMID 21192848.
. PMID 21192848.
- ↑ "Obama Proposes Single Overseer for Food Safety". New York Times. February 20, 2015. Retrieved 2015-02-22.
According to the C.D.C., an estimated 87 million Americans are sickened each year by contaminated food, 371,000 are hospitalized with food-related illness and 5,700 die from food-related disease
- 1 2 Sabrina Tavernise (July 26, 2013). "F.D.A. Says Importers Must Audit Food Safety". New York Times. Retrieved July 27, 2013.
One in every six Americans becomes ill from eating contaminated food each year, Dr. Margaret A. Hamburg, F.D.A. commissioner, estimated. About 130,000 are hospitalized and 3,000 die.
- 1 2 Stephanie Strom (January 4, 2013). "F.D.A. Offers Sweeping Rules to Fight Food Contamination". New York Times. Retrieved January 5, 2013.
One in six Americans becomes ill from eating contaminated food each year, the government estimates; of those, roughly 130,000 are hospitalized and 3,000 die.
- ↑ "Report of the French sanitary agencies" (PDF) (in French). INVS/Afssa.
- ↑ "Summary of Report of the French sanitary agencies" (PDF) (in French). INVS/Afssa.
- ↑ Kirk, Martyn; et al. "Foodborne illness in Australia: Annual incidence circa 2010 pp7-9". Australia Department of Health. Australian National University. Retrieved 13 September 2015.
- ↑ "Food borne illness in Australia" (PDF). OzFoodNet.
- ↑ Astridge, K; McPherson, M; Kirk, M; et al. (2011). "Foodborne disease outbreaks in Australia 2001-2009". Food Australia. 63 (12): 44–50.
- ↑ "Food Hygiene". BUPA. Retrieved 13 September 2015.
- ↑ Smith, David F.; Diack, H. Lesley and Pennington, T. Hugh (2005) Food Poisoning, Policy and Politics : Corned Beef and Typhoid in Britain in the 1960s. Boydell Press. ISBN 1-84383-138-4
- ↑ Brian Deer (February 24, 1985). "Food poison deaths probe may reveal NHS flaws". The Sunday Times.
- ↑ Cowden JM, Ahmed S, Donaghy M, Riley A (2001). "Epidemiological investigation of the Central Scotland outbreak of Escherichia coli O157 infection, November to December 1996" (PDF). Epidemiol. Infect. 126: 335–341. doi:10.1017/S0950268801005520. PMC 2869700
 . PMID 11467789.
. PMID 11467789. - ↑ "The Food Standards Agency: A Force for Change". gov.uk. Food Standards Agency, United Kingdom. January 14, 1998. Retrieved 14 August 2016.
- ↑ Hardy, Anne (13 January 2016). "Food Poisoning: An On-going Saga". History and Policy. History and Policy. Retrieved 4 July 2016.
- ↑ "Meat Produced by Advanced Meat/Bone Separation Machinery and Meat Recovery (AMR) Systems". Federal Register. U.S. National Archive and Records Administration. Retrieved 3 July 2016.
- ↑ "Livestock Industry Opposed to Stricter Laws on Mad Cow Prevention". January 2003. Retrieved 3 July 2016.
- ↑ Healthy People 2010 Home Page
- ↑ "Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food—10 states, 2007". MMWR Morb. Mortal. Wkly. Rep. 57 (14): 366–70. April 2008. PMID 18401330.
- ↑ "Codex Committee on Food Hygiene (CCFH)", European Commission, Retrieved April 7, 2015
-
 This article incorporates public domain material from the Centers for Disease Control and Prevention website http://www.cdc.gov/.
This article incorporates public domain material from the Centers for Disease Control and Prevention website http://www.cdc.gov/.
Further reading
Periodicals
- International Journal of Food Microbiology, ISSN 0168-1605, Elsevier
- Foodborne Pathogens and Disease, ISSN 1535-3141, Mary Ann Liebert, Inc.
- Mycopathologia, ISSN 1573-0832 (electronic), ISSN 0301-486X (paper), Springer
Books
- Hocking, Ailsa D.; Pitt, John I.; Samson, Robert A.; Thrane, Ulf (2005). Advances in Food Mycology. Springer. ISBN 978-0-387-28385-2. ISBN 978-0-387-28391-3 (electronic).
- Hobbs, Betty C. (1993). Food Poisoning and Food Hygiene. Edward Arnold. ISBN 978-0-340-53740-4.
- Riemann, Hans P.; Cliver, Dean O. (2006). FoodBorne Infections and Intoxications. Academic Press. ISBN 978-0-12-588365-8.
- Smith, James L. (2005). Fratamico, Pina M.; Bhunia, Arun K.; Smith, James L., eds. Foodborne Pathogens: Microbiology And Molecular Biology. Horizon Scientific Press. ISBN 978-1-904455-00-4.
External links
- Foodborne diseases, emerging, WHO, Fact sheet N°124, revised January 2002
- Foodborne illness information pages, NSW Food Authority
- Food safety and foodborne illness, WHO, Fact sheet N°237, revised January 2002
- UK Health protection Agency
- US PulseNet
- Food poisoning from NHS Direct Online
- Food Safety Network hosted at the University of Guelph, Canada.
- Food Standard Agency website