Pelvic congestion syndrome
| Pelvic congestion syndrome | |
|---|---|
 | |
| A very large (9cm) fibroid of the uterus which is causing pelvic congestion syndrome as seen on X-ray computed tomography | |
| Classification and external resources | |
| ICD-9-CM | 625.5 |
Pelvic congestion syndrome (also known as pelvic vein incompetence) is a chronic medical condition in women caused by varicose veins in the lower abdomen. The condition causes chronic pain, often manifesting as a constant dull ache, which can be aggravated by standing.[1] Early treatment options include pain medication, alternative therapies such as acupuncture, and suppression of ovarian function. Surgery can be done using noninvasive transcatheter techniques to embolize the varicose veins.[1] Up to 80% of women obtain relief using this method.
The condition can occur as a result of pregnancy or for unknown reasons.[2] The presence of estrogen in the body causes vasodilation, which can result in the accumulation of blood in the veins in the pelvic area.[3] Estrogen can weaken the vein walls, leading to the changes that cause varicosities.[2] Up to 15% of all women have varicose veins in the abdominal area, but not all have symptoms.[3]
Signs and symptoms
Women with this condition experience a constant pain that may be dull and aching, but is occasionally more acute. The pain is worse at the end of the day and after long periods of standing, and sufferers get relief when they lie down. The pain is worse during or after sexual intercourse, and can be worse just before the onset of the menstrual period.[2][3]
Women with pelvic congestion syndrome have a larger uterus and a thicker endometrium. 56% of women manifest cystic changes to the ovaries,[4] and many report other symptoms, such as dysmenorrhea, back pain, vaginal discharge, abdominal bloating, mood swings or depression, and fatigue.[2][3]
Diagnosis
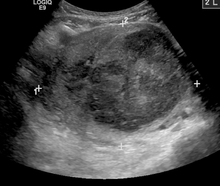
Diagnosis can be made using ultrasound or laparoscopy testing. The condition can also be diagnosed with a venogram, CT scan, or an MRI. Ultrasound is the diagnostic tool most commonly used.[2][3] Recent research from a leading pelvic venous unit has suggested that Transvaginal Duplex Ultrasound scanning is the "Gold Standard" test for pelvic venous reflux.[5] The same research group has shown that the size of the veins - as shown by venography and also used as the diagnostic criteria in CT and MRI - is not relevant and only Trannsvaginal Duplex Ultrasound shows the venous reflux that causes the problem.[6]
Treatment
Early treatment options include pain medication using nonsteroidal anti-inflammatory drugs,[3] suppression of ovarian function,[4] and alternative therapies such as acupuncture and physical therapy.[2]
The surgical option involves stopping blood flow to the varicose veins using noninvasive surgical techniques such as a procedure called embolization. The procedure requires an overnight stay in hospital, and is done using local anesthetic.[2][7] Patients report an 80% success rate, as measured by the amount of pain reduction experienced.[7]
See also
References
- 1 2 "Nonsurgical Treatment for Chronic Pelvic Pain in Women - SIR". sirweb.org. Retrieved February 5, 2011.
- 1 2 3 4 5 6 7 "Pelvic Congestion Syndrome". veindirectory.org. November 9, 2009. Retrieved December 23, 2010.
- 1 2 3 4 5 6 "Dysmenorrhea". Merck Online Medical Manual. December 2008. Retrieved December 23, 2010.
- 1 2 Phillip Reginald, MD. "Pelvic Congestion" (PDF). The International Pelvic Pain Society. Retrieved December 23, 2010.
- ↑ Whiteley M, Dos Santos S, Harrison C, Holdstock J, Lopez A. (Oct 2014). "Transvaginal duplex ultrasonography appears to be the gold standard investigation for the haemodynamic evaluation of pelvic venous reflux in the ovarian and internal iliac veins in women.". Phlebology. Retrieved January 7, 2015.
- ↑ Dos Santos SJ, Holdstock JM, Harrison CC, Lopez AJ, Whiteley MS. (Nov 2014). "Ovarian Vein Diameter Cannot Be Used as an Indicator of Ovarian Venous Reflux.". Eur J Vasc Endovasc Surg. Retrieved January 7, 2015.
- 1 2 "Pelvic Pain (Pelvic Congestion Syndrome)". Johns Hopkins. Retrieved December 23, 2010.