Omenn syndrome
| Omenn syndrome | |
|---|---|
| Classification and external resources | |
| Specialty | hematology |
| ICD-10 | D81.2 (ILDS D81.210) |
| OMIM | 603554 |
| DiseasesDB | 32676 |
| eMedicine | ped/1640 |
| MeSH | D016511 |
| Orphanet | 39041 |
Omenn syndrome is an autosomal recessive severe combined immunodeficiency[1] associated with hypomorphic missense mutations in immunologically relevant genes of T-cells (and B-cells) as recombination activating genes (RAG1 and RAG2), IL-7 Receptor α gene (IL7Rα), DCLRE1C-Artemis, RMRP-CHH, DNA-Ligase IV, common gamma chain, WHN-FOXN1, ZAP-70 and complete DiGeorge anomaly (DiGeorge Syndrome; CHARGE).
Symptoms

The symptoms are very similar to graft-versus-host disease (GVHD). This is because the patients have some T cells with limited levels of recombination with the mutant RAG genes. These T cells are abnormal and have a very specific affinity for self antigens found in the thymus and in the periphery. Therefore, these T cells are auto-reactive and cause the GVHD phenotype.
A characteristic symptom is chronic inflammation of the skin, which appears as a red rash[2] (early onset erythroderma). Other symptoms include eosinophilia, failure to thrive, swollen lymph nodes, swollen spleen, diarrhea, enlarged liver, low immunoglobulin levels (except immunoglobulin E, which is elevated), low T cell levels, and no B cells.[3]
Genetics
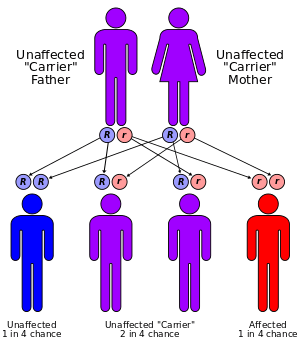
Omenn syndrome is caused by a partial loss of RAG gene function and leads to symptoms similar to severe combined immunodeficiency syndrome, including opportunistic infections. The RAG genes are essential for gene recombination in the T-cell receptor and B-cell receptor, and loss of this ability means that the immune system has difficulty recognizing specific pathogens.[2] For the Omen Syndrom is the loss of T-cell function the important defect, that leads to engraftment of maternal lymphocytes in the foetus and a co-existence of clonally expanded autologous and transplacental-acquired maternal lymphocytes.[4] Omenn syndrome can occasionally be caused in other recombination genes, including IL-7Rα and RMRP.[3]
Treatment
The only treatment for Omenn syndrome is bone marrow transplantation. Without treatment, it is rapidly fatal in infancy.[2] The disease can be cured by bone marrow transplantation.[3]
See also
References
- ↑ Santagata S, Villa A, Sobacchi C, Cortes P, Vezzoni P (2000). "The genetic and biochemical basis of Omenn syndrome". Immunol Rev. 178: 64–74. doi:10.1034/j.1600-065X.2000.17818.x. PMID 11213808.
- 1 2 3 Parham, Peter (2009). The Immune System (3rd ed.). Taylor & Francis Group. p. 128. ISBN 9781136977107.
- 1 2 3 Geha, Raif; Notarangelo, Luigi (2012). Case Studies in Immunology: A Clinical Companion (6th ed.). Garland Science. ISBN 978-0-8153-4441-4.
- ↑ Lev A, Simon AJ, Ben-Ari J, Takagi D, Stauber T, Trakhtenbrot L, Rosenthal E, Rechavi G, Amariglio N, Somech R (2014). "Co-existence of clonal expanded autologous and transplacental-acquired maternal T cells in recombination activating gene-deficient severe combined immunodeficiency.". Clin Exp Immunol. 176 (3): 380–6. doi:10.1111/cei.12273. PMID 24666246.