Mitral insufficiency
| Mitral insufficiency | |
|---|---|
 | |
|
Mitral regurgitation (schematic drawing) During systole, contraction of the left ventricle causes abnormal backflow (arrow) into the left atrium. 1 Mitral valve 2 Left Ventricle 3 Left Atrium 4 Aorta | |
| Classification and external resources | |
| Specialty | Cardiology |
| ICD-10 | I05.1, I34.0, Q23.3 |
| ICD-9-CM | 394.1, 424.0, 746.6 |
| DiseasesDB | 8275 |
| MedlinePlus | 000176 |
| eMedicine | emerg/314 |
| MeSH | D008944 |
Mitral insufficiency (MI), mitral regurgitation or mitral incompetence is a disorder of the heart in which the mitral valve does not close properly when the heart pumps out blood. It is the abnormal leaking of blood backwards from the left ventricle, through the mitral valve, into the left atrium, when the left ventricle contracts, i.e. there is regurgitation of blood back into the left atrium.[1] MI is the most common form of valvular heart disease.[2]
Signs and symptoms
The symptoms associated with MI are dependent on which phase of the disease process the individual is in. Individuals with acute MI are typically severely symptomatic and will have the signs and symptoms of acute decompensated congestive heart failure (i.e. shortness of breath, pulmonary edema, orthopnea, and paroxysmal nocturnal dyspnea[3]), as well as symptoms of cardiogenic shock (i.e., shortness of breath at rest). Cardiovascular collapse with shock (cardiogenic shock) may be seen in individuals with acute MI due to papillary muscle rupture, rupture of a chorda tendinea or infective endocarditis of the mitral valve.
Individuals with chronic compensated MI may be asymptomatic for long periods of time, with a normal exercise tolerance and no evidence of heart failure. Over time, however, there may be decompensation and patients can develop volume overload (congestive heart failure). Symptoms of entry into a decompensated phase may include fatigue, shortness of breath particularly on exertion, and leg swelling. Also there may be development of an irregular heart rhythm known as atrial fibrillation.[3]
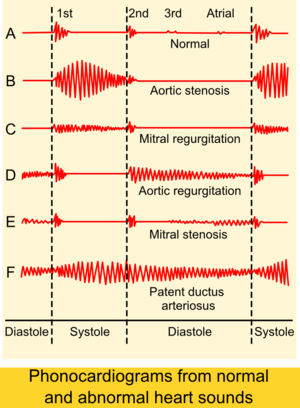
Findings on clinical examination depend on the severity and duration of MI. The mitral component of the first heart sound is usually soft and with a laterally displaced apex beat,[3] often with heave.[4] The first heart sound is followed by a high-pitched holosystolic murmur at the apex, radiating to the back or clavicular area.[3] Its duration is, as the name suggests, the whole of systole. The loudness of the murmur does not correlate well with the severity of regurgitation. It may be followed by a loud, palpable P2,[3] heard best when lying on the left side.[4] A third heart sound is commonly heard.[3]
In acute cases, the murmur and tachycardia may be the only distinctive signs.[4]
Patients with mitral valve prolapse may have a holosystolic murmur or often a mid-to-late systolic click and a late systolic murmur. Cases with a late systolic regurgitant murmur may still be associated with significant hemodynamic consequences.[5]
Cause

The mitral valve apparatus comprises two valve leaflets, the mitral valve annulus, which forms a ring around the valve leaflets, and the papillary muscles, which tether the valve leaflets to the left ventricle and prevent them from prolapsing into the left atrium. The chordae tendineae are also present and connect the valve leaflets to the papillary muscles. Dysfunction of any of these portions of the mitral valve apparatus can cause regurgitation.
The most common cause of MI in developing countries is mitral valve prolapse (MVP). Mitral valve prolapse is in turn is caused by myxomatous degeneration,[6] and is the most common cause of primary mitral regurgitation in the United States, causing about 50% of cases. Myxomatous degeneration of the mitral valve is more common in women as well as with advancing age, which causes a stretching of the leaflets of the valve and the chordae tendineae. Such elongation prevents the valve leaflets from fully coming together when the valve closes, causing the valve leaflets to prolapse into the left atrium, thereby causing MI.
Ischemic heart disease causes MI by the combination of ischemic dysfunction of the papillary muscles, and the dilatation of the left ventricle. This can lead to the subsequent displacement of the papillary muscles and the dilatation of the mitral valve annulus.
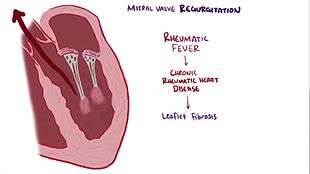
Rheumatic fever and Marfan's syndrome are other typical causes.[3] MI and mitral valve prolapse are also common in Ehlers Danlos Syndrome.[7]
Secondary mitral insufficiency is due to the dilatation of the left ventricle that causes stretching of the mitral valve annulus and displacement of the papillary muscles. This dilatation of the left ventricle can be due to any cause of dilated cardiomyopathy including aortic insufficiency, nonischemic dilated cardiomyopathy, and Noncompaction Cardiomyopathy. Because the papillary muscles, chordae, and valve leaflets are usually normal in such conditions, it is also called functional mitral insufficiency.[8]
Acute MI is most often caused by endocarditis, mainly S. aureus.[3] Rupture or dysfunction of the papillary muscle are also common causes in acute cases,[3] dysfunction, which can include mitral valve prolapse.[4]
Pathophysiology
The pathophysiology of MI can be broken into three phases of the disease process: the acute phase, the chronic compensated phase, and the chronic decompensated phase.[9]
Acute phase
Acute MI (as may occur due to the sudden rupture of a chorda tendinae or papillary muscle) causes a sudden volume overload of both the left atrium and the left ventricle. The left ventricle develops volume overload because with every contraction it now has to pump out not only the volume of blood that goes into the aorta (the forward cardiac output or forward stroke volume) but also the blood that regurgitates into the left atrium (the regurgitant volume). The combination of the forward stroke volume and the regurgitant volume is known as the total stroke volume of the left ventricle.
In the acute setting, the stroke volume of the left ventricle is increased (increased ejection fraction); this happens because of more complete emptying of the heart. However, as it progresses the LV volume increases and the contractile function deteriorates, thus leading to dysfunctional LV and a decrease in ejection fraction.[10] The increase in stroke volume is explained by the Frank–Starling mechanism, in which increased ventricular pre-load stretches the myocardium such that contractions are more forceful.
The regurgitant volume causes a volume overload and a pressure overload of the left atrium and the left ventricle. The increased pressures in the left side of the heart may inhibit drainage of blood from the lungs via the pulmonary veins and lead to pulmonary congestion.
Chronic phase
Compensated
If the MI develops slowly over months to years or if the acute phase cannot be managed with medical therapy, the individual will enter the chronic compensated phase of the disease. In this phase, the left ventricle develops eccentric hypertrophy in order to better manage the larger than normal stroke volume. The eccentric hypertrophy and the increased diastolic volume combine to increase the stroke volume (to levels well above normal) so that the forward stroke volume (forward cardiac output) approaches the normal levels.
In the left atrium, the volume overload causes enlargement of the left atrium, allowing the filling pressure in the left atrium to decrease. This improves the drainage from the pulmonary veins, and signs and symptoms of pulmonary congestion will decrease.
These changes in the left ventricle and left atrium improve the low forward cardiac output state and the pulmonary congestion that occur in the acute phase of the disease. Individuals in the chronic compensated phase may be asymptomatic and have normal exercise tolerances.
Decompensated
An individual may be in the compensated phase of MI for years, but will eventually develop left ventricular dysfunction, the hallmark for the chronic decompensated phase of mitral insufficiency. It is currently unclear what causes an individual to enter the decompensated phase of this disease. However, the decompensated phase is characterized by calcium overload within the cardiac myocytes.
In this phase, the ventricular myocardium is no longer able to contract adequately to compensate for the volume overload of mitral regurgitation, and the stroke volume of the left ventricle will decrease. The decreased stroke volume causes a decreased forward cardiac output and an increase in the end-systolic volume. The increased end-systolic volume translates to increased filling pressures of the left ventricle and increased pulmonary venous congestion. The individual may again have symptoms of congestive heart failure.
The left ventricle begins to dilate during this phase. This causes a dilatation of the mitral valve annulus, which may worsen the degree of MI. The dilated left ventricle causes an increase in the wall stress of the cardiac chamber as well.
While the ejection fraction is less in the chronic decompensated phase than in the acute phase or the chronic compensated phase, it may still be in the normal range (i.e.: > 50 percent), and may not decrease until late in the disease course. A decreased ejection fraction in an individual with mitral insufficiency and no other cardiac abnormality should alert the physician that the disease may be in its decompensated phase.
Diagnosis
There are many diagnostic tests that have abnormal results in the presence of MI. These tests suggest the diagnosis of MI and may indicate to the physician that further testing is warranted. For instance, the electrocardiogram (ECG) in long-standing MI may show evidence of left atrial enlargement and left ventricular hypertrophy. Atrial fibrillation may also be noted on the ECG in individuals with chronic mitral regurgitation. The ECG may not show any of these findings in the setting of acute MI.
| Acute | Chronic | |
|---|---|---|
| Electrocardiogram | Normal | P mitrale, Atrial fibrillation, left ventricular hypertrophy |
| Heart size | Normal | Cardiomegaly, left atrial enlargement |
| Systolic murmur | Heard at the base, radiates to the neck, spine, or top of head | Heard at the apex, radiates to the axilla |
| Apical thrill | May be absent | Present |
| Jugular venous distension | Present | Absent |
The quantification of MI usually employs imaging studies such as echocardiography or magnetic resonance angiography of the heart.
Chest X-ray
The chest X-ray in individuals with chronic MI is characterized by enlargement of the left atrium and the left ventricle.[3] The pulmonary vascular markings are typically normal, since pulmonary venous pressures are usually not significantly elevated.
Echocardiography

The echocardiogram is commonly used to confirm the diagnosis of MI. Color doppler flow on the transthoracic echocardiogram (TTE) will reveal a jet of blood flowing from the left ventricle into the left atrium during ventricular systole. Also, it may detect a dilated left atrium and ventricle and decreased left ventricular function.[3]
Because of inability to obtain accurate images of the left atrium and the pulmonary veins with a transthoracic echocardiogram, a transesophageal echocardiogram may be necessary in some cases to determine the severity of MI.
Electrocardiography
P mitrale is broad, notched P waves in several or many leads with a prominent late negative component to the P wave in lead V1, and may be seen in MI, but also in mitral stenosis, and, potentially, any cause of overload of the left atrium.[11] Thus, P-sinistrocardiale may be a more appropriate term.[11]
Quantification of mitral insufficiency
The degree of severity of MI can be quantified by the regurgitant fraction, which is the percentage of the left ventricular stroke volume that regurgitates into the left atrium.
- regurgitant fraction =
where Vmitral and Vaortic are, respectively, the volumes of blood that flow forward through the mitral valve and aortic valve during a cardiac cycle. Methods that have been used to assess the regurgitant fraction in mitral regurgitation include echocardiography, cardiac catheterization, fast CT scan, and cardiac MRI.
The echocardiographic technique to measure the regurgitant fraction is to determine the forward flow through the mitral valve (from the left atrium to the left ventricle) during ventricular diastole, and comparing it with the flow out of the left ventricle through the aortic valve in ventricular systole. This method assumes that the aortic valve does not suffer from aortic insufficiency.
Another way to quantify the degree of MI is to determine the area of the regurgitant flow at the level of the valve. This is known as the regurgitant orifice area, and correlates with the size of the defect in the mitral valve. One particular echocardiographic technique used to measure the orifice area is measurement of the proximal isovelocity surface area (PISA). The flaw of using PISA to determine the mitral valve regurgitant orifice area is that it measures the flow at one moment in time in the cardiac cycle, which may not reflect the average performance of the regurgitant jet.
| Degree of mitral regurgitation | Regurgitant fraction | Regurgitant Orifice area |
|---|---|---|
| Mild | < 20 percent | |
| Moderate | 20 - 40 percent | |
| Moderate to severe | 40 - 60 percent | |
| Severe | > 60 percent | > 0.4 cm2 |
Treatment
The treatment of mitral insufficiency depends on the acuteness of the disease and whether there are associated signs of hemodynamic compromise.
In acute MI secondary to a mechanical defect in the heart (i.e., rupture of a papillary muscle or chordae tendineae), the treatment of choice is mitral valve surgery. If the patient is hypotensive prior to the surgical procedure, an intra-aortic balloon pump may be placed in order to improve perfusion of the organs and to decrease the degree of MI.[3]
If the individual with acute MI is normotensive, vasodilators may be of use to decrease the afterload seen by the left ventricle and thereby decrease the regurgitant fraction. The vasodilator most commonly used is nitroprusside.
Individuals with chronic MI can be treated with vasodilators as well to decrease afterload.[3] In the chronic state, the most commonly used agents are ACE inhibitors and hydralazine. Studies have shown that the use of ACE inhibitors and hydralazine can delay surgical treatment of mitral insufficiency.[12][13] The current guidelines for treatment of MI limit the use of vasodilators to individuals with hypertension, however. Any hypertension is treated aggressively,[4] e.g. by diuretics and a low-sodium diet.[3] In both hypertensive and normotensive cases, digoxin and antiarrhythmics are also indicated.[3][4] Also, chronic anticoagulation is given where there is concomitant mitral valve prolapse[4] or atrial fibrillation.[3] In general, medical therapy is non-curative and is used for mild-to-moderate regurgitation or in patients unable to tolerate surgery.
Surgery is curative of mitral valve regurgitation. There are two surgical options for the treatment of MI: mitral valve replacement and mitral valve repair.[3] Mitral valve repair is preferred to mitral valve replacement where a repair is feasible as bioprosthetic replacement valves have a limited lifespan of 10 to 15 years, whereas synthetic replacement valves require ongoing use of blood thinners to reduce the risk of stroke. There are two general categories of approaches to mitral valve repair: Resection of the prolapsed valvular segment (sometimes referred to as the 'Carpentier' approach), and installation of artificial chordae to "anchor" the prolapsed segment to the papillary muscle (sometimes referred to as the 'David' approach). With the resection approach, any prolapsing tissue is resected, in effect removing the hole through which the blood is leaking. In the artificial chordae approach, ePTFE (expanded polytetrafluoroethylene, or Gore-Tex™ sutures are used to replace the broken or stretched chordae tendonae, bringing the natural tissue back into the physiological position, thus restoring the natural anatomy of the valve. With both techniques, an annuloplasty ring is typically secured to the annulus, or opening of the mitral valve, to provide additional structural support. In some cases, the "double orifice" (or 'Alfieri') technique for mitral valve repair, the opening of the mitral valve is sewn closed in the middle, leaving the two ends still able to open. This ensures that the mitral valve closes when the left ventricle pumps blood, yet allows the mitral valve to open at the two ends to fill the left ventricle with blood before it pumps. In general, mitral valve surgery requires "open-heart" surgery in which the heart is arrested and the patient is placed on a heart-lung machine (cardiopulmonary bypass). This allows the complex surgery to proceed in a still environment.
Due to the physiological stress associated with open-heart surgery, elderly and very sick patients may be subject to increased risk, and may not be candidates for this type of surgery. As a consequence, there are attempts to identify means of correcting MI on a beating heart. The Alfieri technique for instance, has been replicated using a percutaneous catheter technique, which installs a clip to hold the middle of the mitral valve closed.[14][15][16]
Surgery
Indications for surgery for chronic MI include signs of left ventricular dysfunction with ejection fraction less than 60%, severe pulmonary hypertension with pulmonary artery systolic pressure greater than 50 mmHg at rest or 60 mmHg during activity, and new onset atrial fibrillation.
| Symptoms | LV EF | LVESD |
|---|---|---|
| NYHA II | > 30 percent | < 55 mm |
| NYHA III-IV | < 30 percent | > 55 mm |
| Asymptomatic | 30 - 60 percent | ≥ 40 mm |
| Asymptomatic with pulmonary hypertension | LV EF > 60 percent and pulmonary artery systolic pressure >50-60 mmHg | |
| Asymptomatic and chance for a repair without residual MI is >90% | > 60 percent | < 40 mm |
Epidemiology
Significant mitral valve regurgitation has a prevalence of approximately 2% of the population, affecting males and females equally.[18] It is one of the two most common valvular heart diseases in the elderly.[19]
References
- ↑ Mitral valve regurgitation at Mount Sinai Hospital
- ↑ Weinrauch, LA (2008-05-12). "Mitral regurgitation - chronic". Medline Plus Encyclopedia. U.S. National Library of Medicine and National Institutes of Health. Retrieved 2009-12-04.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6. Chapter 1: Diseases of the Cardiovascular system > Section: Valvular Heart Disease
- 1 2 3 4 5 6 7 VOC=VITIUM ORGANICUM CORDIS, a compendium of the Department of Cardiology at Uppsala Academic Hospital. By Per Kvidal September 1999, with revision by Erik Björklund May 2008
- ↑ "Mitral valve prolapse with a late-systolic regurgitant murmur may be associated with significant hemodynamic consequences.". Am J Med Sci. 338 (2): 113–5. Aug 2009. doi:10.1097/MAJ.0b013e31819d5ec6. PMID 19561453.
- ↑ Kulick, Daniel. "Mitral Valve Prolapse (MVP)". MedicineNet.com. MedicineNet, Inc. Retrieved 2010-01-18.
- ↑ NIH US National Library of Medicine, A.D.A.M. Medical Encyclopedia, Ehlers Danlos Syndrome- PMH0002439
- ↑ Functional mitral regurgitation By William H Gaasch, MD. Retrieved on Jul 8, 2010
- ↑ Di Sandro, D (2009-06-08). "Mitral Regurgitation". eMedicine. Medscape. Retrieved 2009-12-08.
- ↑ Harrison's Internal Medicine 17th edition
- 1 2 medilexicon.com < P mitrale Citing. Stedman's Medical Dictionary. Copyright 2006
- ↑ Greenberg BH, Massie BM, Brundage BH, Botvinick EH, Parmley WW, Chatterjee K (1978). "Beneficial effects of hydralazine in severe mitral regurgitation". Circulation. 58 (2): 273–9. doi:10.1161/01.cir.58.2.273. PMID 668075.
- ↑ Hoit BD (1991). "Medical treatment of valvular heart disease". Curr. Opin. Cardiol. 6 (2): 207–11. doi:10.1097/00001573-199104000-00005. PMID 10149580.
- ↑ Tirrell, Meg (2010-03-14). "Abbott MitraClip Offers Safe Alternative to Open-Heart Surgery". Bloomberg Business Week. Bloomberg L.P. Retrieved 2010-03-14.
- ↑ Garg P, Walton AS (June 2008). "The new world of cardiac interventions: a brief review of the recent advances in non-coronary percutaneous interventions". Heart Lung Circ. 17 (3): 186–99. doi:10.1016/j.hlc.2007.10.019. PMID 18262841.
- ↑ Feldman M.D., Ted; Elyse Foster, M.D., Donald G. Glower, M.D., Saibal Kar, M.D., Michael J. Rinaldi, M.D., Peter S. Fail, M.D., Richard W. Smalling, M.D., Ph.D., Robert Siegel, M.D., Geoffrey A. Rose, M.D., Eric Engeron, M.D., Catalin Loghin, M.D., Alfredo Trento, M.D., Eric R. Skipper, M.D., Tommy Fudge, M.D., George V. Letsou, M.D., Joseph M. Massaro, Ph.D., and Laura Mauri, M.D. for the EVEREST II Investigators (14 April 2011). "Percutaneous Repair or Surgery for Mitral Regurgitation". New England Journal of Medicine. 364: 1395–1406. doi:10.1056/NEJMoa1009355. Cite uses deprecated parameter
|coauthors=(help) - ↑ Bonow R, et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons.". Circulation. 118 (15): e523. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ The Cleveland Clinic Center for Continuing Education > Mitral Valve Disease: Stenosis and Regurgitation Authors: Ronan J. Curtin and Brian P. Griffin. Retrieved September 2010
- ↑ Valvular heart disease in elderly adults Authors: Dania Mohty, Maurice Enriquez-Sarano. Section Editors:Catherine M Otto, Kenneth E Schmader. Deputy Editor: Susan B Yeon. This topic last updated: April 20, 2007. Last literature review version 18.2: May 2010
External links
- MitraClip Film
- Echocardiographic features of mitral regurgitation at Wikiecho
- Mitral Regurgitation information from Seattle Children's Hospital Heart Center
- Educational Infographic about Mitral Regurgitation for patients, their families and friends