Pediculosis pubis
| Pediculosis pubis | |
|---|---|
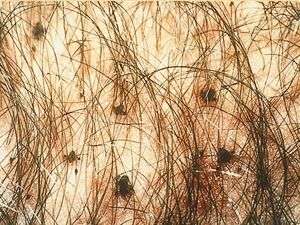 | |
| Pubic lice in genital area | |
| Classification and external resources | |
| Specialty | infectious disease |
| ICD-10 | B85.3 |
| ICD-9-CM | 132.2 |
| DiseasesDB | 10028 |
| MedlinePlus | 000841 |
| eMedicine | med/1769 |
| MeSH | D010373 |


Pediculosis pubis (also known as "crabs" and "pubic lice"[1]) is a disease caused by the pubic louse, Pthirus pubis, a parasitic insect notorious for infesting human pubic hair. The species may also live on other areas with hair, including the eyelashes, causing pediculosis ciliaris. Infestation usually leads to intense itching in the pubic area. Treatment with topic agents such as permethrin or pyrethrin with piperonyl butoxide is exceedingly effective. Worldwide it affects about 2% of the population.
Classification
Infestation with pubic lice is also called phthiriasis or phthiriasis pubis, while infestation of eyelashes with pubic lice is called phthiriasis palpebrarum or pediculosis ciliarum.[2] The disease is spelled with phth, even though the scientific name of the louse is spelled with pth.
Signs and symptoms
The main symptom is itching, usually in the pubic-hair area, resulting from hypersensitivity to louse saliva, which can become stronger over two or more weeks following initial infestation.[3] In some infestations, a characteristic grey-blue or slate coloration macule appears (maculae caeruleae) at the feeding site, which may last for days.[3] Nits or live lice may also be visible to the unaided eye.[3] [4]
Parasitology
Characteristics
Pubic lice are between 1 and 3 mm long with 6 legs.[3]
Transmission
Pubic lice are usually acquired by intimate contact between individuals.[3] Parent-to-child infestations are more likely to occur through routes of shared towels, clothing, beds or closets. Adults are more frequently infested than children. As with most sexually transmitted pathogens, they can only survive a short time away from the warmth and humidity of the human body.
Infection in a young child or teenager is not necessarily indicative of sexual abuse, although this possibility should be kept in mind.[5][6]
Diagnosis
A pubic louse infestation is usually diagnosed by carefully examining pubic hair for nits, nymphs, and adult lice.[3] Lice and nits can be removed either with forceps or by cutting the infested hair with scissors (with the exception of an infestation of the eye area). A magnifying glass or a stereo-microscope can be used for the exact identification. If lice are detected in one family member, the entire family needs to be checked and only those who are infested with living lice should be treated.
Testing for other sexually transmitted infections is recommended in those who are affected.[3]
Treatment
Pediculosis pubis
Recommended treatments include the topical agents permethrin or pyrethrins with piperonyl butoxide.[3] Lindane is a second line treatment due to concerns of toxicity.[3] The Centers for Disease Control and Prevention (CDC) states that lindane should not be used by persons who have extensive dermatitis, women who are pregnant or lactating or children aged under two years.[7] The FDA similarly warns against use in patients with a history of uncontrolled seizure disorders and cautious use in infants, children, the elderly, and individuals with other skin conditions (e.g., atopic dermatitis, psoriasis) and in those who weigh less than 110 lbs (50 kg).[8][9]
Bedding and clothing should be laundered and sexual contact should be avoided until cured.[3] A second treatment is occasionally required if not improved after 3 to 7 days.[3]
Pubic lice are primarily spread through sexual intercourse. Therefore, all partners with whom the patient has had sexual contact within the previous 30 days should be evaluated and treated, and sexual contact should be avoided until all partners have successfully completed treatment and are thought to be cured. Because of the strong association between the presence of pubic lice and classic sexually transmitted infections (STIs), patients diagnosed with pubic lice should undergo evaluation for other STIs.
Pediculosis ciliaris
Infections of the eyelashes may be treated with either petroleum jelly applied twice daily for 10 days or malathion, phenothrin and carbaryl.[3]
Epidemiology
Current worldwide prevalence has been very approximately estimated at two percent of the human population. Accurate numbers are difficult to acquire, because pubic lice infestations are not considered a reportable condition by many governments, and many cases are self-treated or treated discreetly by personal physicians.[10]
Although any part of the body may be colonized, crab lice favor the hairs of the genital and peri-anal region. Especially in male patients, pubic lice and eggs can also be found in hair on the abdomen and under the armpits, as well as on the beard and mustache, while in children they are usually found in eyelashes.
It has recently been suggested that an increasing percentage of humans removing their pubic hair has led to reduced crab louse populations in some parts of the world.[11][12]
In animals
Humans are the only known hosts of this parasite, although a closely related species, Pthirus gorillae, infects gorilla populations.[13]
References
- ↑ Ronald P. Rapini; Jean L. Bolognia; Joseph L. Jorizzo (2007). Dermatology. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ↑ N. P. Manjunatha; G. R. Jayamanne; S. P. Desai; T. R. Moss; J. Lalik; A. Woodland (2006). "Pediculosis pubis: presentation to ophthalmologist as pthriasis palpebrarum associated with corneal epithelial keratitis". International Journal of STD & AIDS. 17 (6): 424–426. doi:10.1258/095646206777323445.
- 1 2 3 4 5 6 7 8 9 10 11 12 P. A. Leone (2007). "Scabies and pediculosis pubis: an update of treatment regimens and general review". Clinical Infectious Diseases. 44 (Suppl. 3): S153–S159. doi:10.1086/511428. PMID 17342668.
- ↑ John O'Donel Alexander (1984). Arthropods and Human Skin. Berlin: Springer. ISBN 978-1-4471-1358-4.
- ↑ Sidney Klaus; Yigal Shvil; Kosta Y. Mumcuoglu (1994). "Generalized infestation of a 3½-year-old girl with the pubic louse". Pediatric Dermatology. 11 (1): 26–28. doi:10.1111/j.1525-1470.1994.tb00068.x. PMID 8170844.
- ↑ José A. Varela; Luis Otero; Emma Espinosa; Carmen Sánchez; María Luisa Junquera; Fernando Vázquez (April 2003). "Phthirus pubis in a sexually transmitted diseases unit: a study of 14 years". Sexually Transmitted Diseases. 30 (4): 292–6. doi:10.1097/00007435-200304000-00004. PMID 12671547.
- ↑ U.S. Centers for Disease Control and Prevention (CDC). Ectoparasitic infections. Sexually transmitted diseases treatment guidelines. 2006" MMWR Recomm Rep 2006, August 10;55 (No. RR-11) 79-80.
- ↑ Lindane shampoo, USP, 1% prescribing information. Updated March 28, 2003.
- ↑ (FDA). Lindane Post Marketing Safety Review (PDF). Posted 2003.
- ↑ Alice L. Anderson; Elizabeth Chaney (2009). "Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US College students". International Journal of Environmental Research and Public Health. 6 (2): 592–600. doi:10.3390/ijerph6020592. PMC 2672365
 . PMID 19440402.
. PMID 19440402. - ↑ N. R. Armstrong; J. D. Wilson (2006). "Did the "Brazilian" kill the pubic louse?". Sexually Transmitted Infections. 82: 265–266. doi:10.1136/sti.2005.018671. PMC 2564756
 . PMID 16731684.
. PMID 16731684. - ↑ Bloomberg: Brazilian bikini waxes make crab lice endangered species, published 13 January 2013, retrieved 14 January 2013
- ↑ Robin A. Weiss (2009). "Apes, lice and prehistory". Journal of Biology. 8 (2): 20. doi:10.1186/jbiol114. PMC 2687769
 . PMID 19232074.
. PMID 19232074.
External links
| Wikimedia Commons has media related to Pubic lice. |
- Crab louse on the UF / IFAS Featured Creatures Web site
- Edinburgh Royal Infirmary on Pubic Lice
- Medline Plus article
- Guideline on the Management of Phthirus pubis infestation (UK, 2007)
- Genetic Analysis of Lice Supports Direct Contact Between Modern and Archaic Humans