Panobinostat
 | |
| Clinical data | |
|---|---|
| Trade names | Farydak |
| Routes of administration | Oral (capsules) |
| ATC code | L01XX42 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 21%[1] |
| Protein binding | 90%[1] |
| Metabolism | CYP3A (40%), CYP2D6, CYP2C19[1] |
| Biological half-life | 37 hours[1] |
| Excretion | Fecal (44–77%), renal (29–51%)[1] |
| Identifiers | |
| |
| CAS Number |
404950-80-7 |
| PubChem (CID) | 6918837 |
| IUPHAR/BPS | 7489 |
| ChemSpider |
5294028 |
| UNII |
9647FM7Y3Z |
| KEGG |
D10019 |
| ChEBI |
CHEBI:85990 |
| ECHA InfoCard | 100.230.582 |
| Chemical and physical data | |
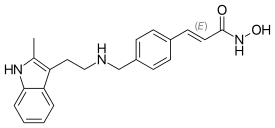
| Formula | C21H23N3O2 |
| Molar mass | 349.42622 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Panobinostat (LBH-589, trade name Farydak FAYR-ah-dak) is a drug developed by Novartis for the treatment of various cancers. It is a hydroxamic acid[2] and acts as a non-selective histone deacetylase inhibitor (pan-HDAC inhibitor).[3]
On 23 February 2015 it received FDA accelerated approval for use in patients with multiple myeloma who had received at least 2 previous treatments, including bortezomib and an immunomodulatory agent.[4][5]
Clinical trials
As of August 2012, it is being tested against Hodgkin's Lymphoma, cutaneous T cell lymphoma (CTCL)[6] and other types of malignant disease in Phase III clinical trials, against myelodysplastic syndromes, breast cancer and prostate cancer in Phase II trials, and against chronic myelomonocytic leukemia (CMML) in a Phase I trial.[7][8]
As of 2014 panobinostat is being used in a Phase I/II clinical trial that aims at curing AIDS in patients on highly active antiretroviral therapy (HAART). In this technique, panobinostat is used to drive the HIV DNA out of the patient's DNA, in the expectation that the patient's immune system in combination with HAART will destroy it.[9][10][11]
As of 2016 panobinostat is being studied in a phase II trial for relapsed and refractory diffuse large B-cell lymphoma (DLBCL).[12]
Preclinical studies
Panobinostat has been found to synergistically act with sirolimus to kill pancreatic cancer cells in the laboratory in a Mayo Clinic study. In the study, investigators found that this combination destroyed up to 65 percent of cultured pancreatic tumor cells. The finding is significant because the three cell lines studied were all resistant to the effects of chemotherapy – as are many pancreatic tumors.[13]
Panobinostat has also been found to significantly increase in vitro the survival of motor neuron (SMN) protein levels in cells of patients suffering from spinal muscular atrophy.[14]
Panobinostat was able to selectively target triple negative breast cancer (TNBC) cells by inducing hyperacetylation and cell cycle arrest at the G2-M DNA damage checkpoint; partially reversing the morphological changes characteristic of breast cancer cells.[15]
Panobinostat, along with other HDAC inhibitors, is also being studied for potential to induce virus HIV-1 expression in latently infected cells and disrupt latency. These resting cells are not recognized by the immune system as harboring the virus and do not respond to antiretroviral drugs.[16]
A 2015 study suggested Panobinostat was effective in preventing diffuse intrinsic pontine glioma cell growth in vitro and in vivo, identifying it as a potential drug candidate.[17]
Mechanism of action
Panobinostat inhibits multiple histone deacetylase enzymes, a mechanism leading to apoptosis of malignant cells via multiple pathways.[2]
References
- 1 2 3 4 5 Panobinostat Package Insert
- 1 2 Revill, P; Mealy, N; Serradell, N; Bolos, J; Rosa, E (2007). "Panobinostat". Drugs of the Future. 32 (4): 315. doi:10.1358/dof.2007.032.04.1094476. ISSN 0377-8282.
- ↑ Table 3: Select epigenetic inhibitors in various stages of development from Mack, G. S. (2010). "To selectivity and beyond". Nature Biotechnology. 28 (12): 1259–1266. doi:10.1038/nbt.1724. PMID 21139608.
- ↑ FDA.gov announcement about accelerated approval of panobinostat (Farydak)
- ↑ Panobinostat chemotherapy regimen for multiple myeloma (MM wiki)
- ↑ Clinical trial number NCT00425555 for "Study of Oral LBH589 in Adult Patients With Refractory Cutaneous T-Cell Lymphoma" at ClinicalTrials.gov
- ↑ ClinicalTrials.gov: LBH-589
- ↑ Prince, HM; M Bishton (2009). "Panobinostat (LBH589): a novel pan-deacetylase inhibitor with activity in T cell lymphoma". Hematology Meeting Reports. Parkville, Australia: Peter MacCallum Cancer Centre and University of Melbourne. 3 (1): 33–38.
- ↑ Simons, J (27 April 2013). "Scientists on brink of HIV cure". The Telegraph.
- ↑ Clinical trial number NCT01680094 for "Safety and Effect of The HDAC Inhibitor Panobinostat on HIV-1 Expression in Patients on Suppressive HAART (CLEAR)" at ClinicalTrials.gov
- ↑ Rasmussen, T. A.; Tolstrup, M.; Brinkmann, C. R.; Olesen, R.; Erikstrup, C.; Solomon, A.; Winckelmann, A.; Palmer, S.; Dinarello, C.; Buzon, M.; Lichterfeld, M.; Lewin, S. R.; Østergaard, L.; Søgaard, O. S. (2014). "Panobinostat, a histone deacetylase inhibitor, for latent-virus reactivation in HIV-infected patients on suppressive antiretroviral therapy: A phase 1/2, single group, clinical trial". The Lancet HIV. 1: e13. doi:10.1016/S2352-3018(14)70014-1.
- ↑ Panobinostat May Be Active in Select Patients With Refractory DLBCL. May 2016
- ↑ Mayo Clinic Researchers Formulate Treatment Combination Lethal To Pancreatic Cancer Cells
- ↑ Garbes, L; Riessland, M; Hölker, I; Heller, R; Hauke, J; Tränkle, Ch; Coras, R; Blümcke, I; Hahnen, E; Wirth, B (2009). "LBH589 induces up to 10-fold SMN protein levels by several independent mechanisms and is effective even in cells from SMA patients non-responsive to valproate". Human Molecular Genetics. 18 (19): 3645–3658. doi:10.1093/hmg/ddp313. PMID 19584083.
- ↑ Tate, CR; Rhodes, LV; Segar, HC; Driver, JL; Pounder, FN; Burow, ME; Collins-Burow, BM (2012). "Targeting triple-negative breast cancer cells with the histone deacetylase inhibitor panobinostat". Breast Cancer Research. 14 (3). doi:10.1186/bcr3192.
- ↑ TA Rasmussen, et al. Comparison of HDAC inhibitors in clinical development: Effect on HIV production in latently infected cells and T-cell activation. Human Vaccines & Immunotherapeutics 9:5, 1-9, May 2013.
- ↑ Grasso, Catherine (4 May 2015). "Functionally defined therapeutic targets in diffuse intrinsic pontine glioma". Nature Medicine. 21: 555–559. doi:10.1038/nm.3855. Retrieved 5 May 2015.