Opioid use disorder
| Opioid use disorder | |
|---|---|
| Synonyms | Opioid addiction and dependence |
 | |
| Classification and external resources | |
| Specialty | psychiatry |
| ICD-10 | F11.2 |
| ICD-9-CM | 304.0 |
| MeSH | D009293 |
An opioid use disorder is a medical condition that is characterized by the compulsive use of opioids despite adverse consequences from continued use and the development of a withdrawal syndrome when opioid use stops. It involves both an addiction to and dependence upon opioids.
Opioids include substances such as morphine, heroin, codeine, oxycodone, hydrocodone, etc. The necessary descriptive characteristics of the medical diagnosis are preoccupation with a desire to obtain and take the drug and persistent drug-seeking behaviour. The opioid dependence-withdrawal syndrome involves both psychological dependence and marked physical dependence upon opioid compounds.
Opioid use disorders resulted in 51,000 deaths worldwide in 2013, up from 18,000 deaths in 1990.[1]
Symptoms of withdrawal
Symptoms of withdrawal from opiates include, but are not limited to:[3]
Early symptoms
- Altered perception of temperature (hot/cold flashes)
- Agitation
- Anxiety
- Change in libido (abnormally high or low)
- Dehydration
- Fatigue
- Muscle aches
- Mental fog/confusion/lack of motivation
- Increased tearing
- Insomnia
- Restless legs
- Runny nose
- Sweating
- Yawning
- Skin-Crawling
Late symptoms
- Abdominal cramping
- Sneezing
- Diarrhea
- Dilated pupils
- Goose bumps
- Nausea
- Vomiting
Cause
Most people who are opioid-dependent have at least one other psychiatric comorbidity.[4] Opioid dependence often develops as a result of self medication.[4] Opioids are excellent acute pain medication, but it is their ability to produce euphoria that makes them attractive to addicts.[5] Scoring systems have been derived to assess the likelihood of opiate addiction in chronic pain patients.[6]
Mechanism
Addiction
Overexpression of the gene transcription factor "ΔFosB" in the nucleus accumbens plays a crucial role in the development of opioid addiction by directly modulating compulsive drug-seeking behaviors.[7][8][9]
Like many other forms of behavioral addiction and drug addiction, overuse of opiates leads to increased ΔFosB expression in the nucleus accumbens.[8][9][10] Opiates affect dopamine neurotransmission in the nucleus accumbens through their disinhibition of the GABA-based negative dopaminergic feedback system in the rostromedial tegmental nucleus.[11][12][13]
Dependence
Some studies suggest a permanent dysregulation of the endogenous opioid receptor system after chronic exposure to opioids. A recent study has shown that an increase in brain-derived neurotrophic factor (BDNF) in the ventral tegmental area (VTA) in rats can cause opiate-naive rats to begin displaying opiate-dependent behavior, including withdrawal and drug-seeking behavior.[14] It has been shown that when an opiate-naive person begins using opiates at levels inducing euphoria, this same increase in BDNF occurs.[15]
Upregulation of the cyclic adenosine monophosphate (cAMP) signal transduction pathway by cAMP response element binding protein (CREB), a gene transcription factor, in the nucleus accumbens is a common mechanism of psychological dependence among several classes of drugs of abuse.[7][16] Upregulation of the same pathway in the locus coeruleus is also a mechanism responsible for certain aspects of opioid-induced physical dependence.[16]
Opioid receptors
A genetic basis for the efficacy of opioids in the treatment of pain has been demonstrated for a number of specific variations; however, the evidence for clinical differences in opioid effects is ambiguous. The pharmacogenomics of the opioid receptors and their endogenous ligands have been the subject of intensive activity in association studies. These studies test broadly for a number of phenotypes, including opioid dependence, cocaine dependence, alcohol dependence, methamphetamine dependence/psychosis, response to naltrexone treatment, personality traits, and others. Major and minor variants have been reported for every receptor and ligand coding gene in both coding sequences, as well as regulatory regions. Newer approaches shift away from analysis of specific genes and regions, and are based on an unbiased screen of genes across the entire genome, which have no apparent relationship to the phenotype in question. These GWAS studies yield a number of implicated genes, although many of them code for seemingly unrelated proteins in processes such as cell adhesion, transcriptional regulation, cell structure determination, and RNA, DNA, and protein handling/modifying.[17]
Currently there are no specific pharmacogenomic dosing recommendations for opioids due to a lack of clear evidence connecting genotype to drug effect, toxicity, or likelihood of dependence.
118A>G variant
While over 100 variants have been identified for the opioid mu-receptor, the most studied mu-receptor variant is the non-synonymous 118A>G variant, which results in functional changes to the receptor, including lower binding site availability, reduced mRNA levels, altered signal transduction, and increased affinity for beta-endorphin. In theory, all of these functional changes would reduce the impact of exogenous opioids, requiring a higher dose to achieve the same therapeutic effect. This points to a potential for a greater addictive capacity in these individuals who require higher dosages to achieve pain control. However, evidence linking the 118A>G variant to opioid dependence is mixed, with associations shown in a number of study groups, but negative results in other groups. One explanation for the mixed results is the possibility of other variants which are in linkage disequilibrium with the 118A>G variant and thus contribute to different haplotype patterns that more specifically associate with opioid dependence.[18]
Non-opioid receptor genes
The preproenkephalin gene, PENK, encodes for the endogenous opiates that modulate pain perception, and are implicated in reward and addiction. (CA) repeats in the 3' flanking sequence of the PENK gene was associated with greater likelihood of opiate dependence in repeated studies. Variability in the MCR2 gene, encoding melanocortin receptor type 2 has been associated with both protective effects and increased susceptibility to heroin addiction. The CYP2B6 gene of the cytochrome P450 family also mediates breakdown of opioids and thus may play a role in dependence and overdose.[19]
Diagnosis
The WHO and DSM-IV-TR clinical guidelines for a definite diagnosis require that three or more of the following six characteristic features be experienced or exhibited:
- A strong desire or sense of compulsion to take the drug;
- Difficulties in controlling drug-taking behaviour in terms of its onset, termination, or levels of use;
- A physiological withdrawal state when drug use is stopped or reduced, as evidenced by: the characteristic withdrawal syndrome for the substance; or use of the same (or a closely related) substance with the intention of relieving or avoiding withdrawal symptoms;
- Evidence of tolerance, such that increased doses of the drug are required in order to achieve effects originally produced by lower doses;
- Progressive neglect of alternative pleasures or interests because of drug use, increased amount of time necessary to obtain or take the drug or to recover from its effects;
- Persisting with drug use despite clear evidence of overtly harmful consequences, such as harm to the liver, depressive mood states or impairment of cognitive functioning.
According to position papers on the treatment of opioid dependence published by the United Nations Office on Drugs and Crime and the World Health Organization, care providers should not treat opioid dependence as the result of a weak character or will.[20][21] Accordingly, detoxification alone does not constitute adequate treatment.
Management
Opioid dependence requires long-term treatment and care with the goals of reducing health risks for the consumer, reducing criminal behaviour, and improving the long-term physical and psychological condition of the addicted person.[21] Most strategies aim ultimately to reduce drug use and lead to abstinence.[21]
No single treatment works for everyone, so several strategies have been developed including therapy and drugs.[21][22]
Detox programs are rarely a good solution, and people often relapse after going through them, but it is an important first step.[21]
As of 2013 in the US, there was a significant increase of prescription opioid abuse compared to illegal opiates like heroin.[23] This development has also implications for the prevention, treatment and therapy of opioid dependence.[24]
Medications
Opioid replacement therapy (ORT) (also called opioid substitution therapy or opioid maintenance therapy) involves replacing an illegal opioid, such as heroin, with a longer acting but less euphoric opioid; methadone or buprenorphine are typically used and the drug is taken under medical supervision.[25]
The driving principle behind ORT is the program's capacity to facilitate a resumption of stability in the user's life, while the patient experiences reduced symptoms of drug withdrawal and less intense drug cravings; a strong euphoric effect is not experienced as a result of the treatment drug.[25] In some countries (not the US, or Australia),[25] regulations enforce a limited time period for people on ORT programs that conclude when a stable economic and psychosocial situation is achieved. (Patients suffering from HIV/AIDS or Hepatitis C are usually excluded from this requirement.) In practice, 40-65% of patients maintain complete abstinence from opioids while receiving opioid replacement therapy, and 70-95% are able to reduce their use significantly, while experiencing a concurrent elimination or reduction in medical (improper diluents, non-sterile injecting equipment), psychosocial (mental health, relationships), and legal (arrest and imprisonment) issues that can arise from the use of illegal opioids.[25] Clonidine or lofexidine can help treat the symptoms of withdrawal.[26]
ORT has proven to be the most effective treatment for improving the health and living condition of people experiencing problematic illegal opiate use or dependence, including mortality reduction[25][27] and overall societal costs, such as the economic loss from drug-related crime and healthcare expenditure.[25] Opioid Replacement Therapy is endorsed by the World Health Organization, United Nations Office on Drugs and Crime and UNAIDS as being effective at reducing injection, lowering risk for HIV/AIDS, and promoting adherence to antiretroviral therapy.[28] Currently, 55 countries worldwide use methadone replacement therapy, while some countries such as Russia do not offer it.[29]
Methadone

Methadone maintenance treatment (MMT), a form of opioid replacement therapy, reduces and/or eliminates the use of illegal opiates, the criminality associated with opiate use, and allows patients to improve their health and social productivity.[30][31] In addition, enrollment in methadone maintenance has the potential to reduce the transmission of infectious diseases associated with opiate injection, such as hepatitis and HIV.[30] The principal effects of methadone maintenance are to relieve narcotic craving, suppress the abstinence syndrome, and block the euphoric effects associated with opiates. Methadone maintenance has been found to be medically safe and non-sedating.[30] It is also indicated for pregnant women addicted to opiates.[30] Methadone maintenance treatment is given to addicted individuals who feel unable to go the whole way and get clean. For those individuals who wish to completely move away from drugs, a methadone reduction program is indicated, where the individual is prescribed an amount of methadone which is titrated up until withdrawal symptoms subside, followed by a period of stability, the dose will then be gradually reduced until the individual is either free of the need for methadone or is at a level which allows a switch to a different opiate with an easier withdrawal profile, such as Suboxone.[32] Methadone toxicity has been shown to be associated with specific phenotypes of CYP2B6.[33]
Buprenorphine

Studies have shown buprenorphine to be a safer alternative over methadone in opiate replacement therapy, primarily due to its lower instance of overdose related deaths during the course of treatment.[34] Buprenorphine sublingual preparations are often used to manage opioid dependence (that is, dependence on heroin, oxycodone, hydrocodone, morphine, oxymorphone, fentanyl or other opioids). The Suboxone and Subutex preparations were approved for this indication by the United States Food and Drug Administration in October 2002.[35] Some formulations of buprenorphine incorporate the opiate antagonist naloxone during the production of the pill form to prevent people from crushing the tablets and injecting them, instead of using the sublingual (under the tongue) route of administration.[25]
Diamorphine
In Switzerland, Germany, the Netherlands, and the United Kingdom, long-term injecting drug users who do not benefit from methadone and other medication options are treated with pure injectable diamorphine that is administered under the supervision of medical staff. For this group of patients, diamorphine treatment has proven superior in improving their social and health situation.[36]
Dihydrocodeine
Dihydrocodeine in both extended-release and immediate-release form are also sometimes used for maintenance treatment as an alternative to methadone or buprenorphine in some European countries.[37]
Heroin-assisted treatment
Heroin-assisted treatment (HAT, the medical prescription of heroin) has been available in Switzerland since 1994.[38] A 2001 study found a high rate of treatment retention and significant improvement in health, social situation and likelihood to leave the illegal drug scene in enrolled participants.[38] The study found that the most common reason for discharge was the start of abstinence treatment or methadone treatment.[38] The study also found that heroin-assisted treatment is cost-beneficial on a society level due to reduced criminality and improved overall health of participants.[38]
The heroin-assisted treatment program was introduced in Switzerland to combat the increase in heroin use in the 1980s and 1990s and written into law 2010 as one pillar of a four-pillar strategy using repression, prevention, treatment and risk reduction.[39] Usually, only a small percentage of patients receive heroin and have to fulfil a number of criteria.[40][41] Since then, HAT programs have been adopted in the Netherlands, United Kingdom, Germany, Spain, Denmark, Belgium, Canada, and Luxembourg.[42]
LAAM
Levacetylmethadol was previously used to treat opioid dependence. In 2003 the drug's manufacturer discontinued production. There are no available generic versions. LAAM produced long-lasting effects, which allowed the person receiving treatment to visit a clinic only three times per week, as opposed to daily as with methadone.[43] In 2001, levacetylmethadol was removed from the European market due to reports of life-threatening ventricular rhythm disorders.[44] In 2003, Roxane Laboratories, Inc. discontinued Orlaam in the US.[45]
Morphine (extended-release)
According to a Cochrane review in 2013, extended-release morphine confers a possible reduction of opioid use and with fewer depressive symptoms but overall more adverse effects when compared to other forms of long-acting opioids. Retention in treatment was not found to be significantly different.[46] It used in Switzerland.[40]
Naltrexone
Naltrexone was approved by the FDA in 1984 for the treatment of opioid dependence. It is available both as an oral medication and as a monthly injectable (approved in 2010). Some authors question whether oral Naltrexone is as effective in the treatment of opioid dependence as methadone and buprenorphine mainly due to non-compliance.[47]
Therapy
12-step support groups
While medical treatment may help with the initial symptoms of opioid withdrawal, once an opiate addict overcomes the first stages of withdrawal, a method for long-term preventative care is attendance at 12-step groups such as Alcoholics Anonymous or Narcotics Anonymous. Attendance and participation in a 12 step program is an effective way to obtain and maintain sobriety.[48] Among primarily inner city minorities who had a "long severe history of (primarily) crack and/or heroin use", 51.7% of the individuals with continuous 12-step attendance had over 3 years of sustained abstinence, in contrast to 13.5% among those who had less than continuous 12-step attendance.[49][50]
Epidemiology
Opioid use disorders resulted in 51,000 deaths in 2013 up from 18,000 deaths in 1990.[1] Deaths from all causes rose from 47.5 million in 1990 to 54.9 million in 2013.[1]
United States
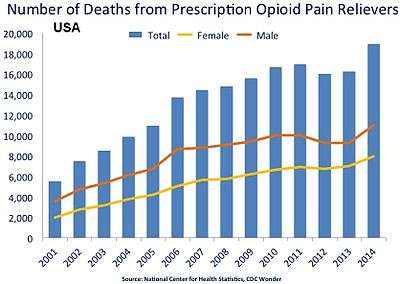
Non-medical consumption of opioids peaked around 2010 and then started to decrease between 2011 and 2013.[51]
Among adults, the rate of inpatient hospital stays in the United States related to opioid overuse increased by an average of 5% annually from 1993–2012. The percentage of inpatient stays due to opioid overuse that were admitted from the emergency department increased from 43% in 1993 to 64% in 2005, but have remained relatively constant since.[52]
The prevalence of opioid use and opioid or opiate dependency varies by age and gender, among a myriad of other factors. Men are at higher risk for opioid use and dependency than women,[53][54] and men also account for more opioid overdoses than women, although this gap is closing.[53] Women are more likely to be prescribed pain relievers, be given higher doses, use them for longer durations, and may become dependent upon them faster.[55]
Deaths due to opioid use also tend to skew at older ages than deaths from use of other illicit drugs.[54][56][57] This does not reflect opioid use as a whole, which includes individuals in younger age demographics. Overdoses from opioids are highest among individuals who are between the ages of 40 and 50,[57] in contrast to heroin overdoses, which are highest among individuals who are between the ages of 20 and 30.[56] 21 to 35-year olds represent 77% of individuals who enter treatment for opioid use disorder,[58] however, the average age of first-time use of prescription painkillers was 21.2 years of age in 2013.[59]
Research
Each of these treatments is experimental, and some remain quite far from having been proven to be effective.
See also
- Benzodiazepine withdrawal syndrome
- Doctor shopping
- Opioid receptor
- Physical dependence
- Post-acute-withdrawal syndrome
- Prescription drug abuse
- Walid–Robinson Opioid-Dependence Questionnaire
References
- 1 2 3 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet. 385: 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604
 . PMID 25530442.
. PMID 25530442. - ↑ Overdose Death Rates. By National Institute on Drug Abuse (NIDA).
- ↑ "Opiate withdrawal". Medline Plus. Retrieved 1 November 2014.
- 1 2 Chen, Kevin W.; Banducci, Annie N.; Guller, Leila; MacAtee, Richard J.; Lavelle, Anna; Daughters, Stacey B.; Lejuez, C.W. (2011). "An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program". Drug and Alcohol Dependence. 118 (2–3): 92–9. doi:10.1016/j.drugalcdep.2011.03.003. PMC 3188332
 . PMID 21514751.
. PMID 21514751. - ↑ Praveen, KT; Law, F; O'Shea, J; Melichar, J (2012). "Opioid dependence". American family physician. 86 (6): 565–6. PMID 23062049.
- ↑ Webster, L. R.; Webster, R. M. (2005). "Predicting aberrant behaviors in opioid-treated patients: Preliminary validation of the Opioid Risk Tool". Pain Medicine. 6 (6): 432–42. doi:10.1111/j.1526-4637.2005.00072.x. PMID 16336480.
- 1 2 Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues Clin Neurosci. 15 (4): 431–443. PMC 3898681
 . PMID 24459410.
. PMID 24459410. DESPITE THE IMPORTANCE OF NUMEROUS PSYCHOSOCIAL FACTORS, AT ITS CORE, DRUG ADDICTION INVOLVES A BIOLOGICAL PROCESS: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. ... A large body of literature has demonstrated that such ΔFosB induction in D1-type NAc neurons increases an animal's sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement
- 1 2 Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nat. Rev. Neurosci. 12 (11): 623–637. doi:10.1038/nrn3111. PMC 3272277
 . PMID 21989194.
. PMID 21989194. ΔFosB has been linked directly to several addiction-related behaviors ... Importantly, genetic or viral overexpression of ΔJunD, a dominant negative mutant of JunD which antagonizes ΔFosB- and other AP-1-mediated transcriptional activity, in the NAc or OFC blocks these key effects of drug exposure14,22–24. This indicates that ΔFosB is both necessary and sufficient for many of the changes wrought in the brain by chronic drug exposure. ΔFosB is also induced in D1-type NAc MSNs by chronic consumption of several natural rewards, including sucrose, high fat food, sex, wheel running, where it promotes that consumption14,26–30. This implicates ΔFosB in the regulation of natural rewards under normal conditions and perhaps during pathological addictive-like states.
- 1 2 Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–22. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704
 . PMID 21459101.
. PMID 21459101. - ↑ Blum K, Werner T, Carnes S, Carnes P, Bowirrat A, Giordano J, Oscar-Berman M, Gold M (2012). "Sex, drugs, and rock 'n' roll: hypothesizing common mesolimbic activation as a function of reward gene polymorphisms". J. Psychoactive Drugs. 44 (1): 38–55. doi:10.1080/02791072.2012.662112. PMC 4040958
 . PMID 22641964.
. PMID 22641964. It has been found that deltaFosB gene in the NAc is critical for reinforcing effects of sexual reward. Pitchers and colleagues (2010) reported that sexual experience was shown to cause DeltaFosB accumulation in several limbic brain regions including the NAc, medial pre-frontal cortex, VTA, caudate, and putamen, but not the medial preoptic nucleus. Next, the induction of c-Fos, a downstream (repressed) target of DeltaFosB, was measured in sexually experienced and naive animals. The number of mating-induced c-Fos-IR cells was significantly decreased in sexually experienced animals compared to sexually naive controls. Finally, DeltaFosB levels and its activity in the NAc were manipulated using viral-mediated gene transfer to study its potential role in mediating sexual experience and experience-induced facilitation of sexual performance. Animals with DeltaFosB overexpression displayed enhanced facilitation of sexual performance with sexual experience relative to controls. In contrast, the expression of DeltaJunD, a dominant-negative binding partner of DeltaFosB, attenuated sexual experience-induced facilitation of sexual performance, and stunted long-term maintenance of facilitation compared to DeltaFosB overexpressing group. Together, these findings support a critical role for DeltaFosB expression in the NAc in the reinforcing effects of sexual behavior and sexual experience-induced facilitation of sexual performance. ... both drug addiction and sexual addiction represent pathological forms of neuroplasticity along with the emergence of aberrant behaviors involving a cascade of neurochemical changes mainly in the brain's rewarding circuitry.
- ↑ Bourdy R, Barrot M (November 2012). "A new control center for dopaminergic systems: pulling the VTA by the tail". Trends Neurosci. 35 (11): 681–690. doi:10.1016/j.tins.2012.06.007. PMID 22824232.
In light of the crucial role of the tVTA in the opiate control of dopamine activity ...
In the context of addiction, the tVTA is a target for psychostimulant-induced plasticity [1,6,23] and is also essential for morphine action on dopamine neurons [19]. This latter finding suggests that the classical disinhibition model may need to be revisited in light of the GABAergic control that the tVTA exerts on dopamine systems. ...
The tVTA is rich in inhibitory GABA neurons expressing μ-opioid receptors and sends extensive projections toward midbrain dopamine cells. It is proposed as a major brake for dopamine systems. - ↑ Barrot M, Sesack SR, Georges F, Pistis M, Hong S, Jhou TC (October 2012). "Braking dopamine systems: a new GABA master structure for mesolimbic and nigrostriatal functions". J. Neurosci. 32 (41): 14094–14101. doi:10.1523/JNEUROSCI.3370-12.2012. PMC 3513755
 . PMID 23055478.
. PMID 23055478. The tVTA/RMTg sends dense GABA projections to VTA and substantia nigra neurons. ...
Indeed, tVTA/RMTg cells express high levels of mu-opioid receptors (Jhou et al., 2009a, 2012; Jalabert et al., 2011), and in vivo, ex vivo and optogenetic electrophysiological approaches demonstrated that morphine excites dopamine neurons by targeting receptors localized to tVTA/RMTg cell bodies as well as its terminals within the VTA (Jalabert et al., 2011; Lecca et al., 2011; Matsui and Williams, 2011; Lecca et al., 2012). - ↑ "Morphine addiction – Homo sapiens (human)". KEGG. Kanehisa Laboratories. 18 June 2013. Retrieved 11 September 2014.
- ↑ Vargas-Perez, H.; Ting-A-Kee, R.; Walton, C. H.; Hansen, D. M.; Razavi, R.; Clarke, L.; Bufalino, M. R.; Allison, D. W.; Steffensen, S. C. (2009). "Ventral Tegmental Area BDNF Induces an Opiate-Dependent-Like Reward State in Naive Rats". Science. 324 (5935): 1732–34. doi:10.1126/science.1168501. PMC 2913611
 . PMID 19478142.
. PMID 19478142. - ↑ Laviolette, Steven R.; Van Der Kooy, Derek (2001). "GABAA receptors in the ventral tegmental area control bidirectional reward signalling between dopaminergic and non-dopaminergic neural motivational systems". European Journal of Neuroscience. 13 (5): 1009–15. doi:10.1046/j.1460-9568.2001.01458.x. PMID 11264674.
- 1 2 Nestler EJ (2015). "Reflections on: "A general role for adaptations in G-Proteins and the cyclic AMP system in mediating the chronic actions of morphine and cocaine on neuronal function"". Brain Res. doi:10.1016/j.brainres.2015.12.039. PMID 26740398.
These findings led us to hypothesize that a concerted upregulation of the cAMP pathway is a general mechanism of opiate tolerance and dependence. ... We thus extended our hypothesis to suggest that, particularly within brain reward regions such as NAc, cAMP pathway upregulation represents a common mechanism of reward tolerance and dependence shared by several classes of drugs of abuse. Research since that time, by many laboratories, has provided substantial support for these hypotheses. Specifically, opiates in several CNS regions including NAc, and cocaine more selectively in NAc, induce expression of certain adenylyl cyclase isoforms and PKA subunits via the transcription factor, CREB, and these transcriptional adaptations serve a homeostatic function to oppose drug action. In certain brain regions, such as locus coeruleus, these adaptations mediate aspects of physical opiate dependence and withdrawal, whereas in NAc they mediate reward tolerance and dependence that drives increased drug self-administration.
- ↑ Hall, F. Scott; Drgonova, Jana; Jain, Siddharth; Uhl, George R. (December 2013). "Implications of genome wide association studies for addiction: Are our a priori assumptions all wrong?". Pharmacology & Therapeutics. 140 (3): 267–279. doi:10.1016/j.pharmthera.2013.07.006.
- ↑ Bruehl, Stephen; Apkarian, A. Vania; Ballantyne, Jane C.; Berger, Ann; Borsook, David; Chen, Wen G.; Farrar, John T.; Haythornthwaite, Jennifer A.; Horn, Susan D.; Iadarola, Michael J.; Inturrisi, Charles E.; Lao, Lixing; Mackey, Sean; Mao, Jianren; Sawczuk, Andrea; Uhl, George R.; Witter, James; Woolf, Clifford J.; Zubieta, Jon-Kar; Lin, Yu (February 2013). "Personalized Medicine and Opioid Analgesic Prescribing for Chronic Pain: Opportunities and Challenges". The Journal of Pain. 14 (2): 103–113. doi:10.1016/j.jpain.2012.10.016. PMC 3564046
 . PMID 23374939.
. PMID 23374939. - ↑ Khokhar, Jibran Y.; Ferguson, Charmaine S.; Zhu, Andy Z.X.; Tyndale, Rachel F. (February 2010). "Pharmacogenetics of Drug Dependence: Role of Gene Variations in Susceptibility and Treatment". Annual Review of Pharmacology and Toxicology. 50 (1): 39–61. doi:10.1146/annurev.pharmtox.010909.105826.
- ↑ Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention (PDF). World Health Organization. 2004. ISBN 92-4-159115-3.
- 1 2 3 4 5 "Treatment of opioid dependence". WHO. Retrieved August 28, 2016.
- ↑ Nicholls L, Bragaw L, Ruetsch C (February 2010). "Opioid Dependence Treatment and guidelines". J Manag Care Pharm. 16 (1 Suppl B): S14–21. PMID 20146550.
- ↑ Matthew Daubresse; Patrick P. Gleason; Yi Peng; Nilay D. Shah; Stephen T. Ritter; G. Caleb Alexander (2013). "Impact of a drug utilization review program on high-risk use of prescription controlled substances". Pharmacoepidemiology and Drug Safety. 23: 419–427. doi:10.1002/pds.3487.
- ↑ Amy Maxmen (June 2012), "Tackling the US pain epidemic". Nature News doi:10.1038/nature.2012.10766
- 1 2 3 4 5 6 7 Richard P. Mattick et al.: National Evaluation of Pharmacotherapies for Opioid Dependence (NEPOD): Report of Results and Recommendation
- ↑ Gowing, L; Farrell, M; Ali, R; White, JM (3 May 2016). "Alpha₂-adrenergic agonists for the management of opioid withdrawal.". The Cochrane database of systematic reviews (5): CD002024. doi:10.1002/14651858.CD002024.pub5. PMID 27140827.
- ↑ Michel et al.: Substitution treatment for opioid addicts in Germany, Harm Reduct J. 2007; 4: 5.
- ↑ WHO; UNODC; UNAIDS (January 2013). WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users – 2012 revision. p. 13. ISBN 978 92 4 150437 9.
- ↑ Michael Schwartz (22 July 2008). "Russia Scorns Methadone for Heroin Addiction". The New York Times. Retrieved 5 April 2014.
- 1 2 3 4 Joseph, H; Stancliff, S; Langrod, J (2000). "Methadone maintenance treatment (MMT): A review of historical and clinical issues". The Mount Sinai journal of medicine, New York. 67 (5–6): 347–64. PMID 11064485.
- ↑ Connock, M; Juarez-Garcia, A; Jowett, S; Frew, E; Liu, Z; Taylor, RJ; Fry-Smith, A; Day, E; Lintzeris, N (2007). "Methadone and buprenorphine for the management of opioid dependence: A systematic review and economic evaluation". Health technology assessment. 11 (9): 1–171, iii–iv. doi:10.3310/hta11090. PMID 17313907.
- ↑ http://www.rcgp.org.uk-PDF-drug_meth%20guidance.
- ↑ Bunten, H; Liang, W J; Pounder, D J; Seneviratne, C; Osselton, D (28 July 2010). "OPRM1 and CYP2B6 Gene Variants as Risk Factors in Methadone-Related Deaths". Clinical Pharmacology & Therapeutics. 88 (3): 383–389. doi:10.1038/clpt.2010.127. PMID 20668445.
- ↑ Bell, J.R; Butler, B., Lawrence, A., Batey, R. & Salmelainen (2009). "Comparing overdose mortality associated with methadone and buprenorphine treatment". Drug and Alcohol Dependence. 104 (1–2): 73–7. doi:10.1016/j.drugalcdep.2009.03.020. PMID 19443138.
- ↑ "Subutex and Suboxone Approved to Treat Opiate Dependence". FDA. 8 October 2002. Retrieved 1 November 2014.
- ↑ Haasen, C.; Verthein, U.; Degkwitz, P.; Berger, J.; Krausz, M.; Naber, D. (2007). "Heroin-assisted treatment for opioid dependence: Randomised controlled trial". The British Journal of Psychiatry. 191: 55–62. doi:10.1192/bjp.bp.106.026112. PMID 17602126.
- ↑ Robertson, J. Roy; Raab, Gillian M.; Bruce, Malcolm; McKenzie, James S.; Storkey, Helen R.; Salter, Amy (2006). "Addressing the efficacy of dihydrocodeine versus methadone as an alternative maintenance treatment for opiate dependence: A randomized controlled trial". Addiction. 101 (12): 1752–9. doi:10.1111/j.1360-0443.2006.01603.x. PMID 17156174.
- 1 2 3 4 Rehm J, Gschwend P, Steffen T, Gutzwiller F, Dobler-Mikola A, Uchtenhagen A (2001). "Feasibility, safety, and efficacy of injectable heroin prescription for refractory opioid addicts: a follow-up study". Lancet. 358 (9291): 1417–23. doi:10.1016/S0140-6736(01)06529-1. PMID 11705488. Retrieved 2016-03-04.
- ↑ "Drogenpolitik: Heroinabgabe gemäss Experten ein Erfolg - NZZ Schweiz". Retrieved 2016-03-04.
- 1 2 "Bundesamt für Gesundheit - Substitutionsgestützte Behandlung mit Diacetylmorphin (Heroin)".
- ↑ "Dank der ärztlichen Heroinabgabe können rund 1400 Süchtige legal konsumieren – Einige schaffen den Anschluss an die Gesellschaft: Heroinsüchtige mitten im Leben - NZZ".
- ↑ "Heroin Assisted Treatment | Drug Policy Alliance". Retrieved 2016-03-04.
- ↑ James W. Kalat, Biological Psychology. Cengage Learning. Page 81.
- ↑ EMEA April 19, 2001 EMEA Public Statement on the Recommendation to Suspend the Marketing Authorisation for Orlaam (Levacetylmethadol) in the European Union
- ↑ US FDA Safety Alerts: Orlaam (levomethadyl acetate hydrochloride) Page Last Updated: Aug 20, 2013
- ↑ Ferri, Marica; Minozzi, Silvia; Bo, Alessandra; Amato, Laura; Ferri, Marica (2013). "Slow-release oral morphine as maintenance therapy for opioid dependence". Reviews. doi:10.1002/14651858.CD009879.pub2.
- ↑ Minozzi S, Amato L, Vecchi S, Davoli M, Kirchmayer U, Verster A (2011). "Oral naltrexone maintenance treatment for opioid dependence". Cochrane Database of Systematic Reviews (4): CD001333. doi:10.1002/14651858.CD001333.pub4. PMID 21491383.
- ↑ Brigham, Gregory (2003). "12-Step Participation as a Pathway to Recovery: The Maryhaven Experience and Implications for Treatment and Research". Science & Practice Perspectives. 2 (1): 43–51. doi:10.1151/spp032143. PMC 2851040
 . PMID 18552722.
. PMID 18552722. - ↑ "PPT – Alexandre B. Laudet, Ph.D PowerPoint presentation - free to view - id: 1460c1-YWY2O". PowerShow.
- ↑ Manning, V; Best D., Faulkner N., Titherington E., Morinan A., Keaney F., Gossop M., Strang J. (November 2012). "Does active referral by a doctor or 12-Step peer improve 12-Step meeting attendance? Results from a pilot randomised control trial". Drug Alcohol Depend; Research study. NCBI Pubmed.gov. 126 (1–2): 131–7. doi:10.1016/j.drugalcdep.2012.05.004. PMID 22677458.
- ↑ Wilkerson, Richard Gentry; Kim, Hong K.; Windsor, Thomas Andrew; Mareiniss, Darren P. (May 2016). "The Opioid Epidemic in the United States". Emergency Medicine Clinics of North America. 34 (2): e1–e23. doi:10.1016/j.emc.2015.11.002.
- ↑ Owens PL, Barrett ML, Weiss AJ, Washington RE, Kronick R (August 2014). "Hospital Inpatient Utilization Related to Opioid Overuse Among Adults, 1993–2012". HCUP Statistical Brief #177. Rockville, MD: Agency for Healthcare Research and Quality.
- 1 2 "Prescription Opioid Overdose Data". Center for Disease Control and Prevention. Retrieved 12 September 2016.
- 1 2 Paulozzi, Len (12 April 2012). "Populations at risk for opioid overdose" (PDF). FDA. Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control Centers for Disease Control and Prevention. Retrieved 12 September 2016.
- ↑ "Opioid Addiction: 2016 Facts and Figures" (PDF). American Society of Addiction Medicine. Retrieved 12 September 2016.
- 1 2 "How Bad is the Opioid Epidemic?". Retrieved 2016-09-12.
- 1 2 Han, Benjamin; Polydorou, Soteri; Ferris, Rosie; Blaum, Caroline S.; Ross, Stephen; McNeely, Jennifer (2015-11-10). "Demographic Trends of Adults in New York City Opioid Treatment Programs—An Aging Population". Substance Use & Misuse. 50 (13): 1660–1667. doi:10.3109/10826084.2015.1027929. ISSN 1082-6084. PMID 26584180.
- ↑ "Facts & Faces of Opioid Addiction: New Insights". MAP Health Management. 2015. Retrieved 12 September 2016.
- ↑ "Opioids". Substance Abuse and Mental Health Services Administration. 23 February 2016. Retrieved 12 September 2016.
- ↑ Brewer, C; H Rezae, C Bailey (1988). "Opioid withdrawal and naltrexone induction in 48–72 hours with minimal drop-out, using a modification of the naltrexone-clonidine technique". The British Journal of Psychiatry. 153 (3): 340–343. doi:10.1192/bjp.153.3.340. PMID 3250670.
- ↑ Ling, W; L Amass, S Shoptaw, JJ Annon, M Hillhouse, D Babcock, G Brigham, J Harrer, M Reid, J Muir, B Buchan, D Orr, G Woody, J Krejci, D Ziedonis (2005). "A multi-center randomized trial of buprenorphine–naloxone versus clonidine for opioid, detoxification: findings from the National Institute on Drug Abuse Clinical Trials Network". Addiction. 100 (8): 1090–1100. doi:10.1111/j.1360-0443.2005.01154.x. PMC 1480367
 . PMID 16042639.
. PMID 16042639. - 1 2 Herman, BH; F Vocci, P Bridge (1995). "The effects of NMDA receptor antagonists and nitric oxide synthase inhibitors on opioid tolerance and withdrawal: Medication development issues for opiate addiction" (PDF). Neuropsychopharmacology. 13 (4): 269–293. doi:10.1016/0893-133X(95)00140-9. PMID 8747752.
- ↑ Alper, Kenneth R.; Lotsof, Howard S.; Kaplan, Charles D. (January 2008). "The ibogaine medical subculture". Journal of Ethnopharmacology. 115 (1): 9–24. doi:10.1016/j.jep.2007.08.034. PMID 18029124.
- ↑ Boyer, Edward W.; Kavita M. Babu, Jessica E. Adkins, Christopher R. McCurdy, John H. Halpern (28 June 2008). "Self-treatment of opioid withdrawal using kratom (Mitragynia speciosa korth)". Addiction. 103 (6): 1048–1050. doi:10.1111/j.1360-0443.2008.02209.x. PMC 3670991
 . PMID 18482427.
. PMID 18482427.
External links
- Heroin information from the National Institute on Drug Abuse
- Opioid information at Opioids.Net
- Opioid Dependence Treatment and Guidelines
- Opioid Risk Tool (ORT) for Narcotic Abuse