Nicotine dependence
| Nicotine dependence | |
|---|---|
| Classification and external resources | |
| ICD-10 | F17.2 |
| ICD-9-CM | 305.1 |
| OMIM | 188890 |
Nicotine dependence is a state of dependence upon nicotine. There are different ways of measuring nicotine dependence. Some nicotine dependence assessments focus on key physical dependence outcomes like the development of tolerance which allows people to smoke heavily. Other assessments ask about psychosocial outcomes or underlying mechanisms of dependence. These different assessments either characterize dependence as a continuous construct or use cut-offs to diagnose whether someone is or is not dependent.
Nicotine dependence is especially a concern among some populations such as those with co-occurring mental illness. There are evidence-based nicotine dependence treatments that include both medication and psychosocial interventions that can significantly increase a smoker’s chances of quitting successfully.
Definition
Nicotine dependence develops over time as a person continues to smoke. The risk for the development of dependence and how long it takes to become dependent differs from person to person; there is not a clear consensus on how long it takes for dependence to develop.
Nicotine dependence results in daily, heavy usage of cigarettes and produces withdrawal symptoms such as urges to smoke, negative moods, and difficulty concentrating, when the person stops smoking. These withdrawal symptoms are so unpleasant that smokers very frequently return to smoking.[1][2][3] However, while it is known what nicotine dependence does--permits heavy smoking and causes severe withdrawal symptoms and relapse back to smoking[4]--it is hard to measure nicotine dependence apart from these consequences.
From a clinical perspective, nicotine dependence has been classified as a chronic, relapsing disease.[5] In other words, it is a long-term disorder that may have periods of relapse and remission that require repeated intervention, similar to other chronic conditions such as diabetes or hypertension. This perspective reinforces the idea that nicotine dependence is not a bad habit but an actual disease that requires ongoing treatment.
Assessment and diagnosis
Nicotine dependence is a complex construct and therefore it is challenging to measure. When it comes to assessing nicotine dependence, how one chooses to define it and/or the purpose of the assessment will guide which assessment to use. Some people distinguish between nicotine dependence and addiction, but, for the most part, nicotine dependence instruments ask about ideas that are thought of to be dependence and addiction. Thus the two terms are now often used interchangeably. For instance, someone could use a narrow definition of nicotine dependence that focused on physical dependence characterized as neuroadaptations—changes in the brain—produced by repeated smoking. This would lead them to use one type of assessment. On the other hand, someone could want to include other components such as the influence of cues in the environment that are now linked to smoking and lead to urges to smoke (e.g., finishing a meal, seeing someone smoke) or the degree to which smokers feel they have lost control over their smoking. These constructs are typically thought of to be related to addiction but they are included in some dependence assessments. Below are three of the major types of nicotine dependence assessments: physical dependence assessments, clinical assessments, and multidimensional assessments. Each type varies in how nicotine dependence is defined and assessed.
Some measures of nicotine dependence focus on physical dependence, which can be defined as the development of tolerance, which allows someone to smoke more heavily, and the presence of withdrawal symptoms when someone quits. Such measures include the Fagerstrom Test of Nicotine Dependence and the Heaviness of Smoking Index. These well-validated, reliable measures focus on heavy use (smoking a large number of cigarettes per day) and the time to smoking the first cigarette in the morning.[6] Heavy smoking indicates neuroadaptation, or changes in the brain, because smoking a large number of cigarettes per day is only possible if the smoker has developed tolerance to the negative effects of cigarettes (i.e., s/he can smoke more cigarettes over time and not get sick). The time to smoking the first cigarette in the morning is an index of the need for nicotine following an extended, overnight abstinence. This illustrates a neuroadaptive response to the lack of nicotine in the system—if the brain needs more nicotine after going all night without any, then the urge to smoke early in the morning will be especially strong. These measures consider dependence to be a continuous construct such that people can be more or less dependent relative to one another or over time.
The 4th edition of the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorder (DSM-IV) had a Nicotine Dependence diagnosis that went beyond physical dependence to include, “…a cluster of cognitive, behavioral, and physiological symptoms ….”[7] In the updated DSM-V there is no nicotine dependence diagnosis, but rather Tobacco Use Disorder, which is defined as, “A problematic pattern of tobacco use leading to clinically significant impairment or distress, as manifested by at least 2 of the following [11 symptoms], occurring within a 12-month period.”[8] Some of these 11 symptoms include tolerance, withdrawal, craving, inability to quit or cut down, and use despite problems. In other words, the indicators of dependence. These symptoms are consistent with other Substance Use Disorder diagnoses for other drugs. However, it is important to note that for nicotine dependence, it is impaired control or the inability to quit despite the known health risks of tobacco use that is the central feature of this definition. It should also be noted that while a DSM diagnosis is dichotomous, the cut-off of 2 of 11 symptoms is somewhat arbitrary.
Finally, there are multidimensional, continuous dependence assessment scales that focus on the mechanisms of dependence, not just the end products of dependence like heavy smoking and time to first morning cigarette. These assessments include the Nicotine Dependence Syndrome Scale and the Wisconsin Inventory of Smoking Dependence Motives.[6] These measures have subscales that assess physical dependence, such as tolerance and heavy smoking, but also have behavioral and psychological components such as smoking contexts (e.g., being around smokers frequently), the ritualized nature of smoking, and smoking for a specific reason (e.g., to improve mood or concentration). These measures provide insight into what might be termed “psychological” dependence, or the drive to continue smoking based on psychological factors. These multidimensional measures consider nicotine dependence to be a continuous construct.
Epidemiology
There are approximately 976 million smokers in the world.[9] Estimates are that half of smokers (and one-third of former smokers) are dependent based on DSM criteria, regardless of age, gender or country of origin, but this could be higher if different definitions of dependence were used.[10] Recent data suggest that, in the United States, the rates of daily smoking and the number of cigarettes smoked per day are declining, suggesting a reduction in population-wide dependence among current smokers.[11] However, there are different groups of people who are more likely to smoke than the average population, such as those with low education or low socio-economic status and those with mental illness.[11] There is also evidence that among smokers, some subgroups may be more dependent than other groups. Men smoke at higher rates than do women and score higher on dependence indices; however, women may be less likely to be successful in quitting, suggesting that women may be more dependent by that criterion.[11][12] Higher nicotine dependence has also been linked with mental illness, including anxiety and depression.[13][14]
Mechanisms
Traditional cigarettes are the most common delivery device for nicotine. However, electronic cigarettes are becoming more popular. Nicotine can also be delivered via other tobacco products such as chewing tobacco, snus, pipe tobacco, hookah, all of which can produce nicotine dependence. The risk for developing dependence is related to how much nicotine is in a product and how fast it can get to the user’s brain. Smoke from products like cigarettes and hookah is absorbed in the lungs and then nicotine gets to the brain in about 6 seconds. Cigarettes and hookah also have large amounts of nicotine in them, and therefore people who use them have a higher risk of developing dependence. Products where nicotine is absorbed into the blood through the mouth (e.g., snus, chewing tobacco), and therefore takes longer to get to the brain, have lower dependence risk. Nicotine replacement medications like the nicotine patch, nicotine lozenges, and nicotine gum have minimal to no dependence risk because they do not contain nearly as much nicotine as tobacco products and they don’t get into the brain very quickly. This is why nicotine replacement medications are safe.
Biomolecular
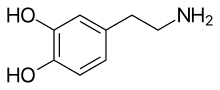
Nicotine binds with nicotinic receptors in the brain and releases a variety of neurotransmitters, including dopamine, which, in turn, produce the pleasurable effects associated with smoking. With repeated exposure to nicotine, the number of binding sites on nicotinic receptors in the brain increases. When these receptors are not occupied by nicotine, they are believed to produce withdrawal symptoms.[15] This upregulation or increase in the number of nicotinic receptors also significantly alters the functioning of the brain reward system.[16] There are genetic risk factors for developing dependence. For instance, genetic markers for a specific type of nicotinic receptor (the α5-α3-β4 nicotine receptors) have been linked to increased risk for dependence.[17][18] In other words, for smokers with a specific genetic code, exposure to nicotine results in an increased risk for neuroadaptation and the development of nicotine dependence.
Psychosocial
In addition to the specific neurological changes in nicotinic receptors, there are other changes that occur as dependence develops. Through various conditioning mechanisms (operant and cue/classical), smoking comes to be associated with different mood and cognitive states as well as external contexts and cues.[16] For instance, the act of repeatedly smoking a cigarette conditions the smoker to expect specific results via operant conditioning. This would include smoking because s/he expects to experience the buzz or high associated with cigarette use (i.e., positive reinforcement) as well as smoking to reduce negative affect or alleviate cravings (i.e., negative reinforcement). In other words, smokers come to rely on smoking to cope with negative moods or to help them feel good and enjoy something even more. This can be especially problematic for smokers who want to quit if they don’t have other ways to cope with negative moods or to enjoy activities. Repeated exposure to nicotine within specific contexts also produces cue conditioning (via classical conditioning), whereby a smoker in a specific context (e.g., after a meal, after an argument, at a certain place in the house) comes to associate that context with smoking. In this case, exposure to a cue, such as seeing someone smoking, could elicit a craving and lead someone to smoke a cigarette. This can become problematic for someone trying to quit because these cues can be everywhere and make it hard to quit by presenting constant reminders of smoking (e.g., a cup of coffee or a party or seeing a particular friend could all be cues to smoke and create urges to smoke).
Treatment
There are effective treatments for nicotine dependence, although the majority of the evidence focuses on treatments for cigarette smokers rather than people who use other forms of tobacco (e.g., chew, snus, pipes, hookah, electronic cigarettes). These treatments have been shown to double or even triple a smoker’s chances of quitting successfully.[5]
Medication
There are eight major evidence-based medications for treating nicotine dependence: bupropion, cytisine (not approved for use in some countries, including the US), nicotine gum, nicotine inhaler, nicotine lozenge/mini-lozenge, nicotine nasal spray, nicotine patch, and varenicline.[19][20] These medications have been shown to significantly improve long-term (i.e., 6-months post-quit day) abstinence rates, especially when used in combination with psychosocial treatment.[5] The nicotine replacement treatments (i.e., patch, lozenge, gum) are dosed based on how dependent a smoker is—people who smoke more cigarettes or who smoke earlier in the morning use higher doses of nicotine replacement treatments.
Psychosocial
Psychosocial interventions delivered in-person (individually or in a group) or over the phone (including mobile phone interventions) have been shown to effectively treat nicotine dependence.[21] These interventions focus on providing support for quitting and helping with smokers with problem-solving and developing healthy responses for coping with cravings, negative moods, and other situations that typically lead to relapse. The combination of pharmacotherapy and psychosocial interventions has been shown to be especially effective.[5]
References
- ↑ Edwards, G; Gross, MM. "Alcohol dependence: provisional description of a clinical syndrome.". BMJ. 1: 1058-1061.
- ↑ Siegel, S (1983). Smart, RG; Glaser, FB; Israel, Y; Kalant, R; Popham, E; Schmidt, W, eds. Research advances in alcohol and drug problems (7th ed.). New York: Plenum.
- ↑ Wikler, A (1980). Opiod dependence. New York: Plenum.
- ↑ U.S. Department of Health and Human Services (1988). The health consequences of smoking: Nicotine addiction: A report of the Surgeon General (PDF). U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health. DHHS Publication No. (CDC) 88-8406.
- 1 2 3 4 Fiore, MC; Jaen, CR; Baker, TB; et al. (2008). Treating tobacco use and dependence: 2008 update (PDF). Rockville, MD: U.S. Department of Health and Human Services, U.S. Public Health Service.
- 1 2 Piper, ME; McCarthy, DE; Baker, TB (2006). "Assessing tobacco dependence: a guide to measure evaluation and selection.". Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 8 (3): 339–51. PMID 16801292.
- ↑ American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (4th ed), DSM-IV. p. 176.
- ↑ American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed), DSM-V. p. 571.
- ↑ Ng, M; Freeman, MK; Fleming, TD; Robinson, M; Dwyer-Lindgren, L; Thomson, B; Wollum, A; Sanman, E; Wulf, S; Lopez, AD; Murray, CJ; Gakidou, E (8 January 2014). "Smoking prevalence and cigarette consumption in 187 countries, 1980-2012.". JAMA. 311 (2): 183–92. PMID 24399557.
- ↑ Hughes, JR; Helzer, JE; Lindberg, SA (8 November 2006). "Prevalence of DSM/ICD-defined nicotine dependence.". Drug and alcohol dependence. 85 (2): 91–102. PMID 16704909.
- 1 2 3 Centers for Disease Control and Prevention (2014). "Current Cigarette Smoking Among Adults — United States, 2005–2013". Morbidity and Mortality Weekly Report (63): 1108–1112.
- ↑ Weinberger, AH; Pilver, CE; Mazure, CM; McKee, SA (September 2014). "Stability of smoking status in the US population: a longitudinal investigation.". Addiction (Abingdon, England). 109 (9): 1541–53. PMID 24916157.
- ↑ Pedersen, W; von Soest, T (January 2009). "Smoking, nicotine dependence and mental health among young adults: a 13-year population-based longitudinal study.". Addiction (Abingdon, England). 104 (1): 129–37. PMID 19133898.
- ↑ Breslau, N; Novak, SP; Kessler, RC (1 January 2004). "Psychiatric disorders and stages of smoking.". Biological psychiatry. 55 (1): 69–76. PMID 14706427.
- ↑ Benowitz, NL (17 June 2010). "Nicotine addiction.". The New England journal of medicine. 362 (24): 2295–303. doi:10.1056/NEJMra0809890. PMID 20554984.
- 1 2 Martin-Soelch, Chantal (15 February 2013). "Neuroadaptive Changes Associated with Smoking: Structural and Functional Neural Changes in Nicotine Dependence". Brain Sciences. 3 (1): 159–176.
- ↑ Saccone, NL; Culverhouse, RC; Schwantes-An, TH; Cannon, DS; Chen, X; Cichon, S; Giegling, I; Han, S; Han, Y; Keskitalo-Vuokko, K; Kong, X; Landi, MT; Ma, JZ; Short, SE; Stephens, SH; Stevens, VL; Sun, L; Wang, Y; Wenzlaff, AS; Aggen, SH; Breslau, N; Broderick, P; Chatterjee, N; Chen, J; Heath, AC; Heliövaara, M; Hoft, NR; Hunter, DJ; Jensen, MK; Martin, NG; Montgomery, GW; Niu, T; Payne, TJ; Peltonen, L; Pergadia, ML; Rice, JP; Sherva, R; Spitz, MR; Sun, J; Wang, JC; Weiss, RB; Wheeler, W; Witt, SH; Yang, BZ; Caporaso, NE; Ehringer, MA; Eisen, T; Gapstur, SM; Gelernter, J; Houlston, R; Kaprio, J; Kendler, KS; Kraft, P; Leppert, MF; Li, MD; Madden, PA; Nöthen, MM; Pillai, S; Rietschel, M; Rujescu, D; Schwartz, A; Amos, CI; Bierut, LJ (5 August 2010). "Multiple independent loci at chromosome 15q25.1 affect smoking quantity: a meta-analysis and comparison with lung cancer and COPD.". PLoS genetics. 6 (8). PMID 20700436.
- ↑ Ware, JJ; van den Bree, MB; Munafò, MR (2011). "Association of the CHRNA5-A3-B4 gene cluster with heaviness of smoking: a meta-analysis.". Nicotine & Tobacco Research. 13 (12): 1167–75. PMID 22071378.
- ↑ Hartmann-Boyce, J; Stead, LF; Cahill, K; Lancaster, T (2013). "Efficacy of interventions to combat tobacco addiction: Cochrane update of 2012 reviews.". Addiction (Abingdon, England). 108 (10): 1711–21. PMID 23834141.
- ↑ Hartmann-Boyce, J; Stead, LF; Cahill, K; Lancaster, T (October 2013). "Efficacy of interventions to combat tobacco addiction: Cochrane update of 2012 reviews.". Addiction (Abingdon, England). 108 (10): 1711–21. PMID 23834141.
- ↑ Hartmann-Boyce, J; Stead, LF; Cahill, K; Lancaster, T (October 2013). "Efficacy of interventions to combat tobacco addiction: Cochrane update of 2012 reviews.". Addiction (Abingdon, England). 108 (10): 1711–21. PMID 23834141.
External links
- Fagerstrom Test of Nicotine Dependence (Heatherton et al., 1991)
- Heaviness of Smoking Index (Heatherton et al., 1989)
- Diagnostic and Stastistical Manual V (DSM-V)
- Tobacco Dependence Screener (Kawakami et al., 1999)
- Nicotine Dependence Syndrome Scale (NDSS; Shiffman, Waters & Hickcox, 2004)
- Cigarette Dependence Scale (Etter et al., 2003)
- Wisconsin Inventory of Smoking Dependence Motives (Piper et al., 2004)]