Pelvic pain
| Pelvic and perineal pain | |
|---|---|
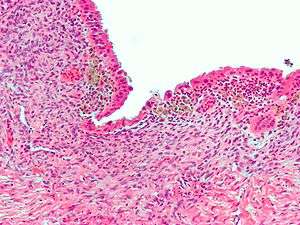 | |
| Micrograph showing endometriosis (H&E stain), a common cause of chronic pelvic pain in women. | |
| Classification and external resources | |
| ICD-10 | R10.2 |
| ICD-9-CM | 625.9, 789.00 |
| MeSH | D017699 |
Pelvic pain is pain in the area of the pelvis. Acute pain is more common than chronic pain.[1] If the pain lasts for more than six months, it is deemed to be chronic pelvic pain.[2] It can affect both women and men.
Common causes in include: endometriosis in women, bowel adhesions, irritable bowel syndrome, and interstitial cystitis.[3] The cause may also be a number of poorly understood conditions that may represent abnormal psychoneuromuscular function.
Terminology
Urologic chronic pelvic pain syndrome (UCPPS) is an umbrella term adopted for use in research into pain syndromes associated with the male and female pelvis. It is not intended for use as a clinical diagnosis. The hallmark symptom for inclusion is chronic pain in the pelvis, pelvic floor or external genitalia, although this is often accompanied by lower urinary tract symptoms (LUTS).[4]
Chronic pelvic pain in men is referred to as chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and is also known as chronic nonbacterial prostatitis. Men in this category have no known infection, but do have extensive pelvic pain lasting more than 3 months.[5]
Cause
Female
Many different conditions can cause pelvic pain including:
- exaggerated bladder, bowel, or uterine pain sensitivity (also known as visceral pain)
- pelvic girdle pain (SPD or DSP)
- Pudendal nerve entrapment
- Gynecologic
- Dysmenorrhea—pain during the menstrual period
- Endometriosis—pain caused by uterine tissue that is outside the uterus. Endometriosis can be visually confirmed by laparoscopy in approximately 75% of adolescent girls with chronic pelvic pain that is resistant to treatment, and in approximately 50% of adolescent in girls with chronic pelvic pain that is not necessarily resistant to treatment.[6]
- Müllerian abnormalities
- Pelvic inflammatory disease—pain caused by damage from infections
- Ovarian cysts—the ovary produces a large, painful cyst, which may rupture
- Ovarian torsion—the ovary is twisted in a way that interferes with its blood supply
- Ectopic pregnancy—a pregnancy implanted outside the uterus
- Abdominal
- Loin pain hematuria syndrome
- Proctitis—infection or inflammation of the anus or rectum
- Colitis—infection or inflammation of the colon
- Appendicitis—infection or inflammation of the bowel
Internal hernias are difficult to identify in women, and misdiagnosis with endometriosis or idiopathic chronic pelvic pain is very common. One cause of misdiagnosis that when the woman lies down flat on an examination table, all of the medical signs of the hernia disappear. The hernia can typically only be detected when symptoms are present, so diagnosis requires positioning the woman's body in a way that provokes symptoms.[7]
Diagnosis
Females
The diagnostic workup begins with a careful history and examination, followed by a pregnancy test. Some women may also need bloodwork or additional imaging studies, and a handful may also benefit from having surgical evaluation.
The absence of visible pathology in chronic pain syndromes should not form the basis for either seeking psychological explanations or questioning the reality of the patient’s pain. Instead it is essential to approach the complexity of chronic pain from a psychophysiological perspective which recognises the importance of the mind-body interaction. Some of the mechanisms by which the limbic system impacts on pain, and in particular myofascial pain, have been clarified by research findings in neurology and psychophysiology.[1]
Males
In chronic pelvic pain there are no standard diagnostic tests in males; diagnosis is by exclusion of other disease entities.
Chronic pelvic pain (category IIIB) is often misdiagnosed as chronic bacterial prostatitis and needlessly treated with antibiotics exposing the patient to inappropriate antibiotic use and unnecessarily to adverse effects with little if any benefit in most cases. Within a Bulgarian study, where by definition all patients had negative microbiological results, a 65% adverse drug reaction rate was found for patients treated with ciprofloxacin in comparison to a 9% rate for the placebo patients. This was combined with a higher cure rate (69% v 53%) found within the placebo group.[8]
Treatment
Females
Many women will benefit from a consultation with a physical therapist, a trial of anti-inflammatory medications, hormonal therapy, or even neurological agents.
A hysterectomy is sometimes performed.[9]
Spinal cord stimulation has been explored as a potential treatment option for some time, however there remains to be consensus on where the optimal location of the spinal cord this treatment should be aimed. As the innervation of the pelvic region is from the sacral nerve roots, previous treatments have been aimed at this region; results have been mixed. Spinal cord stimulation aimed at the mid- to high-thoracic region of the spinal cord have produced some positive results.[10]
Male
Multimodal therapy is the most successful treatment option in chronic pelvic pain,[11] and includes α-blockers,[12] phytotherapy,[13][14] and protocols aimed at quieting the pelvic nerves through myofascial trigger point release with psychological re-training for anxiety control.[15][16] Antibiotics are not recommended.[17][18]
Epidemiology
Female
Most women, at some time in their lives, experience pelvic pain. As girls enter puberty, pelvic or abdominal pain becomes a frequent complaint. Chronic pelvic pain is a common condition with rate of dysmenorrhoea between 16.8—81%, dyspareunia between 8—21.8%, and noncyclical pain between 2.1—24%.[19]
According to the CDC, Chronic pelvic pain (CPP) accounted for approximately 9% of all visits to gynecologists in 2007.[20] In addition, CPP is the reason for 20—30% of all laparoscopies in adults. Pelvic girth pain is frequent during pregnancy.[21]
Social implications
In the pursuit of better outcomes for people, problems have been found in current procedures for the treatment of chronic pelvic pain (CPP). These relate primarily with regard to the conceptual dichotomy between an ‘organic’ genesis of pain, where the presence of tissue damage is presumed, and a ‘psychogenic’ origin, where pain occurs despite a lack of damage to tissue.[22] CPP literature in medicine and psychiatry reflects a paradigm where unproblematically observable ‘organic’ processes are causally and sequentially explained, despite evidence in favour of a possible model which accounts for the “complex role played by meaning and consciousness” in the experience of pain.[22] While in the literature of causal mechanisms reference is made to ‘subjective’ aspects of pain, current models do not provide a means through which these aspects may be accessed or understood.[22] Without interpretive or ‘subjective’ approaches to the pain experienced by patients, medical understandings of CPP are fixed within ‘organic’ sequences of the “purely object” body conceptually separated from the patient.[22] Despite the prevalence of this wider understanding of the biological genesis of pain, alternate diagnosis and treatments of CPP in multidisciplinary settings have shown high success rates for people for whom ‘organic’ pathology has been unhelpful.[22]
Research
In 2007, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the United States National Institutes of Health, began using UCPPS as a term to refer to chronic pelvic pain syndromes, mainly interstitial cystitis/bladder pain syndrome (IC/BPS) in women and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) in men.[23][24]
MAPP Research Network
In 2008, NIDDK established the MAPP (Multidisciplinary Approach to the Study of Chronic Pelvic Pain) Research Network to help better understand the underlying causes of IC/BPS and CP/CPPS, recognising that there was a lack of understanding and management of these pain syndromes and also that they were frequently associated with chronic pain disorders elsewhere in the body.[25] Through its research, the aims are "to discover new and clinically relevant insights that may lead to improved treatment options and better patient care".[25]
Research findings by the MAPP Research Network include:
- People with painful bladder symptoms (painful filling or painful urgency) have more severe UCPPS symptoms, more systemic presentation of syndromes and poorer quality of life.[26]
References
- 1 2 Marek Jantos (2007). "Understanding Chronic Pelvic Pain". Pelviperineology. 26 (2): 66–69.
- ↑ "Chronic pelvic pain" (PDF). ACOG. Retrieved 11 June 2014.
- ↑ Ortiz, DD (Jun 1, 2008). "Chronic pelvic pain in women.". American family physician. 77 (11): 1535–42. PMID 18581833.
- ↑ J. Curtis Nickel; Dean A Tripp; Allan Gordon; Michel Pontari; Daniel Shoskes; Kenneth M Peters; Ragi Doggweiler; Andrew P Baranowski (January 2011). "Update on Urologic Pelvic Pain Syndromes". Reviews in Urology. 13 (1): 39–49. PMC 3151586
 . PMID 21826127.
. PMID 21826127. - ↑ Luzzi GA (2002). "Chronic prostatitis and chronic pelvic pain in men: aetiology, diagnosis and management". Journal of the European Academy of Dermatology and Venereology : JEADV. 16 (3): 253–6. doi:10.1046/j.1468-3083.2002.00481.x. PMID 12195565.
- ↑ Janssen, E. B.; Rijkers, A. C. M.; Hoppenbrouwers, K.; Meuleman, C.; d'Hooghe, T. M. (2013). "Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: A systematic review". Human Reproduction Update. 19 (5): 570–582. doi:10.1093/humupd/dmt016. PMID 23727940.
- ↑ Brody, Jane E. "In women, hernias may be hidden agony" The St. Louis Post-Dispatch. 18 May 2011.
- ↑ J. Dimitrakov; J. Tchitalov; T. Zlatanov; D. Dikov. "A Prospective, Randomized, Double-Blind, Placebo-Controlled Study Of Antibiotics For The Treatment Of Category Iiib Chronic Pelvic Pain Syndrome In Men". Third International Chronic Prostatitis Network. Retrieved 4 September 2009.
The results of our study show that antibiotics have an unacceptably high rate of adverse side effects as well as a statistically insignificant improvement over placebo...
- ↑ Kuppermann M, Learman LA, Schembri M, et al. (March 2010). "Predictors of hysterectomy use and satisfaction". Obstet Gynecol. 115 (3): 543–51. doi:10.1097/AOG.0b013e3181cf46a0. PMID 20177285.
- ↑ Hunter, C; Davé, N; Diwan, S; Deer, T (Jan 2013). "Neuromodulation of pelvic visceral pain: review of the literature and case series of potential novel targets for treatment.". Pain Practice. 13 (1): 3–17. doi:10.1111/j.1533-2500.2012.00558.x. PMID 22521096.
- ↑ Potts JM (2005). "Therapeutic options for chronic prostatitis/chronic pelvic pain syndrome". Current Urology Reports. 6 (4): 313–7. doi:10.1007/s11934-005-0030-5. PMID 15978236.
- ↑ Yang G, Wei Q, Li H, Yang Y, Zhang S, Dong Q (2006). "The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials". J. Androl. 27 (6): 847–52. doi:10.2164/jandrol.106.000661. PMID 16870951.
...treatment duration should be long enough (more than 3 months)
- ↑ Shoskes DA, Zeitlin SI, Shahed A, Rajfer J (1999). "Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial". Urology. 54 (6): 960–3. doi:10.1016/S0090-4295(99)00358-1. PMID 10604689.
- ↑ Elist J (2006). "Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study". Urology. 67 (1): 60–3. doi:10.1016/j.urology.2005.07.035. PMID 16413333.
- ↑ Anderson RU, Wise D, Sawyer T, Chan C (2005). "Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men". J. Urol. 174 (1): 155–60. doi:10.1097/01.ju.0000161609.31185.d5. PMID 15947608.
- ↑ Anderson RU, Wise D, Sawyer T, Chan CA (2006). "Sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: improvement after trigger point release and paradoxical relaxation training". J. Urol. 176 (4 Pt 1): 1534–8; discussion 1538–9. doi:10.1016/j.juro.2006.06.010. PMID 16952676.
- ↑ Alexander RB, Propert KJ, Schaeffer AJ, et al. (2004). "Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial". Ann. Intern. Med. 141 (8): 581–9. doi:10.7326/0003-4819-141-8-200410190-00005. PMID 15492337.
- ↑ Nickel JC, Downey J, Clark J, et al. (2003). "Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial". Urology. 62 (4): 614–7. doi:10.1016/S0090-4295(03)00583-1. PMID 14550427.
- ↑ Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS (2006). "WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity". BMC Public Health. 6: 177. doi:10.1186/1471-2458-6-177. PMC 1550236
 . PMID 16824213.
. PMID 16824213. - ↑ Hsiao, Chun-Ju (3 November 2010). "National Ambulatory medical Care Survey: 2007 Summary" (PDF). National Health Statistics Report. Centers for Disease Control. Retrieved 1 September 2013.
- ↑ Hall, Helen; Cramer, Holger; Sundberg, Tobias; Ward, Lesley; Adams, Jon; Moore, Craig; Sibbritt, David; Lauche, Romy (2016). "The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain". Medicine. 95 (38): e4723. doi:10.1097/MD.0000000000004723. PMC 5044890
 . PMID 27661020.
. PMID 27661020. - 1 2 3 4 5 Grace, Victoria (2000). "Pitfalls of the medical paradigm in chronic pelvic pain". Best practice & research. Clinical obstetrics & gynaecology. 14 (3): 527.
- ↑ UCPPS Society
- ↑ J Quentin Clemens, Chris Mullins, John W Kusek, Ziya Kirkali, Emeran A Mayer, Larissa V Rodríguez, David J Klumpp, Anthony J Schaeffer, Karl J Kreder, Dedra Buchwald, Gerald L Andriole, M Scott Lucia, J Richard Landis, Daniel J Clauw, The MAPP Research Network Study Group (1 August 2014). "The MAPP research network: a novel study of urologic chronic pelvic pain syndromes". BMC Urology. 14 (57). doi:10.1186/1471-2490-14-57. PMC 4134515
 . PMID 25085007.
. PMID 25085007. - 1 2 MAPP Research Network
- ↑ H. Henry Lai; John N. Krieger; Michel A. Pontari; Dedra Buchwald; Xiaoling Hou; J. Richard Landis (December 2015). "Painful Bladder Filling and Painful Urgency Are Distinct Characteristics in Men and Women with Urologic Chronic Pelvic Pain Syndromes – A MAPP Research Network Study". The Journal of Urology. 194 (6): 1634–1641. doi:10.1016/j.juro.2015.05.105. PMC 4669971
 . PMID 26192257.
. PMID 26192257.
External links
- International Pelvic Pain Society
- American Pain Society
- University of Michigan Pelvic Pain Program
- University of North Carolina Pelvic Pain Program
- Tailbone pain (coccyx pain, coccydynia)