Narcolepsy
| Narcolepsy | |
|---|---|
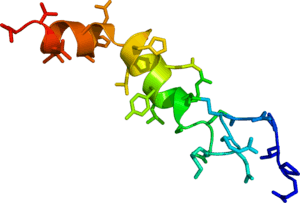 | |
| The neuropeptide orexin-A believed to be reduced in the neurons of people with narcolepsy | |
| Pronunciation | /ˈnɑːrkəˌlɛpsi/ |
| Classification and external resources | |
| Specialty | Sleep medicine |
| ICD-10 | G47.4 |
| ICD-9-CM | 347 |
| OMIM | 161400 |
| DiseasesDB | 8801 |
| MedlinePlus | 000802 |
| eMedicine | neuro/522 |
| MeSH | D009290 |
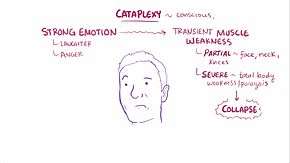
Narcolepsy is a long term neurological disorder that involves a decreased ability to regulate sleep-wake cycles.[1] Symptoms include periods of excessive daytime sleepiness that usually lasts from seconds to minutes and may occur at any time. About 70% also have periods of sudden loss of muscle strength, known as cataplexy. These spells can be brought on by strong emotions. Less commonly there may be vivid dream like images or the inability to move for a period of time during falling asleep or upon waking-up. People with narcolepsy sleep about the same amount of hours per day as people without but the quality of sleep tends to be worse.[1]
The cause of narcolepsy is unknown.[2] In up to 10% of cases there is a family history of the disorder. Often those affected have low levels of the neurotransmitter hypocretin which may be due to an autoimmune disorder. Trauma, certain infections, toxins, or psychological stress may also play a role. Diagnosis is typically based on the symptoms and sleep studies, after ruling out other potential causes. Excessive daytime sleepiness can also be caused by other sleep disorders such as sleep apnea, major depressive disorder, anemia, heart failure, drinking alcohol, and not getting enough sleep. Cataplexy may be mistaken for seizures.[1]
While there is no cure, a number of lifestyle changes and medications may help. Lifestyle changes include taking regular short naps and sleep hygiene. Medications used include modafinil, sodium oxybate, and methylphenidate. While initially fairly effective, tolerance to the benefits may develop. Tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) may improve cataplexy.[1]
About 0.2 to 600 per 100,000 people are affected.[3] The condition often begins in childhood. Men and women are affected equally. Untreated narcolepsy increases the risk of motor vehicle collisions and falls.[1] The term narcolepsy is from the French narcolepsie. The French term was first used in 1880 by Jean-Baptiste-Édouard Gélineau who used the Greek νάρκη (narkē) meaning "numbness" and λῆψις (lepsis) meaning "attack".[4]
Signs and symptoms
There are two main characteristics of narcolepsy: excessive daytime sleepiness and abnormal REM sleep.[5] The first, excessive daytime sleepiness (EDS), occurs even after adequate night time sleep. A person with narcolepsy is likely to become drowsy or fall asleep, often at inappropriate times and places, or just be very tired throughout the day. Narcoleptics are not able to experience the amount of restorative deep sleep that healthy people experience – they are not "over-sleeping". In fact, narcoleptics live their entire lives in a constant state of extreme sleep deprivation. Daytime naps may occur with little warning and may be physically irresistible. These naps can occur several times a day. They are typically refreshing, but only for a few hours or less. Vivid dreams may be experienced on a constant or regular basis, even during very brief naps. Drowsiness may persist for prolonged periods of time or simply never cease. In addition, night-time sleep may be fragmented with frequent awakenings. A second prominent symptom of narcolepsy is abnormal REM sleep. Narcoleptics are unique in that they enter into the REM phase of sleep in the beginnings of sleep, even when sleeping during the day.[5]
The classic symptoms of the disorder, often referred to as the "tetrad of narcolepsy," are cataplexy, sleep paralysis, hypnagogic hallucinations, and excessive daytime sleepiness.[6] Other symptoms may include automatic behaviors and night-time wakefulness.[7][8][9] These symptoms may not occur in all patients.
- Cataplexy is episodic loss of muscle function, ranging from slight weakness such as limpness at the neck or knees, sagging facial muscles, weakness at the knees often referred to as "knee buckling",[10] or inability to speak clearly, to a complete body collapse. Episodes may be triggered by sudden emotional reactions such as laughter, anger, surprise, or fear, and may last from a few seconds to several minutes. The person remains conscious throughout the episode. In some cases, cataplexy may resemble epileptic seizures. Usually speech is slurred and vision is impaired (double vision, inability to focus), but hearing and awareness remain normal. Cataplexy also has a severe emotional impact on narcoleptics, as it can cause extreme anxiety, fear, and avoidance of people or situations that might elicit an attack. Cataplexy is generally considered to be unique to narcolepsy and is analogous to sleep paralysis in that the usually protective paralysis mechanism occurring during sleep is inappropriately activated. The opposite of this situation (failure to activate this protective paralysis) occurs in rapid eye movement behavior disorder.
- Periods of wakefulness at night[5]
- Sleep paralysis is the temporary inability to talk or move when waking (or less often, when falling asleep). It may last a few seconds to minutes. This is often frightening but is not dangerous.
- Hypnagogic hallucinations are vivid, often frightening, dreamlike experiences that occur while dozing or falling asleep. Hypnopompic hallucinations refer to the same sensations while awakening from sleep. These hallucinations may manifest in the form of visual or auditory sensations.[5]
- Automatic behaviors occur when a person continues to function (talking, putting things away, etc.) during sleep episodes, but awakens with no memory of performing such activities. It is estimated that up to 40 percent of people with narcolepsy experience automatic behavior during sleep episodes.
In most cases, the first symptom of narcolepsy to appear is excessive and overwhelming daytime sleepiness. The other symptoms may begin alone or in combination months or years after the onset of the daytime naps. There are wide variations in the development, severity, and order of appearance of cataplexy, sleep paralysis, and hypnagogic hallucinations in individuals. Only about 20 to 25 percent of people with narcolepsy experience all four symptoms. The excessive daytime sleepiness generally persists throughout life, but sleep paralysis and hypnagogic hallucinations may not. A rare subset of narcoleptics also experience a heightened sense of taste and smell known as the supertaster phenomenon.
Many people with narcolepsy also suffer from insomnia for extended periods of time. The excessive daytime sleepiness and cataplexy often become severe enough to cause serious problems in a person's social, personal, and professional life. Normally, when an individual is awake, brain waves show a regular rhythm. When a person first falls asleep, the brain waves become slower and less regular, which is called non-rapid eye movement (NREM) sleep. After about an hour and a half of NREM sleep, the brain waves begin to show a more active pattern again, called REM sleep (rapid eye movement sleep), when most remembered dreaming occurs. Associated with the EEG-observed waves during REM sleep, muscle atonia is present called REM atonia.
In narcolepsy, the order and length of NREM and REM sleep periods are disturbed, with REM sleep occurring at sleep onset instead of after a period of NREM sleep. Also, some aspects of REM sleep that normally occur only during sleep, like lack of muscular control, sleep paralysis, and vivid dreams, occur at other times in people with narcolepsy. For example, the lack of muscular control can occur during wakefulness in a cataplexy episode; it is said that there is intrusion of REM atonia during wakefulness. Sleep paralysis and vivid dreams can occur while falling asleep or waking up. Simply put, the brain does not pass through the normal stages of dozing and deep sleep but goes directly into (and out of) rapid eye movement (REM) sleep.
As a consequence night time sleep does not include as much deep sleep, so the brain tries to "catch up" during the day, hence EDS. People with narcolepsy may visibly fall asleep at unpredicted moments (such motions as head bobbing are common). People with narcolepsy fall quickly into what appears to be very deep sleep, and they wake up suddenly and can be disoriented when they do (dizziness is a common occurrence). They have very vivid dreams, which they often remember in great detail. People with narcolepsy may dream even when they only fall asleep for a few seconds. Along with vivid dreaming, people with narcolepsy are known to have audio or visual hallucinations prior to falling asleep.
Narcoleptics can gain excess weight; children can gain 20 to 40 lb (9 to 18 kg) when they first develop narcolepsy; in adults the body-mass index is about 15% above average.[11][12]
Causes
Although the cause of narcolepsy was not determined for many years after its discovery, scientists had discovered conditions that seemed to be associated with an increase in an individual's risk of having the disorder. Specifically, there appeared to be a strong link between individuals with narcolepsy and certain genetic conditions. One factor that seemed to predispose an individual to narcolepsy involved an area of Chromosome 6 known as the HLA complex.[13] There appeared to be a correlation between individuals with narcolepsy and certain variations in HLA genes, although it was not required for the condition to occur. Certain variations in the HLA complex were thought to increase the risk of an auto-immune response to protein-producing neurons in the brain. The protein produced, called hypocretin or orexin, is responsible for controlling appetite and sleep patterns.[14] Of the billions of cells in the human brain, only about 10,000 to 20,000 cells secrete hypocretin molecules.[5] Low levels of hypocretin have been correlated with a past history of infection, diet, contact with toxins such as pesticides, and brain injuries due to brain tumors or strokes.[5]
Individuals with narcolepsy often have reduced numbers of these protein-producing neurons in their brains.[14] In 2009 the autoimmune hypothesis was supported by research carried out at Stanford University School of Medicine.[15][16]
The neural control of normal sleep states and the relationship to narcolepsy are only partially understood. In humans, narcoleptic sleep is characterized by a tendency to go abruptly from a waking state to REM sleep with little or no intervening non-REM sleep. The changes in the motor and proprioceptive systems during REM sleep have been studied in both human and animal models. During normal REM sleep, spinal and brainstem alpha motor neuron hyperpolarization produces almost complete atonia of skeletal muscles via an inhibitory descending reticulospinal pathway. Acetylcholine may be one of the neurotransmitters involved in this pathway. In narcolepsy, the reflex inhibition of the motor system seen in cataplexy has features normally seen only in normal REM sleep.[17]
In 2004 researchers in Australia induced narcolepsy-like symptoms in mice by injecting them with antibodies from narcoleptic humans. The research has been published in the Lancet providing strong evidence suggesting that some cases of narcolepsy might be caused by autoimmune disease.[18] Narcolepsy is strongly associated with HLA-DQB1*0602 genotype.[19] There is also an association with HLA-DR2 and HLA-DQ1. This may represent linkage disequilibrium. Despite the experimental evidence in human narcolepsy that there may be an inherited basis for at least some forms of narcolepsy, the mode of inheritance remains unknown. Some cases are associated with genetic diseases such as Niemann-Pick disease[20] or Prader-Willi syndrome.[21]
In December 2013, a study was published providing evidence that autoimmune CD4+ T-cells against HRCT epitopes may be a causative factor of the disease, as well as reinforcing the association with the influenza H1N1 vaccine; however, this study was retracted by the authors in July 2014.[22][23]
A retrospective study of several hundred people in China reported that narcolepsy onset is highly correlated with seasonal patterns of upper airway infections, including H1N1 influenza.[24]
Genetics
The allele HLA-DQB1*06:02 of the human gene HLA-DQB1 was reported in more than 90% of patients, and alleles of other HLA genes such as HLA-DQA1*01:02 have been linked. A 2009 study found a strong association with polymorphisms in the TRAC gene locus (dbSNP IDs rs1154155, rs12587781, and rs1263646).[25] A 2013 review article reported additional but weaker links to the loci of the genes TNFSF4 (rs7553711), Cathepsin H (rs34593439), and P2RY11-DNMT1 (rs2305795).[26] Another gene locus that has been associated with narcolepsy is EIF3G (rs3826784).[27]
Evolution
Narcolepsy may represent an evolutionary atavism. According to a hypothesis REM sleep is an evolutionary transformation of a well-known defensive mechanism, the tonic immobility reflex.[28][29] This reflex, also known as animal hypnosis or death feigning, functions as the last line of defense against an attacking predator and consists of the total immobilization of the animal: the animal appears dead (cf. "playing possum"). The neurophysiology and phenomenology of this reaction shows striking similarities to REM sleep, a fact which betrays a potential evolutionary kinship. For example, both reactions exhibit brainstem control, paralysis, sympathetic activation, and thermoregulatory changes. This hypothesis, which integrates many research findings into a unified and evolutionarily well informed framework, also sheds light on the phenomenon of narcolepsy.[28]
Vaccine
A link between GlaxoSmithKline's H1N1 flu vaccine Pandemrix and childhood narcolepsy was investigated due to increased prevalence of narcolepsy in Irish, Finnish and Swedish children after vaccinations. Finland's National Institute of Health and Welfare recommended that Pandemrix vaccinations be suspended pending further investigation into 15 reported cases of children developing narcolepsy.[30][31] In Finland in mid-November 2010, 37 cases of children's narcolepsy had been reported by doctors. This can be compared to the normal average of 3 cases of children's narcolepsy per year.[32] "The incidence of narcolepsy with cataplexy in children/adolescents in the Swedish population increased during the pandemic and vaccination period, with a rapid decline in incidence during the post pandemic period." They concluded that these results "provide strengthened evidence that vaccination with Pandemrix during the pandemic period could be associated with an increase in the risk for narcolepsy with cataplexy in predisposed children/adolescents 19 years and younger."[33] In 2013, the link between Pandemrix and narcolepsy was confirmed by a registry study by the Swedish Medical Products Agency, with a three-fold increase in risk for people under the age of 20.[34]
Diagnosis
Diagnosis is relatively easy when all the symptoms of narcolepsy are present, but if the sleep attacks are isolated and cataplexy is mild or absent, diagnosis is more difficult. It is also possible for cataplexy to occur in isolation. Three tests that are commonly used in diagnosing narcolepsy are the polysomnogram, the multiple sleep latency test (MSLT), and administration of the Epworth Sleepiness Scale. These tests are usually performed by a sleep specialist. The polysomnogram involves continuous recording of sleep brain waves and a number of nerve and muscle functions during nighttime sleep. When tested, people with narcolepsy fall asleep rapidly, enter REM sleep early, and may often awaken during the night. The polysomnogram also helps to detect other possible sleep disorders that could cause daytime sleepiness.
The Epworth Sleepiness Scale is a brief questionnaire that is administered to determine the likelihood of the presence of a sleep disorder, including narcolepsy. For the multiple sleep latency test, a person is given a chance to sleep every 2 hours during normal wake times. The patient is taken in usually for an overnight sleep study. The following day the patient will have multiple tests where they will be told to nap after a full nights sleep (usually eight hours). Observations are made of the time taken to reach various stages of sleep (sleep onset latency). This test measures the degree of daytime sleepiness and also detects how soon REM sleep begins. Again, people with narcolepsy fall asleep rapidly and enter REM sleep early. Occasionally, a multiple sleep latency test can result in a false-negative for a narcoleptic.[35]
The system which regulates sleep, arousal, and transitions between these states in humans is composed of three interconnected subsystems: the orexin projections from the lateral hypothalamus, the reticular activating system, and the ventrolateral preoptic nucleus.[36] In narcoleptic individuals, these systems are all associated with impairments due to a greatly reduced number of hypothalamic orexin projection neurons and significantly fewer orexin neuropeptides in cerebrospinal fluid and neural tissue, compared to non-narcoleptic individuals.[36] Those with narcolepsy generally experience the REM stage of sleep within five minutes of falling asleep, while people who do not have narcolepsy (unless they are significantly sleep deprived)[37] do not experience REM until after a period of slow-wave sleep, which lasts for about the first hour or so of a sleep cycle.[17]
Measuring hypocretin levels in a person's cerebrospinal fluid sampled in a spinal tap may help in diagnosing narcolepsy,[38] with abnormally low levels serving as an indicator of the disorder. This test can be useful when MSLT results are inconclusive or difficult to interpret.[39]
Classification
The 2001 International Classification of Sleep Disorders (ICSD) divides primary hypersomnia syndromes between narcolepsy, idiopathic hypersomnia, and the recurrent hypersomnias (like Klein-Levin syndrome); it further divides narcolepsy into that with cataplexy and that without cataplexy.[40] This ICSD version defines narcolepsy as “a disorder of unknown etiology that is characterized by excessive sleepiness that typically is associated with cataplexy and other REM-sleep phenomena, such as sleep paralysis and hypnagogic hallucinations". It also establishes baseline categorical standards for diagnosis of narcolepsy, through 2 sets of well defined criteria, as follows.[41] Minimal narcolepsy diagnostic criteria set #2:
- A "complaint of excessive sleepiness or sudden muscle weakness."
- Associated features that include: sleep paralysis; disrupted major sleep episode; hypnagogic hallucinations; automatic behaviors.
- Polysomnography with one or more of the following: "sleep latency less than 10 minutes;" "REM sleep latency less than 20 minutes;" an MSLT with a mean sleep latency less than 5 minutes; "two or more sleep-onset REM periods" (SOREMPs).
- "No medical or mental disorder accounts for the symptoms." (see hypersomnia differential diagnosis)[41]
In the absence of clear cataplexy, it becomes much more difficult to make a firm diagnosis of narcolepsy. “Various terms, such as essential hypersomnia, primary hypersomnia, ambiguous narcolepsy, atypical narcolepsy, etc., have been used to classify these patients, who may be in the developing phase of narcolepsy.” [41]
Since the 2001 ICSD, the classification of primary hypersomnias has been steadily evolving, as further research has shown more overlap between narcolepsy and idiopathic hypersomnia.[42] The 3rd edition of the ICSD is currently being finalized, and its new classification will label narcolepsy caused by hypocretin deficiency as “type 1 narcolepsy,” which is almost always associated with cataplexy. The other primary hypersomnias will remain subdivided based on the presence of SOREMPs. They will be labeled: “type 2 narcolepsy,” with 2 or more SOREMPs on MSLT; and “idiopathic hypersomnia,” with less than 2 SOREMPS.[43]
However, “there is no evidence that the pathophysiology or therapeutic response is substantially different for hypersomnia with or without SOREMPs on the MSLT.”[43] Given this currently understood overlap of idiopathic hypersomnia and narcolepsy, the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) is also updating its classification of the primary hypersomnias. It reclassifies narcolepsy without cataplexy as major somnolence disorder (MSD). Additionally, MSD will encompass all syndromes of hypersomnolence not explained by low hypocretin, including idiopathic hypersomnia (with and without long sleep time) and long sleepers (patients requiring >10 hours sleep/day).[43][44][45]
Further complicating these updated classification schemes, overlap between narcolepsy with cataplexy and idiopathic hypersomnia has also been reported. A subgroup of narcoleptics with long sleep time, comprising 18% of narcoleptics in one study, had symptoms of both narcolepsy with cataplexy and idiopathic hypersomnia (long sleep time and unrefreshing naps). It is felt that this subgroup might have dysfunction in multiple arousal systems, including hypocretin and GABA (see idiopathic hypersomnia causes).[46]
Treatment
People with narcolepsy can be substantially helped, but not cured.[47] Treatment is tailored to the individual, based on symptoms and therapeutic response. The time required to achieve optimal control of symptoms is highly variable, and may take several months or longer. Medication adjustments are frequently necessary, and complete control of symptoms is seldom possible. While oral medications are the mainstay of formal narcolepsy treatment, lifestyle changes are also important.
The main treatment of excessive daytime sleepiness in narcolepsy is central nervous system stimulants such as methylphenidate, amphetamine, dextroamphetamine, modafinil, and armodafinil. In late 2007 an alert for severe adverse skin reactions to modafinil was issued by the FDA.[48]
Another drug that is used is atomoxetine,[49] a non-stimulant and norepinephrine reuptake inhibitor (NRI), that has no addiction liability or recreational effects. In many cases, planned regular short naps can reduce the need for pharmacological treatment of the EDS, but only improve symptoms for a short duration. A 120 minute nap provided benefit for 3 hours in patient alertness whereas a 15 minute nap provided no benefit.[50] Daytime naps are not a replacement for nighttime sleep. Ongoing communication between the health care provider, patient, and the patient's family members is important for optimal management of narcolepsy.
Another FDA-approved treatment option for narcolepsy is sodium oxybate,[51] also known as sodium gamma-hydroxybutyrate (GHB). It can be used for cataplexy associated with narcolepsy and excessive daytime sleepiness associated with narcolepsy.[51][52][53][54]
Narcolepsy has sometimes been treated with selective serotonin reuptake inhibitors and tricyclic antidepressants, such as clomipramine, imipramine, or protriptyline, as well as other drugs that suppress REM sleep.[55] Venlafaxine, an antidepressant which blocks the reuptake of serotonin and norepinephrine, has shown usefulness in managing symptoms of cataplexy,[56] however, it has notable side-effects including sleep disruption.[57]
Epidemiology
In the United States, it is estimated that this condition afflicts as many as 200,000 Americans,[58] but fewer than 50,000 are diagnosed. It is as widespread as Parkinson's disease or multiple sclerosis and more prevalent than cystic fibrosis, but it is less well known. Narcolepsy is often mistaken for depression, epilepsy, or the side effects of medications. It can also be mistaken for poor sleeping habits, recreational drug use, or laziness. Narcolepsy can occur in both men and women at any age, although its symptoms are usually first noticed in teenagers or young adults. There is strong evidence that narcolepsy may run in families; around 10 percent of people diagnosed with narcolepsy with cataplexy have a close relative with this neurological disorder.[17] While narcolepsy symptoms are often confused with depression, there is a link between the two disorders. Research studies have mixed results on co-occurrence of depression in narcolepsy patients - the numbers quoted by different studies are anywhere between 6% and 50%.[59]
Narcolepsy has its typical onset in adolescence and young adulthood. There is an average 15-year delay between onset and correct diagnosis which may contribute substantially to the disabling features of the disorder. Cognitive, educational, occupational, and psychosocial problems associated with the excessive daytime sleepiness of narcolepsy have been documented. For these to occur in the crucial teen years when education, development of self-image, and development of occupational choice are taking place is especially devastating. While cognitive impairment does occur, it may only be a reflection of the excessive daytime somnolence.
The prevalence of narcolepsy is about 1 per 2,000 persons.[58] It is a reason for patient visits to sleep disorder centers, and with its onset in adolescence, it is also a major cause of learning difficulty and absenteeism from school. Normal teenagers often already experience excessive daytime sleepiness because of a maturational increase in physiological sleep tendency accentuated by multiple educational and social pressures; this may be disabling with the addition of narcolepsy symptoms in susceptible teenagers. In clinical practice, the differentiation between narcolepsy and other conditions characterized by excessive somnolence may be difficult. Treatment options are currently limited. There is a paucity in the literature of controlled double-blind studies of possible effective drugs or other forms of therapy. Mechanisms of action of some few available therapeutic agents have been explored but detailed studies of mechanisms of action are needed before new classes of therapeutic agents can be developed. Narcolepsy is an underdiagnosed condition in the general population. This is partly because its severity varies, so it can be mistaken for other illnesses very easily. Some people with narcolepsy do not suffer from loss of muscle control.
Society and culture
In the British television comedy-drama Doc Martin, the character Joe Penhale (played by John Marquez) is portrayed as having narcolepsy.[60] In the 2007 video game Little Busters!, the protagonist Riki Naoe suffers from narcolepsy. In the 2001 film Rat Race, Enrico Pollini, played by Rowan Atkinson, suffers from narcolepsy, which is used to comic effect several times. In the 2014 Tamil movie Naan Sigappu Manithan (directed by Thiru) the lead character, played by Vishal, suffers from narcolepsy.[61] In the season four episode of the 2010 television series Rizzoli & Isles, "Judge, Jury and Executioner", the murder victim Judge Kathleen Harper (played by A'da Alison Woolfolk) suffers from narcolepsy, and uses the drug methylphenidate. This drug is later used to kill her through an overdose.[62]
In 2015, it was reported that the British Department of Health was paying for sodium oxybate medication for 80 people who are taking legal action over problems linked to the use of the Pandemrix swine flu vaccine at a cost of £12,000 a year. Sodium oxybate is not available to people with narcolepsy through the National Health Service.[63]
Research
Histamine-directed medications
"Based on the role of histamine in keeping people awake (and hence the common side effect of anti-histamines such as diphenhydramine causing sleepiness), medications that act on histamine are under development for the treatment of excessive sleepiness."[64] It remains to be seen whether these H3 antagonists (i.e., compounds such as pitolisant that promote the release of the wake-promoting amine histamine) will be particularly useful as wake-promoting agents.[43]
GABA-directed medications
Given the possible role of hyper-active GABAA receptors in the primary hypersomnias (narcolepsy and idiopathic hypersomnia), medications that could counteract this activity are being studied to test their potential to improve sleepiness. These currently include clarithromycin and flumazenil.[65][66]
Flumazenil
Flumazenil is the only GABAA receptor antagonist on the market as of Jan 2013, and it is currently manufactured only as an intravenous formulation. Given its pharmacology, researchers consider it to be a promising medication in the treatment of primary hypersomnias. Results of a small, double-blind, randomized, controlled clinical trial were published in November 2012. This research showed that flumazenil provides relief for most patients whose CSF contains the unknown "somnogen" that enhances the function of GABAA receptors, making them more susceptible to the sleep-inducing effect of GABA. For one patient, daily administration of flumazenil by sublingual lozenge and topical cream has proven effective for several years.[65][67] A 2014 case report also showed improvement in primary hypersomnia symptoms after treatment with a continuous subcutaneous flumazenil infusion.[68] The supply of generic flumazenil was initially thought to be too low to meet the potential demand for treatment of primary hypersomnias.[69] However, this scarcity has eased, and dozens of patients are now being treated with flumazenil off-label.[70]
Clarithromycin
In a test tube model, clarithromycin (an antibiotic approved by the FDA for the treatment of infections) was found to return the function of the GABA system to normal in patients with primary hypersomnias. Investigators therefore treated a few patients with off-label clarithromycin, and most felt their symptoms improved with this treatment. In order to help further determine whether clarithromycin is truly beneficial for the treatment of narcolepsy and idiopathic hypersomnia, a small, double-blind, randomized, controlled clinical trial was completed in 2012.[66] "In this pilot study, clarithromycin improved subjective sleepiness in GABA-related hypersomnia. Larger trials of longer duration are warranted."[71] In 2013, a retrospective review evaluating longer-term clarithromycin use showed efficacy in a large percentage of patients with GABA-related hypersomnia.[72] “It is important to note that the positive effect of clarithromycin is secondary to a benzodiazepine antagonist-like effect, not its antibiotic effects, and treatment must be maintained.”[43]
Hypocretin agonists
Hypocretin-1 (also called orexin) has been shown to be strongly wake-promoting in animal models, but it unfortunately does not cross the blood brain barrier. Therefore, companies have developed hypocretin receptor antagonists, like suvorexant, for the treatment of insomnia. It is also likely that a hypocretin-1 agonist will be found and developed for the treatment of hypersomnia.[43]
L-carnitine
Abnormally low levels of acylcarnitine have been observed in people with narcolepsy.[73] These same low levels have been associated with primary hypersomnia in general in mouse studies. “Mice with systemic carnitine deficiency exhibit a higher frequency of fragmented wakefulness and rapid eye movement (REM) sleep, and reduced locomotor activity.” Administration of acetyl-L-carnitine was shown to improve these symptoms in mice.[74] A subsequent human trial found that narcolepsy patients given L-carnitine spent less total time in daytime sleep than patients who were given placebo.[75]
References
- 1 2 3 4 5 "Narcolepsy Fact Sheet". NINDS. April 6, 2016. Retrieved 19 August 2016.
- ↑ "NINDS Narcolepsy Information Page". NINDS. April 6, 2016. Retrieved 19 August 2016.
- ↑ Goswami, Meeta; Thorpy, Michael J.; Pandi-Perumal, S. R. (2016). Narcolepsy: A Clinical Guide (2 ed.). Springer. p. 39. ISBN 9783319237398.
- ↑ Harper, Douglas (2010). "Narcolepsy". Dictionary.com. Online Etymology Dictionary. Retrieved 19 August 2016.
- 1 2 3 4 5 6 Green, Simon (February 2011). Biological rhythms, sleep, and hypnosis. Basingstoke, Hampshire, England: Palgrave Macmillan. ISBN 9780230252653.
- ↑ Kandel, Eric R.; James H. Schwartz, Thomas M. Jessell. Principles of Neural Science (4th ed.). McGraw-Hill. p. 949. ISBN 0-8385-7701-6.
- ↑ Cunha, John P. Shiel, Jr., William C., ed. "Narcolepsy". MedicineNet. Retrieved 15 March 2016.
- ↑ Zorick FJ, Salis PJ, Roth T, Kramer M; Salis; Roth; Kramer (1979). "Narcolepsy and automatic behavior: A case report". The Journal of Clinical Psychiatry. 40 (4): 194–7. PMID 422531.
- ↑ Green, Simon. Biological rhythms, sleep, and hypnosis. Basingstoke, Hampshire, England: Palgrave Macmillan, 2011. Print.
- ↑ "Stanford: Narcolepsy Symptoms". med.stanford.edu. Retrieved 24 May 2012.
- ↑ Scammell Thomas E (2015). "Narcolepsy". N Engl J Med. 373: 2654–2662. doi:10.1056/NEJMra1500587.
- ↑ Nevsimalova, Sona (2014). "The Diagnosis and Treatment of Pediatric Narcolepsy". Current Neurology and Neuroscience Reports. 14 (8). doi:10.1007/s11910-014-0469-1. ISSN 1528-4042.
- ↑ Klein J, Sato A; Sato (September 2000). "The HLA system. Second of two parts". N. Engl. J. Med. 343 (11): 782–6. doi:10.1056/NEJM200009143431106. PMID 10984567.
- 1 2 Mignot E (2001). "A commentary on the neurobiology of the hypocretin/orexin system". Neuropsychopharmacology. 25 (5 Suppl): S5–13. doi:10.1016/S0893-133X(01)00316-5. PMID 11682267.
- ↑ Hallmayer J, Faraco J, Lin L, Hesselson S, Winkelmann J, Kawashima M, Mayer G, Plazzi G, Nevsimalova S, Bourgin P, Hong SC, Hong SS, Honda Y, Honda M, Högl B, Longstreth WT, Montplaisir J, Kemlink D, Einen M, Chen J, Musone SL, Akana M, Miyagawa T, Duan J, Desautels A, Erhardt C, Hesla PE, Poli F, Frauscher B, Jeong JH, Lee SP, Ton TG, Kvale M, Kolesar L, Dobrovolná M, Nepom GT, Salomon D, Wichmann HE, Rouleau GA, Gieger C, Levinson DF, Gejman PV, Meitinger T, Young T, Peppard P, Tokunaga K, Kwok PY, Risch N, Mignot E; Faraco; Lin; Hesselson; Winkelmann; Kawashima; Mayer; Plazzi; Nevsimalova; Bourgin; Hong; Honda; Honda; Högl; Longstreth Jr; Montplaisir; Kemlink; Einen; Chen; Musone; Akana; Miyagawa; Duan; Desautels; Erhardt; Hesla; Poli; Frauscher; Jeong; et al. (June 2009). "Narcolepsy is strongly associated with the TCR alpha locus". Nat. Genet. 41 (6): 708–11. doi:10.1038/ng.372. PMC 2803042
 . PMID 19412176.
. PMID 19412176. - ↑ "Narcolepsy is an autoimmune disorder, Stanford researcher says". EurekAlert!. American Association for the Advancement of Science. 3 May 2009. Retrieved 31 May 2009.
- 1 2 3 "Narcolepsy Fact Sheet - NIH Publication No. 03-1637". National Institute of Neurological Disorders and Stroke. National Institutes of Health. Retrieved 5 August 2010.
- ↑ "BBC News article". 13 December 2004. Retrieved 6 January 2010.
- ↑ Maret S, Tafti M; Tafti (November 2005). "Genetics of narcolepsy and other major sleep disorders" (PDF). Swiss Medical Weekly. EMH Swiss Medical Publishers Ltd. 135 (45–46): 662–5. PMID 16453205. Retrieved 7 March 2008.
- ↑ Vankova J, Stepanova I, Jech R, Elleder M, Ling L, Mignot E, Nishino S, Nevsimalova S; Stepanova; Jech; Elleder; Ling; Mignot; Nishino; Nevsimalova (June 2003). "Sleep disturbances and hypocretin deficiency in Niemann-Pick disease type C". Sleep. 26 (4): 427–30. PMID 12841368.
- ↑ Manni, R; Politini, L; Nobili, L; Ferrillo, F; Livieri, C; Veneselli, E; Biancheri, R; Martinetti, M; Tartara, A (May 2001). "Hypersomnia in the Prader Willi syndrome: clinical-electrophysiological features and underlying factors". Clin Neurophysiol. 112 (5): 800–5. doi:10.1016/S1388-2457(01)00483-7. PMID 11336895.
- ↑ Kugelberg, Elisabeth (21 January 2014). "Autoimmunity: A new clue to sleepiness". Nature Reviews Immunology. 14 (2): 66–67. doi:10.1038/nri3609.
- ↑ De la Herrán-Arita AK, Kornum BR, Mahlios J, Jiang W, Lin L, Hou T, Macaubas C, Einen M, Plazzi G, Crowe C, Newell EW, Davis MM, Mellins ED, Mignot E; Kornum; Mahlios; Jiang; Lin; Hou; MacAubas; Einen; Plazzi; Crowe; Newell; Davis; Mellins; Mignot (2013). "CD4+ T cell autoimmunity to hypocretin/orexin and cross-reactivity to a 2009 H1N1 influenza A epitope in narcolepsy". Sci Transl Med. 5 (216): 216ra176. doi:10.1126/scitranslmed.3007762. PMID 24353159.
- ↑ Wood H (2011). "In brief". Nature Reviews Neurology. 7 (10): 537. doi:10.1038/nrneurol.2011.143. PMID 21984118.
- ↑ Hallmayer, Joachim; et al. (3 May 2009). "Narcolepsy is strongly associated with the T-cell receptor alpha locus". Nature Genetics. 41 (6): 708–711. doi:10.1038/ng.372. PMC 2803042
 . PMID 19412176.
. PMID 19412176. - ↑ Singh, A. K.; Mahlios, J; Mignot, E (Jun 2013). "Genetic association, seasonal infections and autoimmune basis of narcolepsy". J Autoimmun. 43: 26–31. doi:10.1016/j.jaut.2013.02.003. PMC 4118764
 . PMID 23497937.
. PMID 23497937. - ↑ Holm, Anja; Lin, Ling; Faraco, Juliette; Mostafavi, Sara; Battle, Alexis; Zhu, Xiaowei; Levinson, Douglas F; Han, Fang; Gammeltoft, Steen; Jennum, Poul; Mignot, Emmanuel; Kornum, Birgitte R (11 February 2015). "EIF3G is associated with narcolepsy across ethnicities". European Journal of Human Genetics. 23 (11): 1573–1580. doi:10.1038/ejhg.2015.4.
- 1 2 Tsoukalas I (2012). "The origin of REM sleep: A hypothesis.". Dreaming. 22 (4): 253–283. doi:10.1037/a0030790.
- ↑ Vitelli, R. (2013). Exploring the Mystery of REM Sleep. Psychology Today, On-line blog, 25 March
- ↑ "The MPA investigates reports of narcolepsy in patients vaccinated with Pandemrix". Swedish Medical Products Agency. 18 August 2010. Retrieved 19 August 2010.
- ↑ "Terveyden ja hyvinvoinnin laitos suosittaa Pandemrix-rokotusten keskeyttämistä". National Institute of Health and Welfare. 24 August 2010. Retrieved 24 August 2010.
- ↑ "Ties Between Big Pharma and THL Draw Complaints". Yle Uutiset. 17 November 2010. Retrieved 15 March 2016.
- ↑ "Occurrence of narcolepsy with cataplexy among children and adolescents in relation to the H1N1 pandemic and Pandemrix vaccinations: Results of a case inventory study by the MPA in Sweden during 2009‐2010" (PDF). Läkemedelsverket Medical Products Agency. 30 June 2011. pp. 1, 10. Retrieved 15 March 2016.
- ↑ "Registry study confirms increased risk of narcolepsy after vaccination with Pandemrix in children and adolescents and shows an increased risk in young adults". Läkemedelsverket Medical Products Agency. 26 March 2013. Retrieved 15 March 2016.
- ↑ Thorpy MJ (1992). "The clinical use of the Multiple Sleep Latency Test. The Standards of Practice Committee of the American Sleep Disorders Association". Sleep. 15 (3): 268–76. PMID 1621030.
- 1 2 Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 12: Sleep and Arousal". In Sydor A, Brown RY. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 294–296, 303. ISBN 9780071481274.
the loss of orexin neurons raise the interesting possibility that narcolepsy may be caused by an autoimmune mediated destruction of these neurons in analogy with the autoimmune destruction of insulin-secreting β-islet cells in type I diabetes.
- ↑ "REM sleep deprivation during 5 hours leads to an immediate REM sleep rebound and to suppression of non-REM sleep intensity". Electroencephalogr Clin Neurophysiol. 1990 Aug;76(2):114-22. National Institutes of Health. 76: 114–22. Aug 1990. doi:10.1016/0013-4694(90)90209-3. PMID 1697239. Retrieved 6 June 2014.
- ↑ "Narcolepsy Research - FAQs". psychiatry.stanford.edu. Retrieved 13 September 2012.
- ↑ Mignot E, Lammers GJ, Ripley B, Okun M, Nevsimalova S, Overeem S, Vankova J, Black J, Harsh J, Bassetti C, Schrader H, Nishino S; Lammers; Ripley; Okun; Nevsimalova; Overeem; Vankova; Black; Harsh; Bassetti; Schrader; Nishino (2002). "The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias". Archives of Neurology. 59 (10): 1553–1562. doi:10.1001/archneur.59.10.1553. PMID 12374492.
- ↑ "About Hypersomnia". Hypersomnia Foundation. Retrieved 25 January 2013.
- 1 2 3 "International classification of sleep disorders, revised: Diagnostic and coding manual" (PDF). American Academy of Sleep Medicine. 2001. Retrieved 25 January 2013.
- ↑ Bassetti, C (1997). "Idiopathic hypersomnia A series of 42 patients". Brain. 120 (8): 1423–1435. doi:10.1093/brain/120.8.1423.
- 1 2 3 4 5 6 Mignot EJ (2012). "A Practical Guide to the Therapy of Narcolepsy and Hypersomnia Syndromes". Neurotherapeutics. 9 (4): 739–52. doi:10.1007/s13311-012-0150-9. PMC 3480574
 . PMID 23065655.
. PMID 23065655. - ↑ "Diagnosis of Idiopathic Hypersomnia/ Major Hypersomnolence Disorder". Retrieved 23 April 2013.
- ↑ "Recent Updates to Proposed Revisions for DSM-5: Sleep-Wake Disorders". DSM-5 Development. American Psychiatric Association.
- ↑ Vernet, Cyrille (2009). "Narcolepsy with Long Sleep Time". Sleep.
- ↑ "Stanford: Narcolepsy Medications (Stanford)". med.stanford.edu. Retrieved 24 May 2012.
- ↑ "Modafinil (marketed as Provigil): Serious Skin Reactions". Postmarketing Reviews. 1 (1). Fall 2007. Retrieved 15 March 2016.
- ↑ "Stanford Center for Narcolepsy article".
- ↑ Helmus T, Rosenthal L, Bishop C, Roehrs T, Syron ML, Roth T; Rosenthal; Bishop; Roehrs; Syron; Roth (1997). "The alerting effects of short and long naps in narcoleptic, sleep deprived, and alert individuals". Sleep. 20 (4): 251–7. PMID 9231950.
- 1 2 "XYREM® (sodium oxybate)" (PDF). United States Food and Drug Administration. Jazz Pharmaceuticals, Inc. 11 April 2014. Retrieved 9 August 2015.
- ↑ "FDA Approval Letter for Xyrem; Indication: Cataplexy associated with narcolepsy; 17 Jul 2002" (PDF).
- ↑ Wise MS, Arand DL, Auger RR, Brooks SN, Watson NF; Arand; Auger; Brooks; Watson; American Academy of Sleep Medicine (Dec 2007). "Treatment of narcolepsy and other hypersomnias of central origin". Sleep. 30 (12): 1712–27. PMC 2276130
 . PMID 18246981.
. PMID 18246981. - ↑ Boscolo-Berto, R; Viel, G; Montagnese, S; Raduazzo, DI; Ferrara, SD; Dauvilliers, Y (October 2012). "Narcolepsy and effectiveness of gamma-hydroxybutyrate (GHB): a systematic review and meta-analysis of randomized controlled trials.". Sleep medicine reviews. 16 (5): 431–43. doi:10.1016/j.smrv.2011.09.001. PMID 22055895.
- ↑ Gowda CR, Lundt LP; Lundt (December 2014). "Mechanism of action of narcolepsy medications". CNS Spectrums. 19 (Supplement 1): 25–33. doi:10.1017/S1092852914000583. PMID 25403789.
- ↑ Caputo F, Zoli G (March 2007). "Treatment of narcolepsy with cataplexy". Lancet. 369 (9567): 1080–1. doi:10.1016/S0140-6736(07)60522-4. PMID 17398302.
- ↑ "NAMI, National Alliance on Mental Illness, Effexor, Common Side Effects".
- 1 2 "Who Is At Risk for Narcolepsy?".
- ↑ "Link Between Narcolepsy and Mental Health". Retrieved 6 June 2014.
- ↑ "PC Joe Penhale | Doc Martin". Docmartinfan.com. Retrieved 3 March 2014.
- ↑ "Naan Sigappu Manithan - The Times of India". The Times Of India.
- ↑ "Judge, Jury and Executioner" at the Internet Movie Database
- ↑ "DH funds private prescriptions for drug denied to NHS patients". Health Service Journal. 20 July 2015. Retrieved 20 July 2015.
- ↑ "Hypersomnia Foundation - Treatment". Retrieved 25 January 2013.
- 1 2 Lynn Marie Trotti, MD (9 August 2010). "Flumazenil for the Treatment of Primary Hypersomnia". Emory University - Georgia Research Alliance. ClinicalTrials.gov. Retrieved 25 January 2013.
- 1 2 Lynn Marie Trotti, MD (15 June 2010). "Clarithromycin for the Treatment of Primary Hypersomnia". Emory University - Georgia Research Alliance. ClinicalTrials.gov. Retrieved 25 January 2013.
- ↑ Rye DB, Bliwise DL, Parker K, Trotti LM, Saini P, Fairley J, Freeman A, Garcia PS, Owens MJ, Ritchie JC, Jenkins A; Bliwise; Parker; Trotti; Saini; Fairley; Freeman; Garcia; Owens; Ritchie; Jenkins (21 November 2012). "Modulation of Vigilance in the Primary Hypersomnias by Endogenous Enhancement of GABAA Receptors". Sci. Transl. Med. 4 (161): 161ra151. doi:10.1126/scitranslmed.3004685. PMID 23175709.
- ↑ E. Kelty; V. Martyn; G. O’Neil; G. Hulse (19 February 2014). "Use of subcutaneous flumazenil preparations for the treatment of idiopathic hypersomnia: A case report". Journal of Psychopharmacology. 28 (7): 703–706. doi:10.1177/0269881114523865. PMID 24554692.
- ↑ Beck, Melinda (2012-12-10). "Scientists Try to Unravel the Riddle of Too Much Sleep". The Wall Street Journal.
- ↑ "Hypersomnia Update". Emory University. Retrieved 2014-04-22.
- ↑ Trotti, L; et al. (June 2013). "Clarithromycin for the Treatment of Hypersomnia: A Randomized, Double-Blind, Placebo-Controlled, Crossover Trial". Sleep. 36 (Abstract Supplement): A248.
- ↑ Trotti LM, Saini P, Freeman AA, Bliwise DL, García PS, Jenkins A, Rye DB; Saini; Freeman; Bliwise; García; Jenkins; Rye (2013). "Improvement in daytime sleepiness with clarithromycin in patients with GABA-related hypersomnia: Clinical experience". J. Psychopharmacol. (Oxford). 28 (7): 697–702. doi:10.1177/0269881113515062. PMID 24306133.
- ↑ Miyagawa T, Miyadera H, Tanaka S, Kawashima M, Shimada M, Honda Y, Tokunaga K, Honda M; Miyadera; Tanaka; Kawashima; Shimada; Honda; Tokunaga; Honda (2011). "Abnormally low serum acylcarnitine levels in narcolepsy patients". Sleep. 34 (3): 349–53A. PMC 3041711
 . PMID 21358852.
. PMID 21358852. - ↑ Miyagawa T, Honda M, Kawashima M, Shimada M, Tanaka S, Honda Y, Tokunaga K; Honda; Kawashima; Shimada; Tanaka; Honda; Tokunaga (30 April 2009). Rubinsztein, David C, ed. "Polymorphism Located between CPT1B and CHKB, and HLA-DRB1*1501-DQB1*0602 Haplotype Confer Susceptibility to CNS Hypersomnias (Essential Hypersomnia)". PLoS ONE. 4 (4): e5394. Bibcode:2009PLoSO...4.5394M. doi:10.1371/journal.pone.0005394. PMC 2671172
 . PMID 19404393.
. PMID 19404393. - ↑ Miyagawa T, Kawamura H, Obuchi M, Ikesaki A, Ozaki A, Tokunaga K, Inoue Y, Honda M; Kawamura; Obuchi; Ikesaki; Ozaki; Tokunaga; Inoue; Honda (2013). "Effects of oral L-carnitine administration in narcolepsy patients: A randomized, double-blind, cross-over and placebo-controlled trial". PLoS ONE. 8 (1): e53707. Bibcode:2013PLoSO...853707M. doi:10.1371/journal.pone.0053707. PMC 3547955
 . PMID 23349733.
. PMID 23349733.
Sources
- Mitler MM, Hajdukovic R; Hajdukovic (June 1991). "Relative Efficacy of Drugs for the Treatment of Sleepiness in Narcolepsy". Sleep. 14 (3): 218–20. PMC 2246380
 . PMID 1680245.
. PMID 1680245. - Chabas D, Taheri S, Renier C, Mignot E; Taheri; Renier; Mignot (October 2003). "The Genetics of Narcolepsy". Annual Review of Genomics and Human Genetics. 4: 459–83. doi:10.1146/annurev.genom.4.070802.110432. PMID 14527309.
- Smith AJ, Jackson MW, Neufing P, McEvoy RD, Gordon TP; Jackson; Neufing; McEvoy; Gordon (2004). "A functional autoantibody in narcolepsy". Lancet. 364 (9451): 2122–4. doi:10.1016/S0140-6736(04)17553-3. PMID 15589310.
External links
| Wikimedia Commons has media related to Narcolepsy. |
- Narcolepsy Fact Sheet: National Institute of Neurological Disorders and Stroke
- NARCOLEPSY: NOT ALONE international campaign by Project Sleep
- Narcolepsy UK
- Narcolepsy website from the Harvard Medical School Division of Sleep Medicine