Mental disorder
| Mental disorder | |
|---|---|
| psychiatric disorder, psychological disorder, mental illness | |
|
Eight women representing prominent mental diagnoses in the 19th century at the Salpêtrière (Paris). (fr. Armand Gautier) | |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | F99 |
| ICD-9-CM | 290-319 |
| DiseasesDB | 28852 |
| MeSH | D001523 |
A mental disorder, also called a mental illness[1] or psychiatric disorder, is a diagnosis by a mental health professional of a behavioral or mental pattern that may cause suffering or a poor ability to function in life. Such features may be persistent, relapsing and remitting, or occur as a single episode. Many disorders have been described, with signs and symptoms that vary widely between specific disorders.[2][3]
The causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks.[2] This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of mental health. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.[4]
Services are based in psychiatric hospitals or in the community, and assessments are carried out by psychiatrists, clinical psychologists, and clinical social workers, using various methods but often relying on observation and questioning. Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options. Other treatments include social interventions, peer support, and self-help. In a minority of cases there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.[2]
Common mental disorders include depression, which affects about 400 million, dementia which affects about 35 million, and schizophrenia, which affects about 21 million people globally.[2] Stigma and discrimination can add to the suffering and disability associated with mental disorders, leading to various social movements attempting to increase understanding and challenge social exclusion.
Definition
The definition and classification of mental disorders are key issues for researchers as well as service providers and those who may be diagnosed. For a mental state to classify as a disorder, it generally needs to cause dysfunction.[5] Most international clinical documents use the term mental "disorder", while "illness" is also common. It has been noted that using the term "mental" (i.e., of the mind) is not necessarily meant to imply separateness from brain or body.
According to DSM-IV, a mental disorder is a psychological syndrome or pattern which is associated with distress (e.g. via a painful symptom), disability (impairment in one or more important areas of functioning), increased risk of death, or causes a significant loss of autonomy; however it excludes normal responses such as grief from loss of a loved one, and also excludes deviant behavior for political, religious, or societal reasons not arising from a dysfunction in the individual.[6][7]
DSM-IV precedes the definition with caveats, stating that, as in the case with many medical terms, mental disorder "lacks a consistent operational definition that covers all situations", noting that different levels of abstraction can be used for medical definitions, including pathology, symptomology, deviance from a normal range, or etiology, and that the same is true for mental disorders, so that sometimes one type of definition is appropriate, and sometimes another, depending on the situation.[8]
Classifications
There are currently two widely established systems that classify mental disorders;
- ICD-10 Chapter V: Mental and behavioural disorders, since 1949 part of the International Classification of Diseases produced by the WHO,
- the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) produced by the American Psychiatric Association (APA) since 1952.
Both these list categories of disorder and provide standardized criteria for diagnosis. They have deliberately converged their codes in recent revisions so that the manuals are often broadly comparable, although significant differences remain. Other classification schemes may be used in non-western cultures, for example the Chinese Classification of Mental Disorders, and other manuals may be used by those of alternative theoretical persuasions, for example the Psychodynamic Diagnostic Manual. In general, mental disorders are classified separately from neurological disorders, learning disabilities or intellectual disability.
Unlike the DSM and ICD, some approaches are not based on identifying distinct categories of disorder using dichotomous symptom profiles intended to separate the abnormal from the normal. There is significant scientific debate about the relative merits of categorical versus such non-categorical (or hybrid) schemes, also known as continuum or dimensional models. A spectrum approach may incorporate elements of both.
In the scientific and academic literature on the definition or classification of mental disorder, one extreme argues that it is entirely a matter of value judgements (including of what is normal) while another proposes that it is or could be entirely objective and scientific (including by reference to statistical norms).[9] Common hybrid views argue that the concept of mental disorder is objective even if only a "fuzzy prototype" that can never be precisely defined, or conversely that the concept always involves a mixture of scientific facts and subjective value judgments.[10] Although the diagnostic categories are referred to as 'disorders', they are presented as medical diseases, but are not validated in the same way as most medical diagnoses. Some neurologists argue that classification will only be reliable and valid when based on neurobiological features rather than clinical interview, while others suggest that the differing ideological and practical perspectives need to be better integrated.[11][12]
The DSM and ICD approach remains under attack both because of the implied causality model[13] and because some researchers believe it better to aim at underlying brain differences which can precede symptoms by many years.[14]
Disorders
There are many different categories of mental disorder, and many different facets of human behavior and personality that can become disordered.[15][16][17][18][19]
Anxiety or fear that interferes with normal functioning may be classified as an anxiety disorder.[16] Commonly recognized categories include specific phobias, generalized anxiety disorder, social anxiety disorder, panic disorder, agoraphobia, obsessive-compulsive disorder and post-traumatic stress disorder.
Other affective (emotion/mood) processes can also become disordered. Mood disorder involving unusually intense and sustained sadness, melancholia, or despair is known as major depression (also known as unipolar or clinical depression). Milder but still prolonged depression can be diagnosed as dysthymia. Bipolar disorder (also known as manic depression) involves abnormally "high" or pressured mood states, known as mania or hypomania, alternating with normal or depressed mood. The extent to which unipolar and bipolar mood phenomena represent distinct categories of disorder, or mix and merge along a dimension or spectrum of mood, is subject to some scientific debate.[20]
Patterns of belief, language use and perception of reality can become disordered (e.g., delusions, thought disorder, hallucinations). Psychotic disorders in this domain include schizophrenia, and delusional disorder. Schizoaffective disorder is a category used for individuals showing aspects of both schizophrenia and affective disorders. Schizotypy is a category used for individuals showing some of the characteristics associated with schizophrenia but without meeting cutoff criteria.
Personality—the fundamental characteristics of a person that influence thoughts and behaviors across situations and time—may be considered disordered if judged to be abnormally rigid and maladaptive. Although treated separately by some, the commonly used categorical schemes include them as mental disorders, albeit on a separate "axis II" in the case of the DSM-IV. A number of different personality disorders are listed, including those sometimes classed as "eccentric", such as paranoid, schizoid and schizotypal personality disorders; types that have described as "dramatic" or "emotional", such as antisocial, borderline, histrionic or narcissistic personality disorders; and those sometimes classed as fear-related, such as anxious-avoidant, dependent, or obsessive-compulsive personality disorders. The personality disorders in general are defined as emerging in childhood, or at least by adolescence or early adulthood. The ICD also has a category for enduring personality change after a catastrophic experience or psychiatric illness. If an inability to sufficiently adjust to life circumstances begins within three months of a particular event or situation, and ends within six months after the stressor stops or is eliminated, it may instead be classed as an adjustment disorder. There is an emerging consensus that so-called "personality disorders", like personality traits in general, actually incorporate a mixture of acute dysfunctional behaviors that may resolve in short periods, and maladaptive temperamental traits that are more enduring.[21] Furthermore, there are also non-categorical schemes that rate all individuals via a profile of different dimensions of personality without a symptom-based cutoff from normal personality variation, for example through schemes based on dimensional models.[22]
Eating disorders involve disproportionate concern in matters of food and weight.[16] Categories of disorder in this area include anorexia nervosa, bulimia nervosa, exercise bulimia or binge eating disorder.
Sleep disorders such as insomnia involve disruption to normal sleep patterns, or a feeling of tiredness despite sleep appearing normal.
Sexual disorders and gender dysphoria may be diagnosed, including dyspareunia and ego-dystonic homosexuality. Various kinds of paraphilia are considered mental disorders (sexual arousal to objects, situations, or individuals that are considered abnormal or harmful to the person or others).
People who are abnormally unable to resist certain urges or impulses that could be harmful to themselves or others, may be classed as having an impulse control disorder, and disorders such as kleptomania (stealing) or pyromania (fire-setting). Various behavioral addictions, such as gambling addiction, may be classed as a disorder. Obsessive-compulsive disorder can sometimes involve an inability to resist certain acts but is classed separately as being primarily an anxiety disorder.
The use of drugs (legal or illegal, including alcohol), when it persists despite significant problems related to its use, may be defined as a mental disorder. The DSM incorporates such conditions under the umbrella category of substance use disorders, which includes substance dependence and substance abuse. The DSM does not currently use the common term drug addiction, and the ICD simply refers to "harmful use". Disordered substance use may be due to a pattern of compulsive and repetitive use of the drug that results in tolerance to its effects and withdrawal symptoms when use is reduced or stopped.
People who suffer severe disturbances of their self-identity, memory and general awareness of themselves and their surroundings may be classed as having a dissociative identity disorder, such as depersonalization disorder or Dissociative Identity Disorder itself (which has also been called multiple personality disorder, or "split personality"). Other memory or cognitive disorders include amnesia or various kinds of old age dementia.
A range of developmental disorders that initially occur in childhood may be diagnosed, for example autism spectrum disorders, oppositional defiant disorder and conduct disorder, and attention deficit hyperactivity disorder (ADHD), which may continue into adulthood.
Conduct disorder, if continuing into adulthood, may be diagnosed as antisocial personality disorder (dissocial personality disorder in the ICD). Popularist labels such as psychopath (or sociopath) do not appear in the DSM or ICD but are linked by some to these diagnoses.
Somatoform disorders may be diagnosed when there are problems that appear to originate in the body that are thought to be manifestations of a mental disorder. This includes somatization disorder and conversion disorder. There are also disorders of how a person perceives their body, such as body dysmorphic disorder. Neurasthenia is an old diagnosis involving somatic complaints as well as fatigue and low spirits/depression, which is officially recognized by the ICD-10 but no longer by the DSM-IV.[23]
Factitious disorders, such as Munchausen syndrome, are diagnosed where symptoms are thought to be experienced (deliberately produced) and/or reported (feigned) for personal gain.
There are attempts to introduce a category of relational disorder, where the diagnosis is of a relationship rather than on any one individual in that relationship. The relationship may be between children and their parents, between couples, or others. There already exists, under the category of psychosis, a diagnosis of shared psychotic disorder where two or more individuals share a particular delusion because of their close relationship with each other.
There are a number of uncommon psychiatric syndromes, which are often named after the person who first described them, such as Capgras syndrome, De Clerambault syndrome, Othello syndrome, Ganser syndrome, Cotard delusion, and Ekbom syndrome, and additional disorders such as the Couvade syndrome and Geschwind syndrome.[24]
Various new types of mental disorder diagnosis are occasionally proposed. Among those controversially considered by the official committees of the diagnostic manuals include self-defeating personality disorder, sadistic personality disorder, passive-aggressive personality disorder and premenstrual dysphoric disorder.
Two recent unique unofficial proposals are solastalgia by Glenn Albrecht and hubris syndrome by David Owen. The application of the concept of mental illness to the phenomena described by these authors has in turn been critiqued by Seamus Mac Suibhne.[25]
Signs and symptoms
Course
The likely course and outcome of mental disorders varies, and is dependent on numerous factors related to the disorder itself, the individual as a whole, and the social environment. Some disorders are transient, while others may be more chronic in nature.
Even those disorders often considered the most serious and intractable have varied courses i.e. schizophrenia, psychotic disorders, and personality disorders. Long-term international studies of schizophrenia have found that over a half of individuals recover in terms of symptoms, and around a fifth to a third in terms of symptoms and functioning, with some requiring no medication. At the same time, many have serious difficulties and support needs for many years, although "late" recovery is still possible. The World Health Organization concluded that the long-term studies' findings converged with others in "relieving patients, carers and clinicians of the chronicity paradigm which dominated thinking throughout much of the 20th century."[26][27]
Around half of people initially diagnosed with bipolar disorder achieve syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks, and nearly all achieve it within two years, with nearly half regaining their prior occupational and residential status in that period. However, nearly half go on to experience a new episode of mania or major depression within the next two years.[28] Functioning has been found to vary, being poor during periods of major depression or mania but otherwise fair to good, and possibly superior during periods of hypomania in Bipolar II.[29]
Disability
Some disorders may be very limited in their functional effects, while others may involve substantial disability and support needs. The degree of ability or disability may vary over time and across different life domains. Furthermore, continued disability has been linked to institutionalization, discrimination and social exclusion as well as to the inherent effects of disorders. Alternatively, functioning may be affected by the stress of having to hide a condition in work or school etc., by adverse effects of medications or other substances, or by mismatches between illness-related variations and demands for regularity.[30]
It is also the case that, while often being characterized in purely negative terms, some mental traits or states labeled as disorders can also involve above-average creativity, non-conformity, goal-striving, meticulousness, or empathy.[31] In addition, the public perception of the level of disability associated with mental disorders can change.[32]
Nevertheless, internationally, people report equal or greater disability from commonly occurring mental conditions than from commonly occurring physical conditions, particularly in their social roles and personal relationships. The proportion with access to professional help for mental disorders is far lower, however, even among those assessed as having a severely disabling condition.[33] Disability in this context may or may not involve such things as:
- Basic activities of daily living. Including looking after the self (health care, grooming, dressing, shopping, cooking etc.) or looking after accommodation (chores, DIY tasks etc.)
- Interpersonal relationships. Including communication skills, ability to form relationships and sustain them, ability to leave the home or mix in crowds or particular settings
- Occupational functioning. Ability to acquire a job and hold it, cognitive and social skills required for the job, dealing with workplace culture, or studying as a student.
In terms of total Disability-adjusted life years (DALYs), which is an estimate of how many years of life are lost due to premature death or to being in a state of poor health and disability, mental disorders rank amongst the most disabling conditions. Unipolar (also known as Major) depressive disorder is the third leading cause of disability worldwide, of any condition mental or physical, accounting for 65.5 million years lost. The total DALY does not necessarily indicate what is the most individually disabling, because it also depends on how common a condition is; for example, schizophrenia is found to be the most individually disabling mental disorder on average but is less common. Alcohol-use disorders are also high in the overall list, responsible for 23.7 million DALYs globally, while other drug-use disorders accounted for 8.4 million. Schizophrenia causes a total loss of 16.8 million DALY, and bipolar disorder 14.4 million. Panic disorder leads to 7 million years lost, obsessive-compulsive disorder 5.1, primary insomnia 3.6, and post-traumatic stress disorder 3.5 million DALYs.[34]
The first ever systematic description of global disability arising in youth, published in 2011, found that among 10- to 24-year-olds nearly half of all disability (current and as estimated to continue) was due to mental and neurological conditions, including substance use disorders and conditions involving self-harm. Second to this were accidental injuries (mainly traffic collisions) accounting for 12 percent of disability, followed by communicable diseases at 10 percent. The disorders associated with most disability in high income countries were unipolar major depression (20%) and alcohol use disorder (11%). In the eastern Mediterranean region it was unipolar major depression (12%) and schizophrenia (7%), and in Africa it was unipolar major depression (7%) and bipolar disorder (5%).[35]
Suicide, which is often attributed to some underlying mental disorder, is a leading cause of death among teenagers and adults under 35.[36][37] There are an estimated 10 to 20 million non-fatal attempted suicides every year worldwide.[38]
Causes
Risk factors for mental illness include genetic inheritance, such as parents having depression,[39] or a propensity for high neuroticism [40][41] or "emotional instability".
In depression, parenting risk factors include parental unequal treatment,[42] and there is association with high cannabis use.[43]
In schizophrenia and psychosis, risk factors include migration and discrimination, childhood trauma, bereavement or separation in families, and abuse of drugs,[44] including cannabis,[43] and urbanicity.[45]
In anxiety risk factors may include family history (e.g. of anxiety), temperament and attitudes (e.g. pessimism),[46] and parenting factors including parental rejection, lack of parental warmth, high hostility, harsh discipline, high maternal negative affect, anxious childrearing, modelling of dysfunctional and drug-abusing behaviour, and child abuse (emotional, physical and sexual).[47]
Environmental events surrounding pregnancy and birth have also been implicated. Traumatic brain injury may increase the risk of developing certain mental disorders. There have been some tentative inconsistent links found to certain viral infections, to substance misuse, and to general physical health.
Social influences have been found to be important,[48] including abuse, neglect, bullying, social stress, traumatic events and other negative or overwhelming life experiences. For bipolar disorder, stress (such as childhood adversity) is not a specific cause, but does place genetically and biologically vulnerable individuals at risk for a more severe course of illness.[49] The specific risks and pathways to particular disorders are less clear, however. Aspects of the wider community have also been implicated,[45] including employment problems, socioeconomic inequality, lack of social cohesion, problems linked to migration, and features of particular societies and cultures.
Drugs
Correlations of mental disorders with drug use include cannabis,[43] alcohol[50] and caffeine,[51] use of which appears to promote anxiety.[52] For psychosis and schizophrenia, usage of a number of drugs has been associated with development of the disorder, including cannabis, cocaine, and amphetamines.[53] There has been debate regarding the relationship between usage of cannabis and bipolar disorder.[54]
Genetics
Although researchers have been looking for decades for clear linkages between genetics and mental disorders to provide better diagnosis and facilitate the development of better treatments, that work has yielded almost nothing.[55]
Models
Mental disorders can arise from multiple sources, and in many cases there is no single accepted or consistent cause currently established. An eclectic or pluralistic mix of models may be used to explain particular disorders.[41][56] The primary paradigm of contemporary mainstream Western psychiatry is said to be the biopsychosocial model which incorporates biological, psychological and social factors, although this may not always be applied in practice.
Biological psychiatry follows a biomedical model where many mental disorders are conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience. A common assumption is that disorders may have resulted from genetic and developmental vulnerabilities, exposed by stress in life (for example in a diathesis–stress model), although there are various views on what causes differences between individuals. Some types of mental disorder may be viewed as primarily neurodevelopmental disorders.
Evolutionary psychology may be used as an overall explanatory theory, while attachment theory is another kind of evolutionary-psychological approach sometimes applied in the context of mental disorders. Psychoanalytic theories have continued to evolve alongside and cognitive-behavioral and systemic-family approaches. A distinction is sometimes made between a "medical model" or a "social model" of disorder and disability.
Diagnosis
Psychiatrists seek to provide a medical diagnosis of individuals by an assessment of symptoms and signs associated with particular types of mental disorder. Other mental health professionals, such as clinical psychologists, may or may not apply the same diagnostic categories to their clinical formulation of a client's difficulties and circumstances.[57] The majority of mental health problems are, at least initially, assessed and treated by family physicians (in the UK general practitioners) during consultations, who may refer a patient on for more specialist diagnosis in acute or chronic cases.
Routine diagnostic practice in mental health services typically involves an interview known as a mental status examination, where evaluations are made of appearance and behavior, self-reported symptoms, mental health history, and current life circumstances. The views of other professionals, relatives or other third parties may be taken into account. A physical examination to check for ill health or the effects of medications or other drugs may be conducted. Psychological testing is sometimes used via paper-and-pen or computerized questionnaires, which may include algorithms based on ticking off standardized diagnostic criteria, and in rare specialist cases neuroimaging tests may be requested, but such methods are more commonly found in research studies than routine clinical practice.[58][59]
Time and budgetary constraints often limit practicing psychiatrists from conducting more thorough diagnostic evaluations.[60] It has been found that most clinicians evaluate patients using an unstructured, open-ended approach, with limited training in evidence-based assessment methods, and that inaccurate diagnosis may be common in routine practice.[61] In addition, comorbidity is very common in psychiatric diagnosis, where the same person meets the criteria for more than one disorder. On the other hand, a person may have several different difficulties only some of which meet the criteria for being diagnosed. There may be specific problems with accurate diagnosis in developing countries.
More structured approaches are being increasingly used to measure levels of mental illness.
- HoNOS is the most widely used measure in English mental health services, being used by at least 61 trusts.[62] In HoNOS a score of 0–4 is given for each of 12 factors, based on functional living capacity.[63] Research has been supportive of HoNOS,[64] although some questions have been asked about whether it provides adequate coverage of the range and complexity of mental illness problems, and whether the fact that often only 3 of the 12 scales vary over time gives enough subtlety to accurately measure outcomes of treatment.[65]
Since the 1980s, Paula Caplan has been concerned about the subjectivity of psychiatric diagnosis, and people being arbitrarily “slapped with a psychiatric label”. Caplan says because psychiatric diagnosis is unregulated, doctors are not required to spend much time interviewing patients or to seek a second opinion. The Diagnostic and Statistical Manual of Mental Disorders can lead a psychiatrist to focus on narrow checklists of symptoms, with little consideration of what is actually causing the patient’s problems. So, according to Caplan, getting a psychiatric diagnosis and label often stands in the way of recovery.[66]
In 2013, psychiatrist Allen Frances wrote a paper entitled "The New Crisis of Confidence in Psychiatric Diagnosis", which said that "psychiatric diagnosis still relies exclusively on fallible subjective judgments rather than objective biological tests". Frances was also concerned about "unpredictable overdiagnosis".[67] For many years, marginalized psychiatrists (such as Peter Breggin, Thomas Szasz) and outside critics (such as Stuart A. Kirk) have "been accusing psychiatry of engaging in the systematic medicalization of normality". More recently these concerns have come from insiders who have worked for and promoted the American Psychiatric Association (e.g., Robert Spitzer, Allen Frances).[68] A 2002 editorial in the British Medical Journal warned of inappropriate medicalization leading to disease mongering, where the boundaries of the definition of illnesses are expanded to include personal problems as medical problems or risks of diseases are emphasized to broaden the market for medications.[69]
Prevention
The 2004 WHO report "Prevention of Mental Disorders" stated that "Prevention of these disorders is obviously one of the most effective ways to reduce the [disease] burden."[70]
The 2011 European Psychiatric Association (EPA) guidance on prevention of mental disorders states "There is considerable evidence that various psychiatric conditions can be prevented through the implementation of effective evidence-based interventions."[71]
A 2011 UK Department of Health report on the economic case for mental health promotion and mental illness prevention found that "many interventions are outstandingly good value for money, low in cost and often become self-financing over time, saving public expenditure".[72]
Parenting may affect the child's mental health, and evidence suggests that helping parents to be more effective with their children can address mental health needs.[73][74]
Universal prevention (aimed at a population that has no increased risk for developing a mental disorder, such as school programs or mass media campaigns) need very high numbers of people to show effect (sometimes known as the "power" problem). Approaches to overcome this are (1) focus on high-incidence groups (e.g. by targeting groups with high risk factors), (2) use multiple interventions to achieve greater, and thus more statistically valid, effects, (3) use cumulative meta-analyses of many trials, and (4) run very large trials.[75][76]
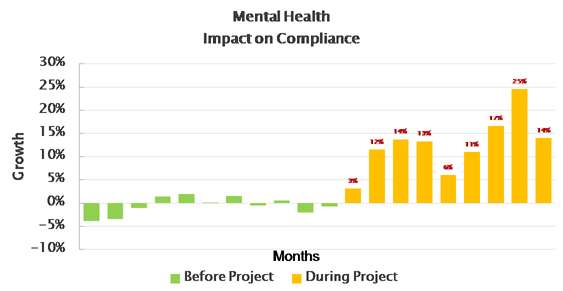
Depression
For depressive disorders, when people participated in interventions, the number of new cases is reduced by 22% to 38%.[77][78] These interventions included CBT.[79] Such interventions also save costs.[80] Depression prevention continues to be called for.[81]
Anxiety
For anxiety disorders,
- use of CBT with people at risk has significantly reduced the number of episodes of generalized anxiety disorder and other anxiety symptoms, and also given significant improvements in explanatory style, hopelessness, and dysfunctional attitudes.[46][82] Other interventions (parental inhibition reduction, behaviourism, parental modelling, problem-solving and communication skills) have also produced significant benefits.[46] People with subthreshold panic disorder were found to benefit from use of CBT.[83]
- for older people, a stepped-care intervention (watchful waiting, CBT and medication if appropriate) achieved a 50% lower incidence rate of depression and anxiety disorders in a patient group aged 75 or older.[84]
- for younger people, it has been found that teaching CBT in schools reduced anxiety in children,[85] and a review found that most universal, selective and indicated prevention programs are effective in reducing symptoms of anxiety in children and adolescents.[86]
Psychosis
In those at high risk there is tentative evidence that psychosis incidence may be reduced with the use of CBT or other types of therapy.[87][88] In 2014 the UK National Institute for Health and Care Excellence (NICE) recommended preventive CBT for people at risk of psychosis.[89][90]
There is also tentative evidence that treatment may help those with early symptoms.[91][92] Antipsychotic medications are not recommended for preventing psychosis.[89]
For schizophrenia, one study of preventative CBT showed a positive effect[93] and another showed neutral effect.[94]
Mental health strategies
Prevention is currently a very small part of the spend of mental health systems. For instance the 2009 UK Department of Health analysis of prevention expenditure does not include any apparent spend on mental health.[95] The situation is the same in research.[44]
However prevention is beginning to appear in mental health strategies:
- The US Substance Abuse and Mental Health Services Administration (SAMHSA) advocates a 5-step prevention framework.[96]
- In 2016:
- the UK NHS Mental Health Taskforce included 'preventing mental health' in its 3 Priorities, focusing on children and young ages, and the importance of employment.[97]
- the UK NGO Mental Health Foundation published a review of prevention approaches.[98]
- In 2015:
- the Hunter Institute of mental health in Australia published it's "Prevention First" strategic framework for prevention.[99]
- the UK NGO Mental Health Foundation published a review of prevention research, paving the way for prevention strategies.[100]
- the official journal of the World Psychiatric Association included a survey of public mental health which concluded "the evidence base for public mental health interventions is convincing, and the time is now ripe to move from knowledge to action".[101]
- In 2014 the UK Chief Medical Officer chose mental health for her major annual report, and included prevention of mental illness heavily in this.[102]
- In 2013 the Faculty of Public Health, the UK professional body for public health professionals, produced it's 'Better Mental Health for All" resource, which aims at "the promotion of mental wellbeing and the primary prevention of mental illness".[103]
- In 2012, Mind, the UK mental health NGO, included "Staying well; Support people likely to develop mental health problems, to stay well." as its first goal for 2012–16.[104]
- The 2011 mental health strategy of Manitoba (Canada) included intents to (i) reduce risk factors associated with mental ill-health and (ii) increase mental health promotion for both adults and children.[105]
- The 2011 US National Prevention Strategy included mental and emotional well-being, with recommendations including (i) better parenting and (ii) early intervention.[106]
- Australia's mental health plan for 2009–14 included "Prevention and Early Intervention" as priority 2.[107]
- The 2008 EU "Pact for Mental Health" made recommendations for youth and education including (i) promotion of parenting skills, (ii) integration of socio-emotional learning into education curricular and extracurricular activities, and (iii) early intervention throughout the educational system.[108]
- The 2006 Canadian "Out of the Shadows at last" included a section on prevention.[109]
Prevention programmes
- In 2013 the UK NGO Mental Health Foundation and partners began to use Video Interaction Guidance (VIG) in an early years intervention to reduce later life mental illness.[110][111]
- In 2013 in Australia the National Health and Medical Research Council supported a set of parenting strategies to prevent teenagers becoming anxious or depressed.[112][113]
- In 2012 the UK Schizophrenia Commission recommended "a preventative strategy for psychosis including promoting protective factors for mental wellbeing and reducing risks such as cannabis use in early adolescence."[44]
- In 2010 the European Union DataPrev database was launched. It states "A healthy start is crucial for mental health and wellbeing throughout life, with parenting being the single most important factor," and recommends a range of interventions.[114]
- In 2009 the US National Academies publication on preventing mental, emotional, and behavioral disorders among young people focused on recent research and program experience and stated that "A number of promotion and prevention programs are now available that should be considered for broad implementation."[115][116] A 2011 review of this by the authors said "A scientific base of evidence shows that we can prevent many mental, emotional, and behavioral disorders before they begin" and made recommendations including
- supporting the mental health and parenting skills of parents,
- encouraging the developmental competencies of children and
- using preventive strategies particularly for children at risk (such as children of parents with mental illness, or with family stresses such as divorce or job loss).[117]
In India the 1982 National Mental health Programme included prevention,[118] but implementation has been slow, particularly of prevention elements.[119][120][121]
It is already known that home visiting programs for pregnant women and parents of young children can produce replicable effects on children's general health and development in a variety of community settings.[122] Similarly positive benefits from social and emotional education are well proven.[123] Research has shown that risk assessment and behavioral interventions in pediatric clinics reduced abuse and neglect outcomes for young children.[124] Early childhood home visitation also reduced abuse and neglect, but results were inconsistent.[125]
Assessing parenting capability has been raised in child protection and other contexts.[126][127][128][129] Delaying of potential very young pregnancies could lead to better mental health causal risk factors such as improved parenting skills and more stable homes,[130] and various approaches have been used to encourage such behaviour change.[131][132] Some countries run conditional cash transfer welfare programs where payment is conditional on behaviour of the recipients. Compulsory contraception has been used to prevent future mental illness.[133]
Prevention programs can face issues in (i) ownership, because health systems are typically targeted at current suffering, and (ii) funding, because program benefits come on longer timescales than the normal political and management cycle.[134][135] Assembling collaborations of interested bodies appears to be an effective model for achieving sustained commitment and funding.[136]
Targeted vs universal programs
There has been an historical trend among public health professionals to consider targeted programmes. However identification of high risk groups can increase stigma, in turn meaning that the targeted people do not engage. Thus current policy recommends universal programs, with resources within such programs weighted towards high risk groups.[137]
Management

Treatment and support for mental disorders is provided in psychiatric hospitals, clinics or any of a diverse range of community mental health services. A number of professions have developed that specialize in the treatment of mental disorders. This includes the medical specialty of psychiatry (including psychiatric nursing),[138][139][140] the field of psychology known as clinical psychology,[141] and the practical application of sociology known as social work.[142] There is also a wide range of psychotherapists (including family therapy), counselors, and public health professionals. In addition, there are peer support roles where personal experience of similar issues is the primary source of expertise.[143][144][145][146] The different clinical and scientific perspectives draw on diverse fields of research and theory, and different disciplines may favor differing models, explanations and goals.[31]
In some countries services are increasingly based on a recovery approach, intended to support each individual's personal journey to gain the kind of life they want, although there may also be 'therapeutic pessimism' in some areas.
There are a range of different types of treatment and what is most suitable depends on the disorder and on the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived.
Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.[147]
Psychotherapy
A major option for many mental disorders is psychotherapy. There are several main types. Cognitive behavioral therapy (CBT) is widely used and is based on modifying the patterns of thought and behavior associated with a particular disorder. Psychoanalysis, addressing underlying psychic conflicts and defenses, has been a dominant school of psychotherapy and is still in use. Systemic therapy or family therapy is sometimes used, addressing a network of significant others as well as an individual.
Some psychotherapies are based on a humanistic approach. There are a number of specific therapies used for particular disorders, which may be offshoots or hybrids of the above types. Mental health professionals often employ an eclectic or integrative approach. Much may depend on the therapeutic relationship, and there may be problems with trust, confidentiality and engagement.
Medication
A major option for many mental disorders is psychiatric medication and there are several main groups. Antidepressants are used for the treatment of clinical depression, as well as often for anxiety and a range of other disorders. Anxiolytics (including sedatives) are used for anxiety disorders and related problems such as insomnia. Mood stabilizers are used primarily in bipolar disorder. Antipsychotics are used for psychotic disorders, notably for positive symptoms in schizophrenia, and also increasingly for a range of other disorders. Stimulants are commonly used, notably for ADHD.
Despite the different conventional names of the drug groups, there may be considerable overlap in the disorders for which they are actually indicated, and there may also be off-label use of medications. There can be problems with adverse effects of medication and adherence to them, and there is also criticism of pharmaceutical marketing and professional conflicts of interest.
Other
Electroconvulsive therapy (ECT) is sometimes used in severe cases when other interventions for severe intractable depression have failed. Psychosurgery is considered experimental but is advocated by certain neurologists in certain rare cases.[148][149]
Counseling (professional) and co-counseling (between peers) may be used. Psychoeducation programs may provide people with the information to understand and manage their problems. Creative therapies are sometimes used, including music therapy, art therapy or drama therapy. Lifestyle adjustments and supportive measures are often used, including peer support, self-help groups for mental health and supported housing or supported employment (including social firms). Some advocate dietary supplements.[150]
Reasonable accommodations (adjustments and supports) might be put in place to help an individual cope and succeed in environments despite potential disability related to mental health problems. This could include an emotional support animal or specifically trained psychiatric service dog.
Epidemiology
Mental disorders are common. Worldwide, more than one in three people in most countries report sufficient criteria for at least one at some point in their life.[151] In the United States 46% qualifies for a mental illness at some point.[152] An ongoing survey indicates that anxiety disorders are the most common in all but one country, followed by mood disorders in all but two countries, while substance disorders and impulse-control disorders were consistently less prevalent.[153] Rates varied by region.[154]
A review of anxiety disorder surveys in different countries found average lifetime prevalence estimates of 16.6%, with women having higher rates on average.[155] A review of mood disorder surveys in different countries found lifetime rates of 6.7% for major depressive disorder (higher in some studies, and in women) and 0.8% for Bipolar I disorder.[156]
In the United States the frequency of disorder is: anxiety disorder (28.8%), mood disorder (20.8%), impulse-control disorder (24.8%) or substance use disorder (14.6%).[152][157][158]
A 2004 cross-Europe study found that approximately one in four people reported meeting criteria at some point in their life for at least one of the DSM-IV disorders assessed, which included mood disorders (13.9%), anxiety disorders (13.6%) or alcohol disorder (5.2%). Approximately one in ten met criteria within a 12-month period. Women and younger people of either gender showed more cases of disorder.[159] A 2005 review of surveys in 16 European countries found that 27% of adult Europeans are affected by at least one mental disorder in a 12-month period.[160]
An international review of studies on the prevalence of schizophrenia found an average (median) figure of 0.4% for lifetime prevalence; it was consistently lower in poorer countries.[161]
Studies of the prevalence of personality disorders (PDs) have been fewer and smaller-scale, but one broad Norwegian survey found a five-year prevalence of almost 1 in 7 (13.4%). Rates for specific disorders ranged from 0.8% to 2.8%, differing across countries, and by gender, educational level and other factors.[162] A US survey that incidentally screened for personality disorder found a rate of 14.79%.[163]
Approximately 7% of a preschool pediatric sample were given a psychiatric diagnosis in one clinical study, and approximately 10% of 1- and 2-year-olds receiving developmental screening have been assessed as having significant emotional/behavioral problems based on parent and pediatrician reports.[164]
While rates of psychological disorders are often the same for men and women, women tend to have a higher rate of depression. Each year 73 million women are affected by major depression, and suicide is ranked 7th as the cause of death for women between the ages of 20–59. Depressive disorders account for close to 41.9% of the disability from neuropsychiatric disorders among women compared to 29.3% among men.[165]
History
Ancient civilizations
Ancient civilizations described and treated a number of mental disorders. The Greeks coined terms for melancholy, hysteria and phobia and developed the humorism theory. Mental disorders were described, and treatments developed, in Persia, Arabia and in the medieval Islamic world.
Europe
Middle Ages
Conceptions of madness in the Middle Ages in Christian Europe were a mixture of the divine, diabolical, magical and humoral, as well as more down to earth considerations. In the early modern period, some people with mental disorders may have been victims of the witch-hunts but were increasingly admitted to local workhouses and jails or sometimes to private madhouses. Many terms for mental disorder that found their way into everyday use first became popular in the 16th and 17th centuries.
Eighteenth century
By the end of the 17th century and into the Enlightenment, madness was increasingly seen as an organic physical phenomenon with no connection to the soul or moral responsibility. Asylum care was often harsh and treated people like wild animals, but towards the end of the 18th century a moral treatment movement gradually developed. Clear descriptions of some syndromes may be rare prior to the 19th century.
Nineteenth century
Industrialization and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the 19th century. Numerous different classification schemes and diagnostic terms were developed by different authorities, and the term psychiatry was coined (1808), though medical superintendents were still known as alienists.
Twentieth century
The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums renamed as hospitals.
Europe and the U.S.
Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first Diagnostic and Statistical Manual of Mental Disorders (DSM). The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomies and the "neuroleptic" chlorpromazine came to be used by mid-century. In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioural psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in Science by Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.[166]
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The DSM and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
Society and culture
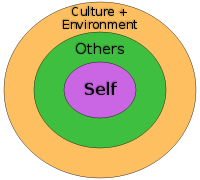
Different societies or cultures, even different individuals in a subculture, can disagree as to what constitutes optimal versus pathological biological and psychological functioning. Research has demonstrated that cultures vary in the relative importance placed on, for example, happiness, autonomy, or social relationships for pleasure. Likewise, the fact that a behavior pattern is valued, accepted, encouraged, or even statistically normative in a culture does not necessarily mean that it is conducive to optimal psychological functioning.
People in all cultures find some behaviors bizarre or even incomprehensible. But just what they feel is bizarre or incomprehensible is ambiguous and subjective.[167] These differences in determination can become highly contentious. The process by which conditions and difficulties come to be defined and treated as medical conditions and problems, and thus come under the authority of doctors and other health professionals, is known as medicalization or pathologization.
Religion
Religious, spiritual, or transpersonal experiences and beliefs meet many criteria of delusional or psychotic disorders.[168][169] A belief or experience can sometimes be shown to produce distress or disability—the ordinary standard for judging mental disorders.[170] There is a link between religion and schizophrenia,[171] a complex mental disorder characterized by a difficulty in recognizing reality, regulating emotional responses, and thinking in a clear and logical manner. Those with schizophrenia commonly report some type of religious delusion,[171][172][173] and religion itself may be a trigger for schizophrenia.[174]
Movements

Controversy has often surrounded psychiatry, and the term anti-psychiatry was coined by psychiatrist David Cooper in 1967. The anti-psychiatry message is that psychiatric treatments are ultimately more damaging than helpful to patients, and psychiatry's history involves what may now be seen as dangerous treatments.[175] Electroconvulsive therapy was one of these, which was used widely between the 1930s and 1960s. Lobotomy was another practice that was ultimately seen as too invasive and brutal. Diazepam and other sedatives were sometimes over-prescribed, which led to an epidemic of dependence. There was also concern about the large increase in prescribing psychiatric drugs for children. Some charismatic psychiatrists came to personify the movement against psychiatry. The most influential of these was R.D. Laing who wrote a series of best-selling books, including The Divided Self. Thomas Szasz wrote The Myth of Mental Illness. Some ex-patient groups have become militantly anti-psychiatric, often referring to themselves as "survivors".[175] Giorgio Antonucci has questioned the basis of psychiatry through his work on the dismantling of two psychiatric hospitals (in the city of Imola), carried out from 1973 to 1996.
The consumer/survivor movement (also known as user/survivor movement) is made up of individuals (and organizations representing them) who are clients of mental health services or who consider themselves survivors of psychiatric interventions. Activists campaign for improved mental health services and for more involvement and empowerment within mental health services, policies and wider society.[176][177][178] Patient advocacy organizations have expanded with increasing deinstitutionalization in developed countries, working to challenge the stereotypes, stigma and exclusion associated with psychiatric conditions. There is also a carers rights movement of people who help and support people with mental health conditions, who may be relatives, and who often work in difficult and time-consuming circumstances with little acknowledgement and without pay. An anti-psychiatry movement fundamentally challenges mainstream psychiatric theory and practice, including in some cases asserting that psychiatric concepts and diagnoses of 'mental illness' are neither real nor useful.[179][180][181]
Alternatively, a movement for global mental health has emerged, defined as 'the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide'.[182]
Cultural bias
Current diagnostic guidelines, namely the DSM and to some extent the ICD, have been criticized as having a fundamentally Euro-American outlook. Opponents argue that even when diagnostic criteria are used across different cultures, it does not mean that the underlying constructs have validity within those cultures, as even reliable application can prove only consistency, not legitimacy.[183] Advocating a more culturally sensitive approach, critics such as Carl Bell and Marcello Maviglia contend that the cultural and ethnic diversity of individuals is often discounted by researchers and service providers.[184]
Cross-cultural psychiatrist Arthur Kleinman contends that the Western bias is ironically illustrated in the introduction of cultural factors to the DSM-IV. Disorders or concepts from non-Western or non-mainstream cultures are described as "culture-bound", whereas standard psychiatric diagnoses are given no cultural qualification whatsoever, revealing to Kleinman an underlying assumption that Western cultural phenomena are universal.[185] Kleinman's negative view towards the culture-bound syndrome is largely shared by other cross-cultural critics. Common responses included both disappointment over the large number of documented non-Western mental disorders still left out and frustration that even those included are often misinterpreted or misrepresented.[186]
Many mainstream psychiatrists are dissatisfied with the new culture-bound diagnoses, although for partly different reasons. Robert Spitzer, a lead architect of the DSM-III, has argued that adding cultural formulations was an attempt to appease cultural critics, and has stated that they lack any scientific rationale or support. Spitzer also posits that the new culture-bound diagnoses are rarely used, maintaining that the standard diagnoses apply regardless of the culture involved. In general, mainstream psychiatric opinion remains that if a diagnostic category is valid, cross-cultural factors are either irrelevant or are significant only to specific symptom presentations.[183]
Clinical conceptions of mental illness also overlap with personal and cultural values in the domain of morality, so much so that it is sometimes argued that separating the two is impossible without fundamentally redefining the essence of being a particular person in a society.[187] In clinical psychiatry, persistent distress and disability indicate an internal disorder requiring treatment; but in another context, that same distress and disability can be seen as an indicator of emotional struggle and the need to address social and structural problems.[188][189] This dichotomy has led some academics and clinicians to advocate a postmodernist conceptualization of mental distress and well-being.[190][191]
Such approaches, along with cross-cultural and "heretical" psychologies centered on alternative cultural and ethnic and race-based identities and experiences, stand in contrast to the mainstream psychiatric community's alleged avoidance of any explicit involvement with either morality or culture.[192] In many countries there are attempts to challenge perceived prejudice against minority groups, including alleged institutional racism within psychiatric services.[193] There are also ongoing attempts to improve professional cross cultural sensitivity.
Laws and policies
Three quarters of countries around the world have mental health legislation. Compulsory admission to mental health facilities (also known as involuntary commitment) is a controversial topic. It can impinge on personal liberty and the right to choose, and carry the risk of abuse for political, social and other reasons; yet it can potentially prevent harm to self and others, and assist some people in attaining their right to healthcare when they may be unable to decide in their own interests.[194]
All human rights oriented mental health laws require proof of the presence of a mental disorder as defined by internationally accepted standards, but the type and severity of disorder that counts can vary in different jurisdictions. The two most often utilized grounds for involuntary admission are said to be serious likelihood of immediate or imminent danger to self or others, and the need for treatment. Applications for someone to be involuntarily admitted usually come from a mental health practitioner, a family member, a close relative, or a guardian. Human-rights-oriented laws usually stipulate that independent medical practitioners or other accredited mental health practitioners must examine the patient separately and that there should be regular, time-bound review by an independent review body.[194] The individual should also have personal access to independent advocacy.
In order for involuntary treatment to be administered (by force if necessary), it should be shown that an individual lacks the mental capacity for informed consent (i.e. to understand treatment information and its implications, and therefore be able to make an informed choice to either accept or refuse). Legal challenges in some areas have resulted in supreme court decisions that a person does not have to agree with a psychiatrist's characterization of the issues as constituting an "illness", nor agree with a psychiatrist's conviction in medication, but only recognize the issues and the information about treatment options.[195]
Proxy consent (also known as surrogate or substituted decision-making) may be transferred to a personal representative, a family member or a legally appointed guardian. Moreover, patients may be able to make, when they are considered well, an advance directive stipulating how they wish to be treated should they be deemed to lack mental capacity in future.[194] The right to supported decision-making, where a person is helped to understand and choose treatment options before they can be declared to lack capacity, may also be included in legislation.[196] There should at the very least be shared decision-making as far as possible. Involuntary treatment laws are increasingly extended to those living in the community, for example outpatient commitment laws (known by different names) are used in New Zealand, Australia, the United Kingdom and most of the United States.
The World Health Organization reports that in many instances national mental health legislation takes away the rights of persons with mental disorders rather than protecting rights, and is often outdated.[194] In 1991, the United Nations adopted the Principles for the Protection of Persons with Mental Illness and the Improvement of Mental Health Care, which established minimum human rights standards of practice in the mental health field. In 2006, the UN formally agreed the Convention on the Rights of Persons with Disabilities to protect and enhance the rights and opportunities of disabled people, including those with psychosocial disabilities.[197]
The term insanity, sometimes used colloquially as a synonym for mental illness, is often used technically as a legal term. The insanity defense may be used in a legal trial (known as the mental disorder defence in some countries).
Perception and discrimination
Stigma
The social stigma associated with mental disorders is a widespread problem. The US Surgeon General stated in 1999 that: "Powerful and pervasive, stigma prevents people from acknowledging their own mental health problems, much less disclosing them to others."[198] Employment discrimination is reported to play a significant part in the high rate of unemployment among those with a diagnosis of mental illness.[199] An Australian study found that having a mental illness is a bigger barrier to employment than a physical disability.[200]
Efforts are being undertaken worldwide to eliminate the stigma of mental illness,[201] although the methods and outcomes used have sometimes been criticized.[202]
A 2008 study by Baylor University researchers found that clergy in the US often deny or dismiss the existence of a mental illness. Of 293 Christian church members, more than 32 percent were told by their church pastor that they or their loved one did not really have a mental illness, and that the cause of their problem was solely spiritual in nature, such as a personal sin, lack of faith or demonic involvement. The researchers also found that women were more likely than men to get this response. All participants in both studies were previously diagnosed by a licensed mental health provider as having a serious mental illness.[203] However, there is also research suggesting that people are often helped by extended families and supportive religious leaders who listen with kindness and respect, which can often contrast with usual practice in psychiatric diagnosis and medication.[204]
The mentally ill are stigmatized in Chinese society and can not legally marry.[205] Recently more studies are being conducted to show how being stigmatized effects the care and treatment mental health patients receive. Participatory action research is a method now being used to help understand how young people in particular are being effected by their diagnosis. One study conducted by, School of Health and Human Sciences, University of Essex showed that males and females had a hard time telling their friends about their recent diagnosis and felt alienated. Most of them, however felt that the experience allowed them to open their minds to the idea of needing mental help.[206]
Doctors and therapist also play a role in helping patients to learn to cope with the possibility of being stigmatized. In order to improve their quality of life the people involved in the patient's care must make them aware that stigmas may arise and prepare them for the reality of being diagnosed with a serious mental illness. Yet another study was conducted in which 101 participants diagnosed with a serious mental illness were monitored for a year, some patients were socialized with the intent to teach them about stigmas and how to cope and others were not. The results showed that those participants that were socialized fared better in daily activities such as work and school and they also responded to treatment better than those who were not exposed to the socialization.[207] Based on the most recent research from 2012–2013, children and adolescents have been widely reporting to face problems with peer relationships due to the diagnosis of a mental illness. They face isolation and ridicule from peers. Stereotypes that are associated with their diagnosis also do not go unnoticed, many of them face bullying simply due to the fact that they have ADHD or depression. This hinders their chance for a fast recovery and may even prevent them from seeking further treatment.[208]
Media and general public
Media coverage of mental illness comprises predominantly negative and pejorative depictions, for example, of incompetence, violence or criminality, with far less coverage of positive issues such as accomplishments or human rights issues.[209][210][211] Such negative depictions, including in children's cartoons, are thought to contribute to stigma and negative attitudes in the public and in those with mental health problems themselves, although more sensitive or serious cinematic portrayals have increased in prevalence.[212][213]
In the United States, the Carter Center has created fellowships for journalists in South Africa, the U.S., and Romania, to enable reporters to research and write stories on mental health topics.[214] Former US First Lady Rosalynn Carter began the fellowships not only to train reporters in how to sensitively and accurately discuss mental health and mental illness, but also to increase the number of stories on these topics in the news media.[215][216] There is also a World Mental Health Day, which in the US and Canada falls within a Mental Illness Awareness Week.
The general public have been found to hold a strong stereotype of dangerousness and desire for social distance from individuals described as mentally ill.[217] A US national survey found that a higher percentage of people rate individuals described as displaying the characteristics of a mental disorder as "likely to do something violent to others", compared to the percentage of people who are rating individuals described as being "troubled".[218]
Recent depictions in media have included leading characters successfully living with and managing a mental illness, including in bipolar disorder in Homeland (2011) and posttraumatic stress disorder in Iron Man 3 (2013).
Violence
Despite public or media opinion, national studies have indicated that severe mental illness does not independently predict future violent behavior, on average, and is not a leading cause of violence in society. There is a statistical association with various factors that do relate to violence (in anyone), such as substance abuse and various personal, social and economic factors.[219] A 2015 review found that in the United States, about 4% of violence is attributable to people diagnosed with mental illness,[220] and a 2014 study found that 7.5% of crimes committed by mentally ill people were directly related to the symptoms of their mental illness.[221] The majority of people with serious mental illness are never violent.[222]
In fact, findings consistently indicate that it is many times more likely that people diagnosed with a serious mental illness living in the community will be the victims rather than the perpetrators of violence.[223][224] In a study of individuals diagnosed with "severe mental illness" living in a US inner-city area, a quarter were found to have been victims of at least one violent crime over the course of a year, a proportion eleven times higher than the inner-city average, and higher in every category of crime including violent assaults and theft.[225] People with a diagnosis may find it more difficult to secure prosecutions, however, due in part to prejudice and being seen as less credible.[226]
However, there are some specific diagnoses, such as childhood conduct disorder or adult antisocial personality disorder or psychopathy, which are defined by, or are inherently associated with, conduct problems and violence. There are conflicting findings about the extent to which certain specific symptoms, notably some kinds of psychosis (hallucinations or delusions) that can occur in disorders such as schizophrenia, delusional disorder or mood disorder, are linked to an increased risk of serious violence on average. The mediating factors of violent acts, however, are most consistently found to be mainly socio-demographic and socio-economic factors such as being young, male, of lower socioeconomic status and, in particular, substance abuse (including alcoholism) to which some people may be particularly vulnerable.[31][223][227][228]
High-profile cases have led to fears that serious crimes, such as homicide, have increased due to deinstitutionalization, but the evidence does not support this conclusion.[228][229] Violence that does occur in relation to mental disorder (against the mentally ill or by the mentally ill) typically occurs in the context of complex social interactions, often in a family setting rather than between strangers.[230] It is also an issue in health care settings[231] and the wider community.[232]
Mental health
The recognition and understanding of mental health conditions have changed over time and across cultures and there are still variations in definition, assessment and classification, although standard guideline criteria are widely used. In many cases, there appears to be a continuum between mental health and mental illness, making diagnosis complex.[17]:39 According to the World Health Organisation (WHO), over a third of people in most countries report problems at some time in their life which meet criteria for diagnosis of one or more of the common types of mental disorder.[151] Mental health can be defined as an absence of mental disorder.
Other animals
Psychopathology in non-human primates has been studied since the mid-20th century. Over 20 behavioral patterns in captive chimpanzees have been documented as (statistically) abnormal for frequency, severity or oddness—some of which have also been observed in the wild. Captive great apes show gross behavioral abnormalities such as stereotypy of movements, self-mutilation, disturbed emotional reactions (mainly fear or aggression) towards companions, lack of species-typical communications, and generalized learned helplessness. In some cases such behaviors are hypothesized to be equivalent to symptoms associated with psychiatric disorders in humans such as depression, anxiety disorders, eating disorders and post-traumatic stress disorder. Concepts of antisocial, borderline and schizoid personality disorders have also been applied to non-human great apes.[233][234]
The risk of anthropomorphism is often raised with regard to such comparisons, and assessment of non-human animals cannot incorporate evidence from linguistic communication. However, available evidence may range from nonverbal behaviors—including physiological responses and homologous facial displays and acoustic utterances—to neurochemical studies. It is pointed out that human psychiatric classification is often based on statistical description and judgment of behaviors (especially when speech or language is impaired) and that the use of verbal self-report is itself problematic and unreliable.[233][235]
Psychopathology has generally been traced, at least in captivity, to adverse rearing conditions such as early separation of infants from mothers; early sensory deprivation; and extended periods of social isolation. Studies have also indicated individual variation in temperament, such as sociability or impulsiveness. Particular causes of problems in captivity have included integration of strangers into existing groups and a lack of individual space, in which context some pathological behaviors have also been seen as coping mechanisms. Remedial interventions have included careful individually tailored re-socialization programs, behavior therapy, environment enrichment, and on rare occasions psychiatric drugs. Socialization has been found to work 90% of the time in disturbed chimpanzees, although restoration of functional sexuality and care-giving is often not achieved.[233][236]
Laboratory researchers sometimes try to develop animal models of human mental disorders, including by inducing or treating symptoms in animals through genetic, neurological, chemical or behavioral manipulation,[237][238] but this has been criticized on empirical grounds[239] and opposed on animal rights grounds.
Research
In 2016 the NIMH re-affirmed prevention as a research priority area.[240]
See also
- Erving Goffman
- Mental illness portrayed in media
- Mental illness in American prisons
- National Institute of Mental Health
- Psychological evaluation
- Parity of esteem
Notes
- ↑ "Mental Disorders", Medline Plus, U.S. National Library of Medicine, 15 Sep 2014, retrieved 10 Jun 2016
- 1 2 3 4 "Mental disorders Fact sheet N°396". World Health Organisation. October 2014. Retrieved 13 May 2015.
- ↑ "Mental disorders". World Health Organization. WHO. Retrieved 9 April 2016.
- ↑ American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington: American Psychiatric Publishing. pp. 101–05. ISBN 978-0890425558.
- ↑ Stein, Dan J. (December 2013). "What is a mental disorder? A perspective from cognitive-affective science" (PDF). Canadian Journal of Psychiatry. 58 (12): 656–62. PMID 24331284.
- ↑ Stein, Dan J; Phillips, K.A; Bolton, D; Fulford, K.W.M; Sadler, J.Z; Kendler, K.S (November 2010). "What is a Mental/Psychiatric Disorder? From DSM-IV to DSM-V". Psychological Medicine. London: Cambridge University Press. 40 (11): 1759–1765. doi:10.1017/S0033291709992261. ISSN 0033-2917. OCLC 01588231. PMC 3101504
 . PMID 20624327.
. PMID 20624327. In DSM-IV, each of the mental disorders is conceptualized as a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and that is associated with present distress (e.g., a painful symptom) or disability (i.e., impairment in one or more important areas of functioning) or with a significantly increased risk of suffering death, pain, disability, or an important loss of freedom. In addition, this syndrome or pattern must not be merely an expectable and culturally sanctioned response to a particular event, for example, the death of a loved one. Whatever its original cause, it must currently be considered a manifestation of a behavioral, psychological, or biological dysfunction in the individual. Neither deviant behavior (e.g., political, religious, or sexual) nor conflicts that are primarily between the individual and society are mental disorders unless the deviance or conflict is a symptom of a dysfunction in the individual, as described above.
- ↑ Stein, Dan J; Phillips, K.A; Bolton, D; Fulford, K.W.M; Sadler, J.Z; Kendler, K.S (November 2010). "What is a Mental/Psychiatric Disorder? From DSM-IV to DSM-V : Table 1 DSM-IV Definition of Mental Disorder". Psychological Medicine. London: Cambridge University Press. 40 (11): 1759–1765. doi:10.1017/S0033291709992261. ISSN 0033-2917. OCLC 01588231. PMC 3101504
 . PMID 20624327.
. PMID 20624327. - ↑ Stein, Dan J; Phillips, K.A; Bolton, D; Fulford, K.W.M; Sadler, J.Z; Kendler, K.S (November 2010). "What is a Mental/Psychiatric Disorder? From DSM-IV to DSM-V". Psychological Medicine. London: Cambridge University Press. 40 (11): 1759–1765. doi:10.1017/S0033291709992261. ISSN 0033-2917. OCLC 01588231. PMC 3101504
 . PMID 20624327.
. PMID 20624327. ... although this manual provides a classification of mental disorders, it must be admitted that no definition adequately specifies precise boundaries for the concept of ‘mental disorder.’ The concept of mental disorder, like many other concepts in medicine and science, lacks a consistent operational definition that covers all situations. All medical conditions are defined on various levels of abstraction--for example, structural pathology (e.g., ulcerative colitis), symptom presentation (e.g., migraine), deviance from a physiological norm (e.g., hypertension), and etiology (e.g., pneumococcal pneumonia). Mental disorders have also been defined by a variety of concepts (e.g., distress, dyscontrol, disadvantage, disability, inflexibility, irrationality, syndromal pattern, etiology, and statistical deviation). Each is a useful indicator for a mental disorder, but none is equivalent to the concept, and different situations call for different definitions.
- ↑ Berrios, German E. (1999). "Classifications in psychiatry: A conceptual history". Australian and New Zealand Journal of Psychiatry. 33 (2): 145–60. doi:10.1046/j.1440-1614.1999.00555.x. PMID 10336212.
- ↑ Perring, C. (2005) Mental Illness Stanford Encyclopedia of Philosophy
- ↑ Katschnig, Heinz (2010). "Are psychiatrists an endangered species? Observations on internal and external challenges to the profession". World Psychiatry. 9 (1): 21–8. doi:10.1002/j.2051-5545.2010.tb00257.x (inactive 2015-01-01). PMC 2816922
 . PMID 20148149.
. PMID 20148149. - ↑ Kato, Tadafumi (2011). "A renovation of psychiatry is needed". World Psychiatry. 10 (3): 198–9. doi:10.1002/j.2051-5545.2011.tb00056.x (inactive 2015-01-01). PMC 3188773
 . PMID 21991278.
. PMID 21991278. - ↑ Doward, Jamie (11 May 2013). "Medicine's big new battleground: does mental illness really exist?". The Guardian.
- ↑ "NIMH » Mental Disorders as Brain Disorders: Thomas Insel at TEDxCaltech". National Institute of Mental Health. U.S. Department of Health and Human Services. 23 April 2013.
- ↑ Gazzaniga, M.S., & Heatherton, T.F. (2006). Psychological Science. New York: W.W. Norton & Company, Inc.
- 1 2 3 "Mental Health: Types of Mental Illness". WebMD. 1 July 2005. Retrieved 2009-09-29.
- 1 2 Office of the Surgeon General; Center for Mental Health Services; National Institute of Mental Health (1999). "The Fundamentals of Mental Health and Mental Illness" (PDF). Mental Health: A Report of the Surgeon General. National Institute of Mental Health. pp. 26–50. ISBN 978-0-16-050300-9.
- ↑ NIMH (2005) Teacher's Guide: Information about Mental Illness and the Brain Curriculum supplement from The NIH Curriculum Supplements Series
- ↑ Phillip W. Long M.D. (1995–2008). "Disorders". Internet Mental Health. Retrieved 5 October 2009.
- ↑ Akiskal, Hagop S.; Benazzi, Franco (2006). "The DSM-IV and ICD-10 categories of recurrent \major] depressive and bipolar II disorders: Evidence that they lie on a dimensional spectrum". Journal of Affective Disorders. 92 (1): 45–54. doi:10.1016/j.jad.2005.12.035. PMID 16488021.
- ↑ Clark, Lee Anna (2007). "Assessment and Diagnosis of Personality Disorder: Perennial Issues and an Emerging Reconceptualization". Annual Review of Psychology. 58 (1): 227–57. doi:10.1146/annurev.psych.57.102904.190200. PMID 16903806.
- ↑ Morey, Leslie C.; Hopwood, Christopher J.; Gunderson, John G.; Skodol, Andrew E.; Shea, M. Tracie; Yen, Shirley; Stout, Robert L.; Zanarini, Mary C.; Grilo, Carlos M.; Sanislow, Charles A.; McGlashan, Thomas H. (2006). "Comparison of alternative models for personality disorders". Psychological Medicine. 37 (7): 983–94. doi:10.1017/S0033291706009482. PMID 17121690.
- ↑ Gamma, Alex; Angst, Jules; Ajdacic, Vladeta; Eich, Dominique; Rössler, Wulf (2006). "The spectra of neurasthenia and depression: Course, stability and transitions". European Archives of Psychiatry and Clinical Neuroscience. 257 (2): 120–7. doi:10.1007/s00406-006-0699-6. PMID 17131216.
- ↑ Trimble, Michael (2002). "Uncommon psychiatric syndromes, 4th edn". Journal of Neurology, Neurosurgery & Psychiatry. 73 (2): 211–c. doi:10.1136/jnnp.73.2.211-c. PMC 1738003
 .
. - ↑ MacSuibhne, Seamus P (2009). "What makes 'a mental illness?' What makes 'a new mental illness'?: The cases of solastalgia and hubris syndrome". Cosmos and History. 5 (2): 210–25.
- ↑ Harrison, G.; Hopper, K; Craig, T; Laska, E; Siegel, C; Wanderling, J; Dube, KC; Ganev, K; Giel, R; An Der Heiden, W; Holmberg, SK; Janca, A; Lee, PW; León, CA; Malhotra, S; Marsella, AJ; Nakane, Y; Sartorius, N; Shen, Y; Skoda, C; Thara, R; Tsirkin, SJ; Varma, VK; Walsh, D; Wiersma, D (2001). "Recovery from psychotic illness: A 15- and 25-year international follow-up study". The British Journal of Psychiatry. 178 (6): 506–17. doi:10.1192/bjp.178.6.506. PMID 11388966.
- ↑ Jobe, TH; Harrow, M (2005). "Long-term outcome of patients with schizophrenia: A review". Canadian Journal of Psychiatry. 50 (14): 892–900. PMID 16494258.
- ↑ Tohen, Mauricio; Zarate Jr, Carlos A.; Hennen, John; Khalsa, Hari-Mandir Kaur; Strakowski, Stephen M.; Gebre-Medhin, Priscilla; Salvatore, Paola; Baldessarini, Ross J. (2003). "The McLean-Harvard First-Episode Mania Study: Prediction of Recovery and First Recurrence". American Journal of Psychiatry. 160 (12): 2099–107. doi:10.1176/appi.ajp.160.12.2099. PMID 14638578.
- ↑ Judd, Lewis L.; Akiskal, HS; Schettler, PJ; Endicott, J; Leon, AC; Solomon, DA; Coryell, W; Maser, JD; Keller, MB (2005). "Psychosocial Disability in the Course of Bipolar I and II Disorders: A Prospective, Comparative, Longitudinal Study". Archives of General Psychiatry. 62 (12): 1322–30. doi:10.1001/archpsyc.62.12.1322. PMID 16330720.
- ↑ Center for Psychiatric Rehabilitation What is Psychiatric Disability and Mental Illness? Boston University, Retrieved January 2012
- 1 2 3 Pilgrim, David; Rogers, Anne (2005). A sociology of mental health and illness (3rd ed.). Milton Keynes: Open University Press. ISBN 0-335-21583-1.
- ↑ Ferney, V. (2003) The Hierarchy of Mental Illness: Which diagnosis is the least debilitating? New York City Voices Jan/March
- ↑ Ormel, Johan; Petukhova, Maria; Chatterji, Somnath; Aguilar-Gaxiola, Sergio; Alonso, Jordi; Angermeyer, Matthias C.; Bromet, Evelyn J.; Burger, Huibert; Demyttenaere, Koen; De Girolamo, G.; Haro, J. M.; Hwang, I.; Karam, E.; Kawakami, N.; Lépine, J. P.; Medina-Mora, M. E.; Posada-Villa, J.; Sampson, N.; Scott, K.; Ustün, T. B.; Von Korff, M.; Williams, D. R.; Zhang, M.; Kessler, R. C. (2008). "Disability and treatment of specific mental and physical disorders across the world". The British Journal of Psychiatry. 192 (5): 368–75. doi:10.1192/bjp.bp.107.039107. PMC 2681238
 . PMID 18450663.
. PMID 18450663. - ↑ Collins, Pamela Y.; Patel, Vikram; Joestl, Sarah S.; March, Dana; Insel, Thomas R.; Daar, Abdallah S.; Bordin, Isabel A.; Anderson, E. Jane; Dhansay, Maureen; Phillips, Christopher; Shurin, Roger I.; Walport, Wayne; Ewart, Yueqin; Savill, Steven E.; Bordin, Kay; Costello, Sylvia; Durkin, Shitij; Fairburn, Arthur; Glass, Adesola; Hall, Angel; Huang, Mu-Ming; Hyman, Vijayalakshmi; Jamison, Barbara J.; Kaaya, Shekhar; Kapur, Peter A.; Kleinman, Dan J.; Ogunniyi, Warwick; Otero-Ojeda, Muhammad A.; Poo, Wendy; Ravindranath, Anthony; Scientific Advisory Board the Executive Committee of the Grand Challenges on Global Mental Health (2011). "Grand challenges in global mental health". Nature. 475 (7354): 27–30. doi:10.1038/475027a. PMC 3173804
 . PMID 21734685.
. PMID 21734685. - ↑ Gore, Fiona M; Bloem, Paul JN; Patton, George C; Ferguson, Jane; Joseph, Véronique; Coffey, Carolyn; Sawyer, Susan M; Mathers, Colin D (2011). "Global burden of disease in young people aged 10–24 years: A systematic analysis". The Lancet. 377 (9783): 2093–102. doi:10.1016/S0140-6736(11)60512-6. PMID 21652063.
- ↑ "CIS: UN Body Takes On Rising Suicide Rates – Radio Free Europe / Radio Liberty 2006".
- ↑ O'Connor, Rory; Sheehy, Noel (29 Jan 2000). Understanding suicidal behaviour. Leicester: BPS Books. pp. 33–37. ISBN 978-1-85433-290-5.
- ↑ Bertolote, José Manoel; Fleischmann, Alexandra (2002). "Suicide and psychiatric diagnosis: A worldwide perspective". World Psychiatry. 1 (3): 181–5. PMC 1489848
 . PMID 16946849.
. PMID 16946849. - ↑ Sellers, R.; Collishaw, S.; Rice, F.; Thapar, A. K.; Potter, R.; Mars, B.; Harold, G. T.; Smith, D. J.; Owen, M. J.; Craddock, N.; Thapar, A. (2012). "Risk of psychopathology in adolescent offspring of mothers with psychopathology and recurrent depression". The British Journal of Psychiatry. 202 (2): 108–14. doi:10.1192/bjp.bp.111.104984. PMID 23060622.
- ↑ Jeronimus B.F.; Kotov, R.; Riese, H.; Ormel, J. (2016). "Neuroticism's prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants". Psychological Medicine. doi:10.1017/S0033291716001653. PMID 27523506.
- 1 2 Ormel J.; Jeronimus, B.F.; Kotov, M.; Riese, H.; Bos, E.H.; Hankin, B. (July 2013). "Neuroticism and common mental disorders: Meaning and utility of a complex relationship". Clinical Psychology Review. 33 (5): 686–697. doi:10.1016/j.cpr.2013.04.003. PMC 4382368
 . PMID 23702592.
. PMID 23702592. - ↑ Pillemer, Karl; Suitor, J. Jill; Pardo, Seth; Henderson Jr, Charles (2010). "Mothers' Differentiation and Depressive Symptoms Among Adult Children". Journal of Marriage and Family. 72 (2): 333–345. doi:10.1111/j.1741-3737.2010.00703.x. PMC 2894713
 . PMID 20607119.
. PMID 20607119. - 1 2 3 "Cannabis and mental health". Royal College of Psychiatrists. Retrieved 2013-04-23.
- 1 2 3 "The Report". The Schizophrenia Commission. 2012-11-13. Retrieved 2013-04-23.
- 1 2 Krabbendam, L., Van Os, J. (2005). "Schizophrenia and Urbanicity: A Major Environmental Influence - Conditional on Genetic Risk". Schizophrenia Bulletin. 31 (4): 795–799. doi:10.1093/schbul/sbi060.
- 1 2 3 Bienvenu, O. Joseph; Ginsburg, Golda S. (2007). "Prevention of anxiety disorders". International Review of Psychiatry. 19 (6): 647–54. doi:10.1080/09540260701797837. PMID 18092242.
- ↑ O'Connell, Mary Ellen; Boat, Thomas; Warner, Kenneth E., eds. (2009). "Table E-4 Risk Factors for Anxiety". Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective. National Academies Press. p. 530. ISBN 978-0-309-12674-8.
- ↑ Hiday, VA (June 1995). "The social context of mental illness and violence.". Journal of health and social behavior. 36 (2): 122–37. doi:10.2307/2137220. PMID 9113138.
- ↑ Miklowitz, David J.; Chang, Kiki D. (2008). "Prevention of bipolar disorder in at-risk children: Theoretical assumptions and empirical foundations". Development and Psychopathology. 20 (3): 881–97. doi:10.1017/S0954579408000424. PMC 2504732
 . PMID 18606036.
. PMID 18606036. - ↑ Fergusson, David M.; Boden, Joseph M.; Horwood, L. John (March 2009). "Tests of Causal Links Between Alcohol Abuse or Dependence and Major Depression". Archives of General Psychiatry. 66 (3): 260–266. doi:10.1001/archgenpsychiatry.2008.543. PMID 19255375.
- ↑ Winston, Anthony P.; Hardwick, Elizabeth; Jaberi, Neema (October 2005). "Neuropsychiatric effects of caffeine". Advances in Psychiatric Treatment. 11 (6): 432–9. doi:10.1192/apt.11.6.432.
- ↑ Vilarim, MM; Rocha Araujo, DM; Nardi, AE (August 2011). "Caffeine challenge test and panic disorder: a systematic literature review.". Expert review of neurotherapeutics. 11 (8): 1185–95. PMID 21797659.
- ↑ Picchioni, M. M; Murray, R. M (2007). "Schizophrenia". BMJ. 335 (7610): 91–5. doi:10.1136/bmj.39227.616447.BE. PMC 1914490
 . PMID 17626963.
. PMID 17626963. - ↑ Khan, MA; Akella, S (2009). "Cannabis-induced bipolar disorder with psychotic features: A case report". Psychiatry. 6 (12): 44–8. PMC 2811144
 . PMID 20104292.
. PMID 20104292. - ↑ American Psychiatric Association May 3, 2013 Release Number 13-33
- ↑ Kendler, K.S. (2012). "The dappled nature of causes of psychiatric illness: replacing the organic-functional/hardware-software dichotomy with empirically based pluralism". Mol Psychiatry. 17 (4): 377–88. doi:10.1038/mp.2011.182. PMC 3312951
 . PMID 22230881.
. PMID 22230881. - ↑ Kinderman, Peter; Lobban, Fiona (2000). "Evolving Formulations: Sharing Complex Information with Clients". Behavioural and Cognitive Psychotherapy. 28 (3): 307–10. doi:10.1017/S1352465800003118.
- ↑ HealthWise (2004) Mental Health Assessment. Yahoo! Health
- ↑ Davies, T. (1997). "ABC of mental health: Mental health assessment". BMJ. 314 (7093): 1536–9. doi:10.1136/bmj.314.7093.1536. PMC 2126757
 . PMID 9183204.
. PMID 9183204. - ↑ Kashner, T. M.; Rush, AJ; Surís, A; Biggs, MM; Gajewski, VL; Hooker, DJ; Shoaf, T; Altshuler, KZ (2003). "Impact of Structured Clinical Interviews on Physicians' Practices in Community Mental Health Settings". Psychiatric Services. 54 (5): 712–8. doi:10.1176/appi.ps.54.5.712. PMID 12719503.
- ↑ Shear, M. Katherine; Greeno, C; Kang, J; Ludewig, D; Frank, E; Swartz, HA; Hanekamp, M (2000). "Diagnosis of Nonpsychotic Patients in Community Clinics". American Journal of Psychiatry. 157 (4): 581–7. doi:10.1176/appi.ajp.157.4.581. PMID 10739417.
- ↑ "What is HoNOS?". Royal College of Psychiatrists.
- ↑ "Introduction to HoNOS". Royal College of Psychiatrists.
- ↑ Pirkis, Jane E; Burgess, Philip M; Kirk, Pia K; Dodson, Sarity; Coombs, Tim J; Williamson, Michelle K (November 2005). "A review of the psychometric properties of the Health of the Nation Outcome Scales (HoNOS) family of measures". Health and Quality of Life Outcomes. 3 (1): 76. doi:10.1186/1477-7525-3-76. PMC 1315350
 . PMID 16313678.
. PMID 16313678. 
- ↑ Audin, K. (June 2001). "Value of HoNOS in assessing patient change in NHS psychotherapy and psychological treatment services". The British Journal of Psychiatry. 178 (6): 561–6. doi:10.1192/bjp.178.6.561. PMID 11388975.
- ↑ Paula J. Caplan (April 28, 2012). "Psychiatry's bible, the DSM, is doing more harm than good". Washington Post.
- ↑ Frances, Allen (6 August 2013). "The New Crisis in Confidence in Psychiatric Diagnosis". Annals of Internal Medicine. 159 (3): 221–222. doi:10.7326/0003-4819-159-3-201308060-00655. PMID 23685989.
- ↑ Kirk, S. A., Gomory, T., & Cohen, D. (2013). Mad Science: Psychiatric Coercion, Diagnosis, and Drugs. Transaction Publishers. p. 185.
- ↑ Moynihan, Ray; Heath, Iona; Henry, David (13 April 2002). "Selling sickness: the pharmaceutical industry and disease mongering". BMJ. 324 (7342): 886–891. doi:10.1136/bmj.324.7342.886. PMC 1122833
 . PMID 11950740.
. PMID 11950740. - ↑ World Health Organization, Department of Mental Health and Substance Abuse; Prevention Research Centre of the Universities of Nijmegen and Maastricht (2004). Prevention of mental disorders: effective interventions and policy options: summary report (PDF). Geneva: World Health Organization. ISBN 92-4-159215-X.
- ↑ Campion, J.; Bhui, K.; Bhugra, D.; European Psychiatric, Association (2012). "European Psychiatric Association (EPA) guidance on prevention of mental disorders". European Psychiatry. 27 (2): 68–80. doi:10.1016/j.eurpsy.2011.10.004. PMID 22285092.
- ↑ "Mental health promotion and mental illness prevention: The economic case". London School of Economics and Political Science. 2 February 2011. Retrieved May 27, 2013.
- ↑ Barth, Richard P. (2009). "Preventing Child Abuse and Neglect with Parent Training: Evidence and Opportunities" (PDF). The Future of Children. 19 (2): 95–118. doi:10.1353/foc.0.0031. JSTOR 27795049. PMID 19719024.
- ↑ Stewart-Brown, Sarah L.; Schrader-Mcmillan, Anita (December 2011). "Parenting for mental health: what does the evidence say we need to do? Report of Workpackage 2 of the DataPrev project". Health Promotion International. 26 (suppl 1): i10–i28. doi:10.1093/heapro/dar056. PMID 22079931. Retrieved 2014-04-15.
- ↑ Muñoz, Ricardo F.; Cuijpers, Pim; Smit, Filip; Barrera, Alinne Z.; Leykin, Yan (2010). "Prevention of Major Depression". Annual Review of Clinical Psychology. 6: 181–212. doi:10.1146/annurev-clinpsy-033109-132040. PMID 20192789.
- ↑ Cuijpers, P. (2003). "Examining the Effects of Prevention Programs on the Incidence of New Cases of Mental Disorders: The Lack of Statistical Power". American Journal of Psychiatry. 160 (8): 1385–91. doi:10.1176/appi.ajp.160.8.1385. PMID 12900296.
- ↑ Cuijpers, Pim; Van Straten, A; Smit, F; Mihalopoulos, C; Beekman, A (2008). "Preventing the Onset of Depressive Disorders: A Meta-Analytic Review of Psychological Interventions". American Journal of Psychiatry. 165 (10): 1272–80. doi:10.1176/appi.ajp.2008.07091422. PMID 18765483.
- ↑ Muñoz, Ricardo F.; Beardslee, William R.; Leykin, Yan (2012). "Major depression can be prevented". American Psychologist. 67 (4): 285–95. doi:10.1037/a0027666. PMC 4533896
 . PMID 22583342.
. PMID 22583342. - ↑ Cuijpers, Pim; Muñoz, Ricardo F.; Clarke, Gregory N.; Lewinsohn, Peter M. (2009). "Psychoeducational treatment and prevention of depression: The "coping with depression" course thirty years later". Clinical Psychology Review. 29 (5): 449–58. doi:10.1016/j.cpr.2009.04.005. PMID 19450912.
- ↑ Smit, Filip; Ederveen, A; Cuijpers, P; Deeg, D; Beekman, A (2006). "Opportunities for Cost-effective Prevention of Late-Life Depression: An Epidemiological Approach". Archives of General Psychiatry. 63 (3): 290–6. doi:10.1001/archpsyc.63.3.290. PMID 16520434.
- ↑ Muñoz, RF; Bunge, EL (27 January 2016). "Prevention of depression worldwide: a wake-up call.". The lancet. Psychiatry. 3: 306–7. doi:10.1016/S2215-0366(15)00555-6. PMID 26827251.
- ↑ Seligman, Martin E. P.; Schulman, Peter; Derubeis, Robert J.; Hollon, Steven D. (1999). "The prevention of depression and anxiety". Prevention & Treatment. 2 (1). doi:10.1037/1522-3736.2.1.28a.
- ↑ Gardenswartz, Cara Ann; Craske, Michelle G. (2001). "Prevention of panic disorder". Behavior Therapy. 32 (4): 725–37. doi:10.1016/S0005-7894(01)80017-4.
- ↑ Van't Veer-Tazelaar, Petronella J.; Van Marwijk, HW; Van Oppen, P; Van Hout, HP; Van Der Horst, HE; Cuijpers, P; Smit, F; Beekman, AT (2009). "Stepped-Care Prevention of Anxiety and Depression in Late Life: A Randomized Controlled Trial". Archives of General Psychiatry. 66 (3): 297–304. doi:10.1001/archgenpsychiatry.2008.555. PMID 19255379.
- ↑ "CBT lessons in school reduce anxiety in children". University of Bath. 16 July 2014. Retrieved 18 July 2014.
- ↑ Neil, AL; Christensen, H (April 2009). "Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety.". Clinical Psychology Review. 29 (3): 208–15. doi:10.1016/j.cpr.2009.01.002. PMID 19232805.
- ↑ Stafford, M. R.; Jackson, H.; Mayo-Wilson, E.; Morrison, A. P.; Kendall, T. (2013). "Early interventions to prevent psychosis: Systematic review and meta-analysis". BMJ. 346: f185. doi:10.1136/bmj.f185. PMC 3548617
 . PMID 23335473.
. PMID 23335473. - ↑ http://schizophreniabulletin.oxfordjournals.org/content/early/2016/06/15/schbul.sbw084.abstract
- 1 2 "Psychosis and schizophrenia in adults: updated NICE guidance for 2014". National Elf Service.
- ↑ "Psychosis and schizophrenia". nice.org.uk.
- ↑ Marshall, M; Rathbone, J (15 June 2011). "Early intervention for psychosis.". The Cochrane database of systematic reviews (6): CD004718. doi:10.1002/14651858.CD004718.pub3. PMC 4163966
 . PMID 21678345.
. PMID 21678345. - ↑ Hutton, P.; Taylor, P. J. (2013). "Cognitive behavioural therapy for psychosis prevention: A systematic review and meta-analysis". Psychological Medicine. 44: 1–20. doi:10.1017/S0033291713000354. PMID 23521867.
- ↑ Stafford, M. R.; Jackson, H.; Mayo-Wilson, E.; Morrison, A. P.; Kendall, T. (2013). "Early interventions to prevent psychosis: Systematic review and meta-analysis". BMJ. 346: f185. doi:10.1136/bmj.f185. PMC 3548617
 . PMID 23335473.
. PMID 23335473. - ↑ McGorry, Patrick D.; Nelson, Barnaby; Phillips, Lisa J.; Yuen, Hok Pan; Francey, Shona M.; Thampi, Annette; Berger, Gregor E.; Amminger, G. Paul; et al. (2013). "Randomized Controlled Trial of Interventions for Young People at Ultra-High Risk of Psychosis". The Journal of Clinical Psychiatry. 74 (4): 349–56. doi:10.4088/JCP.12m07785. PMID 23218022.
- ↑ Butterfield, Rebecca; Henderson, John; Scott, Robert (May 2009), Public Health and Prevention Expenditure in England: Health England Report No. 4 (PDF), London: Department of Health, archived from the original (PDF) on 13 September 2009
- ↑ http://www.samhsa.gov/prevention/samhsas-efforts
- ↑ https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf
- ↑ https://www.mentalhealth.org.uk/publications/mental-health-and-prevention-taking-local-action-better-mental-health
- ↑ http://himh.clients.squiz.net/home/news-and-media/news/2015/new-prevention-framework-to-support
- ↑ http://www.mentalhealth.org.uk/content/assets/PDF/publications/prevention-review.pdf
- ↑ Wahlbeck, Kristian (February 2015). "Public mental health: the time is ripe for translation of evidence into practice.". World Psychiatry. 14 (1): 36–42. doi:10.1002/wps.20178. PMC 4329888
 . PMID 25655149.
. PMID 25655149. - ↑ "Chief Medical Officer (CMO) annual report: public mental health". www.gov.uk.
- ↑ "UK Faculty of Public Health :: Better Mental Health for All". Fph.org.uk. Retrieved 2014-04-15.
- ↑ "Our plans". Mind. Retrieved 2013-04-23.
- ↑ "Mental Health and Spiritual Health Care | Healthy Living, Seniors and Consumer Affairs | Province of Manitoba" (PDF). Gov.mb.ca. Retrieved 2013-04-23.
- ↑ National Prevention Council (16 June 2011), National Prevention Strategy: America's Plan for Better Health and Wellness (PDF), Washington, DC: Office of the Surgeon General, archived from the original (PDF) on 15 January 2013
- ↑ "Priority area 2: Prevention and early intervention" (PDF). Fourth National Mental Health Plan: An agenda for collaborative government action in mental health 2009–2014. Canberra ACT, Australia: Department of Health. 2009. pp. 31–37. ISBN 978-1-74241-075-3.
- ↑ EU High-level Conference: Together for Mental Health and Well-being (13 June 2008), European Pact for Mental Health and Well-being (PDF), Brussels: European Union
- ↑ Standing Senate Committee on Social Affairs, Science and Technology (May 2006), "Mental Health Promotion and Mental Illness Prevention", Out of the Shadows at Last: Transforming Mental Health, Mental Illness and Addiction Services in Canada, Parliament of Canada
- ↑ "Babies in Mind - Early Intervention in Sutton". Mentalhealth.org.uk. Retrieved 2014-04-15.
- ↑ "Babies In Mind, a project by Home-Start Sutton | The Big Give". Secure.thebiggive.org.uk. Retrieved 2014-04-15.
- ↑ "Preventing Depression & Anxiety - Home Page". Parenting Strategies. Retrieved 2014-04-15.
- ↑ "A new guide to help navigate the terrible teens". Beyondblue.org.au. Retrieved 2014-04-15.
- ↑ "DataPrev". Dataprevproject.net. Retrieved 2014-04-15.
- ↑ O'Connell, Mary Ellen; Boat, Thomas; Warner, Kenneth E., eds. (2009). Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective. National Academies Press. ISBN 978-0-309-12674-8.
- ↑ Saxena, S; Jané-Llopis, E; Hosman, C (2006). "Prevention of mental and behavioural disorders: Implications for policy and practice". World Psychiatry. 5 (1): 5–14. PMC 1472261
 . PMID 16757984.
. PMID 16757984. - ↑ Beardslee, W. R.; Chien, P. L.; Bell, C. C. (2011). "Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective". Psychiatric Services. 62 (3): 247–54. doi:10.1176/appi.ps.62.3.247. PMID 21363895.
- ↑ "National Mental Health Programme". National Institute of Health & Family Welfare. Archived from the original on 10 August 2014.
- ↑ "Jalna Zilla Parishad takes up fight against mental illness". The Times of India.
- ↑ National Mental Health Programme (NMHP) (PDF), New Delhi, India: Ministry of Health & Family Welfare, 23 July 2012
- ↑ Satyakam Mohapatra. "National mental health programme (nmhp)". slideshare.net.
- ↑ Olds, David L.; Sadler, Lois; Kitzman, Harriet (2007). "Programs for parents of infants and toddlers: Recent evidence from randomized trials". Journal of Child Psychology and Psychiatry. 48 (3–4): 355–91. doi:10.1111/j.1469-7610.2006.01702.x. PMID 17355402.
- ↑ Durlak, Joseph A.; Weissberg, Roger P.; Dymnicki, Allison B.; Taylor, Rebecca D.; Schellinger, Kriston B. (2011). "The Impact of Enhancing Students' Social and Emotional Learning: A Meta-Analysis of School-Based Universal Interventions". Child Development. 82 (1): 405–32. doi:10.1111/j.1467-8624.2010.01564.x. PMID 21291449.
- ↑ Dubowitz, H.; Feigelman, S.; Lane, W.; Kim, J. (2009). "Pediatric Primary Care to Help Prevent Child Maltreatment: The Safe Environment for Every Kid (SEEK) Model". Pediatrics. 123 (3): 858–64. doi:10.1542/peds.2008-1376. PMID 19255014.
- ↑ Selph, Shelley S.; Bougatsos, C; Blazina, I; Nelson, HD (2013). "Behavioral Interventions and Counseling to Prevent Child Abuse and Neglect: A Systematic Review to Update the U.S. Preventive Services Task Force Recommendation". Annals of Internal Medicine. 158 (3): 179–90. doi:10.7326/0003-4819-158-3-201302050-00590. PMID 23338775.
- ↑ Effective parenting capacity assessment: Key issues (PDF). Centre for Parenting & Research. May 2006. ISBN 0-7310-4387-1.
- ↑ "Assessing Parenting Skills and Competencies". Childwelfare.gov. Retrieved 2013-04-23.
- ↑ White, Angela (December 2005). Assessment of parenting capacity Literature review (PDF). Centre for Parenting & Research. ISBN 978-0-7310-4385-9.
- ↑ "Assessing parenting capacity". Practice Centre. Retrieved 2013-04-23.
- ↑ Morris, N M (1981). "The biological advantages and social disadvantages of teenage pregnancy". American Journal of Public Health. 71 (8): 796. doi:10.2105/AJPH.71.8.796. PMC 1620003
 . PMID 7258440.
. PMID 7258440. - ↑ "Adolescent Pregnancy Prevention Interventions – Family Home Visiting". Health.state.mn.us. Retrieved 2013-04-23.
- ↑ Harden, A.; Brunton, G.; Fletcher, A.; Oakley, A. (2009). "Teenage pregnancy and social disadvantage: Systematic review integrating controlled trials and qualitative studies". BMJ. 339: b4254. doi:10.1136/bmj.b4254. PMC 2776931
 . PMID 19910400.
. PMID 19910400. - ↑ Reilly, Philip (1991). The surgical solution: a history of involuntary sterilization in the United States. Baltimore: Johns Hopkins University Press. ISBN 978-0-8018-4096-8.
- ↑ Harris, Anthony; Mortimer, Duncan (2009). "Funding illness prevention and health promotion in Australia: A way forward". Australia and New Zealand Health Policy. 6 (1): 25. doi:10.1186/1743-8462-6-25. PMC 2780431
 . PMID 19909519.
. PMID 19909519. - ↑ Executive Office of the President: Office of Management and Budget (13 April 2011), Statement of Administration Policy: H.R. 1217 – Repeal of the Affordable Care Act's Prevention and Public Health Fund (Rep. Pitts, R-PA, and 3 cosponsors) (PDF), Washington, DC
- ↑ "National Prevention Research Initiative". Medical Research Council.
- ↑ "UK Faculty of Public Health :: Examples of interventions". Fph.org.uk. 2013-01-07. Retrieved 2014-04-15.
- ↑ Andreasen, NC (1997). "What is psychiatry?". The American Journal of Psychiatry. 154 (5): 591–3. doi:10.1176/ajp.154.5.591. PMID 9137110.
- ↑ "What is Psychiatry?". University of Melbourne. 19 August 2005. Archived from the original on August 20, 2006. Retrieved April 19, 2007.
- ↑ "Frequently Asked Questions About Psychiatry & Psychiatrists". California Psychiatric Association. 28 February 2007. Retrieved April 19, 2007.
- ↑ American Psychological Association, Division 12, http://www.apa.org/divisions/div12/aboutcp.html
- ↑ Golightley, M. (2004) Social work and Mental Health Learning Matters, UK
- ↑ Goldstrom, Ingrid D.; Campbell, Jean; Rogers, Joseph A.; Lambert, David B.; Blacklow, Beatrice; Henderson, Marilyn J.; Manderscheid, Ronald W. (2005). "National Estimates for Mental Health Mutual Support Groups, Self-Help Organizations, and Consumer-Operated Services". Administration and Policy in Mental Health and Mental Health Services Research. 33 (1): 92–103. doi:10.1007/s10488-005-0019-x. PMID 16240075.
- ↑ The Joseph Rowntree Foundation (1998) The experiences of mental health service users as mental health professionals
- ↑ Chamberlin, Judi (2011). "User/consumer involvement in mental health service delivery". Epidemiologia e Psichiatria Sociale. 14 (1): 10–4. doi:10.1017/S1121189X00001871. PMID 15792289.
- ↑ McCann, Terence V.; Baird, John; Clark, Eileen; Lu, Sai (2006). "Beliefs about using consumer consultants in inpatient psychiatric units". International Journal of Mental Health Nursing. 15 (4): 258–65. doi:10.1111/j.1447-0349.2006.00432.x. PMID 17064322.
- ↑ Kisely, SR; Campbell, LA (4 December 2014). "Compulsory community and involuntary outpatient treatment for people with severe mental disorders.". The Cochrane database of systematic reviews. 12: CD004408. doi:10.1002/14651858.CD004408.pub4. PMID 25474592.
- ↑ Mind Disorders Encyclopedia Psychosurgery [Retrieved on August 5th 2008]
- ↑ Mashour, George A.; Walker, Erin E.; Martuza, Robert L. (2005). "Psychosurgery: Past, present, and future". Brain Research Reviews. 48 (3): 409–19. doi:10.1016/j.brainresrev.2004.09.002. PMID 15914249.
- ↑ Lakhan, Shaheen E; Vieira, Karen F (2008). "Nutritional therapies for mental disorders". Nutrition Journal. 7 (1): 2. doi:10.1186/1475-2891-7-2. PMC 2248201
 . PMID 18208598.
. PMID 18208598. - 1 2 "Cross-national comparisons of the prevalences and correlates of mental disorders. WHO International Consortium in Psychiatric Epidemiology". Bulletin of the World Health Organization. 78 (4): 413–26. 2000. doi:10.1590/S0042-96862000000400003 (inactive 2016-11-07). PMC 2560724
 . PMID 10885160.
. PMID 10885160. - 1 2 Kessler, Ronald C.; Berglund, P; Demler, O; Jin, R; Merikangas, KR; Walters, EE (2005). "Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication". Archives of General Psychiatry. 62 (6): 593–602. doi:10.1001/archpsyc.62.6.593. PMID 15939837.
- ↑ "The World Mental Health Survey Initiative". Harvard School of Medicine. 2005.
- ↑ Demyttenaere, Koen; Bruffaerts, Ronny; Posada-Villa, Jose; Gasquet, Isabelle; Kovess, Viviane; Lepine, Jean Pierre; Angermeyer, Matthias C.; Bernert, Sebastian; De Girolamo, Giovanni; Morosini, P; Polidori, G; Kikkawa, T; Kawakami, N; Ono, Y; Takeshima, T; Uda, H; Karam, EG; Fayyad, JA; Karam, AN; Mneimneh, ZN; Medina-Mora, ME; Borges, G; Lara, C; De Graaf, R; Ormel, J; Gureje, O; Shen, Y; Huang, Y; Zhang, M; Alonso, J (2004). "Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys". JAMA. 291 (21): 2581–90. doi:10.1001/jama.291.21.2581. PMID 15173149.
- ↑ Somers, Julian M; Goldner, Elliot M; Waraich, Paul; Hsu, Lorena (2006). "Prevalence and Incidence Studies of Anxiety Disorders: A Systematic Review of the Literature". Canadian Journal of Psychiatry. 51 (2): 100–13. PMID 16989109.
- ↑ Waraich, Paul; Goldner, Elliot M; Somers, Julian M; Hsu, Lorena (2004). "Prevalence and Incidence Studies of Mood Disorders: A Systematic Review of the Literature". Canadian Journal of Psychiatry. 49 (2): 124–38. PMID 15065747.
- ↑ Kessler, Ronald C.; Chiu, WT; Demler, O; Merikangas, KR; Walters, EE (2005). "Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication". Archives of General Psychiatry. 62 (6): 617–27. doi:10.1001/archpsyc.62.6.617. PMC 2847357
 . PMID 15939839.
. PMID 15939839. - ↑ "The Numbers Count: Mental Disorders in America". National Institute of Mental Health. May 24, 2013. Archived from the original on 24 May 2013. Retrieved May 27, 2013.
- ↑ Alonso, J.; Angermeyer, M. C.; Bernert, S.; Bruffaerts, R.; Brugha, T. S.; Bryson, H.; Girolamo, G.; Graaf, R.; Demyttenaere, K.; Gasquet, I.; Haro, J. M.; Katz, S. J.; Kessler, R. C.; Kovess, V.; Lepine, J. P.; Ormel, J.; Polidori, G.; Russo, L. J.; Vilagut, G.; Almansa, J.; Arbabzadeh-Bouchez, S.; Autonell, J.; Bernal, M.; Buist-Bouwman, M. A.; Codony, M.; Domingo-Salvany, A.; Ferrer, M.; Joo, S. S.; Martinez-Alonso, M.; Matschinger, H. (2004). "Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project". Acta Psychiatrica Scandinavica. 109 (420): 21–7. doi:10.1111/j.1600-0047.2004.00327.x. PMID 15128384.
- ↑ Wittchen, Hans-Ulrich; Jacobi, Frank (2005). "Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies". European Neuropsychopharmacology. 15 (4): 357–76. doi:10.1016/j.euroneuro.2005.04.012. PMID 15961293.
- ↑ Saha, Sukanta; Chant, David; Welham, Joy; McGrath, John (2005). "A Systematic Review of the Prevalence of Schizophrenia". PLoS Medicine. 2 (5): e141. doi:10.1371/journal.pmed.0020141. PMC 1140952
 . PMID 15916472.
. PMID 15916472. - ↑ Torgersen, S.; Kringlen, E; Cramer, V (2001). "The Prevalence of Personality Disorders in a Community Sample". Archives of General Psychiatry. 58 (6): 590–6. doi:10.1001/archpsyc.58.6.590. PMID 11386989.
- ↑ Grant, Bridget F.; Hasin, Deborah S.; Stinson, Frederick S.; Dawson, Deborah A.; Chou, S. Patricia; Ruan, W. June; Pickering, Roger P. (2004). "Prevalence, Correlates, and Disability of Personality Disorders in the United States". The Journal of Clinical Psychiatry. 65 (7): 948–58. doi:10.4088/JCP.v65n0711. PMID 15291684.
- ↑ Carter, Alice S.; Briggs-Gowan, Margaret J.; Davis, Naomi Ornstein (2004). "Assessment of young children's social-emotional development and psychopathology: Recent advances and recommendations for practice". Journal of Child Psychology and Psychiatry. 45 (1): 109–34. doi:10.1046/j.0021-9630.2003.00316.x. PMID 14959805.
- ↑ "Gender disparities and mental health: The Facts". World Health Organization. Retrieved January 12, 2012.
- ↑ Kirk, Stuart A.; Kutchins, Herb (1994). "The Myth of the Reliability of DSM". Journal of Mind and Behavior. 15 (1&2).
- ↑ Heinimaa, Markus (2002). "Incomprehensibility: The role of the concept in DSM-IV definition of schizophrenic delusions". Medicine, Health Care and Philosophy. 5 (3): 291–5. doi:10.1023/A:1021164602485.
- ↑ Pierre, Joseph M. (2001). "Faith or Delusion? At the Crossroads of Religion and Psychosis". Journal of Psychiatric Practice. 7 (3): 163–72. doi:10.1097/00131746-200105000-00004. PMID 15990520.
- ↑ Johnson, C. V.; Friedman, H. L. (2008). "Enlightened or Delusional?: Differentiating Religious, Spiritual, and Transpersonal Experiences from Psychopathology". Journal of Humanistic Psychology. 48 (4): 505–27. doi:10.1177/0022167808314174.
- ↑ Clarke, Isabel (2010). Psychosis and Spirituality: Consolidating the New Paradigm. John Wiley & Sons. p. 240. ISBN 978-0-470-97029-4.
- 1 2 Siddle, Ronald; Haddock, Gillian; Tarrier, Nicholas; Faragher, E. Brian (1 March 2002). "Religious delusions in patients admitted to hospital with schizophrenia". Social Psychiatry and Psychiatric Epidemiology. 37 (3): 130–138. doi:10.1007/s001270200005. PMID 11990010.
- ↑ Mohr, Sylvia; Borras, Laurence; Betrisey, Carine; Pierre-Yves, Brandt; Gilliéron, Christiane; Huguelet, Philippe (1 June 2010). "Delusions with Religious Content in Patients with Psychosis: How They Interact with Spiritual Coping". Psychiatry: Interpersonal and Biological Processes. 73 (2): 158–172. doi:10.1521/psyc.2010.73.2.158.
- ↑ Suhail, Kausar; Ghauri, Shabnam (1 April 2010). "Phenomenology of delusions and hallucinations in schizophrenia by religious convictions". Mental Health, Religion & Culture. 13 (3): 245–259. doi:10.1080/13674670903313722.
- ↑ Mohr, Sylvia; Borras, Laurence; Rieben, Isabelle; Betrisey, Carine; Gillieron, Christiane; Brandt, Pierre-Yves; Perroud, Nader; Huguelet, Philippe (11 October 2009). "Evolution of spirituality and religiousness in chronic schizophrenia or schizo-affective disorders: a 3-years follow-up study". Social Psychiatry and Psychiatric Epidemiology. 45 (11): 1095–1103. doi:10.1007/s00127-009-0151-0.
- 1 2 Tom Burns (2006). Psychiatry:A Very Short Introduction. Oxford University Press. Retrieved 27 February 2014.
- ↑ Everett, Barbara (1994). "Something is happening: the contemporary consumer and psychiatric survivor movement in historical context". Journal of Mind and Behavior. 15 (1–2): 55–70.
- ↑ Rissmiller, David; Rissmiller, JH (2006). "Open Forum: Evolution of the Antipsychiatry Movement into Mental Health Consumerism". Psychiatric Services. 57 (6): 863–6. doi:10.1176/appi.ps.57.6.863. PMID 16754765.
- ↑ Oaks, D. (2006). "The Evolution of the Consumer Movement". Psychiatric Services. 57 (8): 1212. doi:10.1176/appi.ps.57.8.1212. PMID 16870979.
- ↑ The Antipsychiatry Coalition. (2005, November 26). The Antipsychiatry Coalition. Retrieved April 19, 2007, from antipsychiatry.org
- ↑ O'Brien, Anthony Paul; Woods, Martin; Palmer, Christine (2001). "The emancipation of nursing practice: Applying anti-psychiatry to the therapeutic community". Australian and New Zealand Journal of Mental Health Nursing. 10 (1): 3–9. doi:10.1046/j.1440-0979.2001.00183.x. PMID 11421968.
- ↑ Weitz, Don (2003). "Call Me Antipsychiatry Activist—Not 'Consumer'". Ethical Human Sciences and Services. 5 (1): 71–2. PMID 15279009. Republished from Weitz, Don (Spring 2002). "Call me Antipsychiatry Activist – not 'Consumer'". Radical Psychology. 3 (2).
- ↑ Patel, Vikram; Prince, M (2010). "Global Mental Health: A New Global Health Field Comes of Age". JAMA. 303 (19): 1976–7. doi:10.1001/jama.2010.616. PMC 3432444
 . PMID 20483977.
. PMID 20483977. - 1 2 Widiger, T. A.; Sankis, L. M. (2000). "Adult Psychopathology: Issues and Controversies". Annual Review of Psychology. 51 (1): 377–404. doi:10.1146/annurev.psych.51.1.377. PMID 10751976.
- ↑ Vedantam, Shankar (June 26, 2005). "Psychiatry's Missing Diagnosis: Patients' Diversity Is Often Discounted". The Washington Post.
- ↑ Kleinman, Arthur (1997). "Triumph or Pyrrhic Victory? The Inclusion of Culture in DSM-IV". Harvard Review of Psychiatry. 4 (6): 343–4. doi:10.3109/10673229709030563. PMID 9385013.
- ↑ Bhugra, D.; Munro, A. (1997). Troublesome Disguises: Underdiagnosed Psychiatric Syndromes. Blackwell Science.
- ↑ Clark, Lee Anna (2006). "The Role of Moral Judgment in Personality Disorder Diagnosis". Journal of Personality Disorders. 20 (2): 184–5. doi:10.1521/pedi.2006.20.2.184.
- ↑ Karasz, Alison (2005). "Cultural differences in conceptual models of depression". Social Science & Medicine. 60 (7): 1625–35. doi:10.1016/j.socscimed.2004.08.011. PMID 15652693.
- ↑ Tilbury, Farida; Rapley, Mark (2004). "'There are orphans in Africa still looking for my hands': African women refugees and the sources of emotional distress". Health Sociology Review. 13: 54–64. doi:10.5172/hesr.13.1.54.
- ↑ Bracken, P.; Thomas, P (2001). "Postpsychiatry: A new direction for mental health". BMJ. 322 (7288): 724–7. doi:10.1136/bmj.322.7288.724. PMC 1119907
 . PMID 11264215.
. PMID 11264215. - ↑ Lewis, Bradley (2000). "Psychiatry and Postmodern Theory". Journal of Medical Humanities. 21 (2): 71–84. doi:10.1023/A:1009018429802.
- ↑ Kwate, Naa Oyo A. (2005). "The Heresy of African-Centered Psychology". Journal of Medical Humanities. 26 (4): 215–35. doi:10.1007/s10912-005-7698-x. PMID 16333686.
- ↑ Patel, Kamlesh; Heginbotham, Chris (2007). "Institutional racism in mental health services does not imply racism in individual psychiatrists: Commentary on... Institutional racism in psychiatry". Psychiatric Bulletin. 31 (10): 367–8. doi:10.1192/pb.bp.107.017137.
- 1 2 3 4 WHO Resource Book on Mental Health: Human rights and legislation (PDF). World Health Organization. 2005. ISBN 92-4-156282-X.
- ↑ Sklar, Ronald (June 2007). "Starson v. Swayze: The Supreme Court Speaks Out (Not all That Clearly) on the Question of 'Capacity'" (PDF). Canadian Journal of Psychiatry. 52 (6): 390–6. PMID 17696026.
- ↑ Manitoba Family Services and Housing. The Vulnerable Persons Living with a Mental Disability Act, 1996
- ↑ ENABLE website UN section on disability
- ↑ Office of the Surgeon General; Center for Mental Health Services; National Institute of Mental Health (1999). "A Vision for the Future" (PDF). Mental Health: A Report of the Surgeon General. National Institute of Mental Health. pp. 451–8. ISBN 978-0-16-050300-9.
- ↑ Stuart, Heather (2006). "Mental illness and employment discrimination". Current Opinion in Psychiatry. 19 (5): 522–6. doi:10.1097/01.yco.0000238482.27270.5d. PMID 16874128.
- ↑ Lucas, Clay. "Stigma hurts job prospects". Sydney Morning Herald. Archived from the original on 20 January 2013. Retrieved 13 October 2012.
- ↑ "Stop Stigma". Bipolarworld-net.canadawebhosting.com. 2002-04-29. Retrieved 2013-04-23.
- ↑ Read, J.; Haslam, N.; Sayce, L.; Davies, E. (2006). "Prejudice and schizophrenia: A review of the 'mental illness is an illness like any other' approach". Acta Psychiatrica Scandinavica. 114 (5): 303–18. doi:10.1111/j.1600-0447.2006.00824.x. PMID 17022790.
- ↑ Stanford, Matthew S. (2007). "Demon or disorder: A survey of attitudes toward mental illness in the Christian church". Mental Health, Religion & Culture. 10 (5): 445–9. doi:10.1080/13674670600903049. Lay summary – Baylor University (October 14, 2008).
- ↑ Halliwell, Ed (June 22, 2009). "Psychiatric diagnoses are less reliable than star signs". The Times. Retrieved May 28, 2013. (subscription required)
- ↑ Richard Spencer (21 August 2003). "China relaxes laws on love and marriage". The Telegraph. Retrieved 24 October 2013.
- ↑ Aggart, D., Franks, W., Osborne, O., & Collins, S. (2013). 'We are the ones asking the questions': The experiences of young mental health service users conducting research into stigma. Educational & Child Psychology, 30(1), 61–71.
- ↑ Chronister, J., Chou, C., & Liao, H. (2013). THE ROLE OF STIGMA COPING AND SOCIAL SUPPORT IN MEDIATING THE EFFECT OF SOCIETAL STIGMA ON INTERNALIZED STIGMA, MENTAL HEALTH RECOVERY, AND QUALITY OF LIFE AMONG PEOPLE WITH SERIOUS MENTAL ILLNESS. Journal Of Community Psychology, 41(5), 582–600. doi:10.1002/jcop.21558
- ↑ O'driscoll, C., Heary, C., Hennessy, E., & Mckeague, L. (2012). Explicit and implicit stigma towards peers with mental health problems in childhood and adolescence. Journal Of Child Psychology & Psychiatry, 53(10), 1054–1062. doi:10.1111/j.1469-7610.2012.02580.x
- ↑ Coverdale, John; Nairn, Raymond; Claasen, Donna (2002). "Depictions of mental illness in print media: A prospective national sample". Australian and New Zealand Journal of Psychiatry. 36 (5): 697–700. doi:10.1046/j.1440-1614.2002.00998.x. PMID 12225457.
- ↑ Edney, RD. (2004) Mass Media and Mental Illness: A Literature Review Canadian Mental Health Association
- ↑ Diefenbach, Donald L. (1997). "The portrayal of mental illness on prime-time television". Journal of Community Psychology. 25 (3): 289–302. doi:10.1002/(SICI)1520-6629(199705)25:3<289::AID-JCOP5>3.0.CO;2-R.
- ↑ Sieff, Elaine (2003). "Media frames of mental illnesses: The potential impact of negative frames". Journal of Mental Health. 12 (3): 259–69. doi:10.1080/0963823031000118249.
- ↑ Wahl, Otto F. (2003). "News Media Portrayal of Mental Illness: Implications for Public Policy". American Behavioral Scientist. 46 (12): 1594–600. doi:10.1177/0002764203254615.
- ↑ "The Carter Center Awards 2008–2009 Rosalynn Carter Fellowships for Mental Health Journalism" (Press release). The Carter Center. July 18, 2008. Retrieved May 28, 2013.
- ↑ "The Rosalynn Carter Fellowships For Mental Health Journalism". The Carter Center. 2013. Retrieved May 28, 2013.
- ↑ The Carter Center. "Rosalynn Carter's Advocacy in Mental Health". Retrieved May 28, 2013.
- ↑ Link, Bruce G.; Phelan, Jo C.; Bresnahan, Michaeline; Stueve, Ann; Pescosolido, Bernice A. (1999). "Public conceptions of mental illness: Labels, causes, dangerousness, and social distance". American Journal of Public Health. 89 (9): 1328–33. doi:10.2105/AJPH.89.9.1328. PMC 1508784
 . PMID 10474548.
. PMID 10474548. - ↑ Pescosolido, Bernice A.; Monahan, John; Link, Bruce G.; Stueve, Ann; Kikuzawa, Saeko (1999). "The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems". American Journal of Public Health. 89 (9): 1339–45. doi:10.2105/AJPH.89.9.1339. PMC 1508769
 . PMID 10474550.
. PMID 10474550. - ↑ Elbogen, Eric B.; Johnson, SC (2009). "The Intricate Link Between Violence and Mental Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions". Archives of General Psychiatry. 66 (2): 152–61. doi:10.1001/archgenpsychiatry.2008.537. PMID 19188537.
- ↑ Metzl, Jonathan M.; MacLeish, Kenneth T. (February 2015). "Mental Illness, Mass Shootings, and the Politics of American Firearms". American Journal of Public Health. 105 (2): 240–249. doi:10.2105/AJPH.2014.302242.
- ↑ Peterson, Jillian K.; Skeem, Jennifer; Kennealy, Patrick; Bray, Beth; Zvonkovic, Andrea (2014). "How often and how consistently do symptoms directly precede criminal behavior among offenders with mental illness?". Law and Human Behavior. 38 (5): 439–449. doi:10.1037/lhb0000075.
- ↑ Swanson, JW; McGinty, EE; Fazel, S; Mays, VM (May 2015). "Mental illness and reduction of gun violence and suicide: bringing epidemiologic research to policy.". Annals of Epidemiology. 25 (5): 366–76. doi:10.1016/j.annepidem.2014.03.004. PMC 4211925
 . PMID 24861430.
. PMID 24861430. - 1 2 Stuart H (June 2003). "Violence and mental illness: an overview". World Psychiatry. 2 (2): 121–124. PMC 1525086
 . PMID 16946914.
. PMID 16946914. - ↑ Brekke, John S.; Prindle, C; Bae, SW; Long, JD (2001). "Risks for Individuals with Schizophrenia Who Are Living in the Community". Psychiatric Services. 52 (10): 1358–66. doi:10.1176/appi.ps.52.10.1358. PMID 11585953.
- ↑ Teplin, Linda A.; McClelland, GM; Abram, KM; Weiner, DA (2005). "Crime Victimization in Adults with Severe Mental Illness: Comparison with the National Crime Victimization Survey". Archives of General Psychiatry. 62 (8): 911–21. doi:10.1001/archpsyc.62.8.911. PMC 1389236
 . PMID 16061769.
. PMID 16061769. - ↑ Petersilia, J. R. (2001). "Crime Victims with Developmental Disabilities: A Review Essay". Criminal Justice and Behavior. 28 (6): 655–94. doi:10.1177/009385480102800601.
- ↑ Steadman, H. J.; Mulvey, EP; Monahan, J; Robbins, PC; Appelbaum, PS; Grisso, T; Roth, LH; Silver, E (1998). "Violence by People Discharged from Acute Psychiatric Inpatient Facilities and by Others in the Same Neighborhoods". Archives of General Psychiatry. 55 (5): 393–401. doi:10.1001/archpsyc.55.5.393. PMID 9596041.
- 1 2 Fazel, Seena; Gulati, Gautam; Linsell, Louise; Geddes, John R.; Grann, Martin (2009). McGrath, John, ed. "Schizophrenia and Violence: Systematic Review and Meta-Analysis". PLoS Medicine. 6 (8): e1000120. doi:10.1371/journal.pmed.1000120. PMC 2718581
 . PMID 19668362.
. PMID 19668362. - ↑ Taylor, P. J.; Gunn, J. (1999). "Homicides by people with mental illness: Myth and reality". The British Journal of Psychiatry. 174 (1): 9–14. doi:10.1192/bjp.174.1.9. PMID 10211145.
- ↑ Solomon, P. L.; Cavanaugh, MM; Gelles, RJ (2005). "Family Violence among Adults with Severe Mental Illness: A Neglected Area of Research". Trauma, Violence, & Abuse. 6 (1): 40–54. doi:10.1177/1524838004272464. PMID 15574672.
- ↑ Chou, Kuei-Ru; Lu, Ru-Band; Chang, Min (2001). "Assaultive Behavior by Psychiatric In-Patients and Its Related Factors". Journal of Nursing Research. 9 (5): 139–51. doi:10.1097/01.JNR.0000347572.60800.00. PMID 11779087.
- ↑ Logdberg, B.; Nilsson, L.-L.; Levander, M. T.; Levander, S. (2004). "Schizophrenia, neighbourhood, and crime". Acta Psychiatrica Scandinavica. 110 (2): 92–7. doi:10.1111/j.1600-0047.2004.00322.x. PMID 15233709.
- 1 2 3 Brune, M; Brunecohrs, U; McGrew, W; Preuschoft, S (2006). "Psychopathology in great apes: Concepts, treatment options and possible homologies to human psychiatric disorders". Neuroscience & Biobehavioral Reviews. 30 (8): 1246–59. doi:10.1016/j.neubiorev.2006.09.002. PMID 17141312.
- ↑ Ferdowsian, Hope R.; Durham, Debra L.; Kimwele, Charles; Kranendonk, Godelieve; Otali, Emily; Akugizibwe, Timothy; Mulcahy, J. B.; Ajarova, Lilly; Johnson, Cassie Meré (2011). Callaerts, Patrick, ed. "Signs of Mood and Anxiety Disorders in Chimpanzees". PLoS ONE. 6 (6): e19855. Bibcode:2011PLoSO...619855F. doi:10.1371/journal.pone.0019855. PMC 3116818
 . PMID 21698223.
. PMID 21698223. - ↑ Fabregajr, H (2006). "Making sense of behavioral irregularities of great apes". Neuroscience & Biobehavioral Reviews. 30 (8): 1260–73; discussion 1274–7. doi:10.1016/j.neubiorev.2006.09.004. PMID 17079015.
- ↑ Lilienfeld, Scott O.; Gershon, Jonathan; Duke, Marshall; Marino, Lori; De Waal, Frans B. M. (1999). "A preliminary investigation of the construct of psychopathic personality (psychopathy) in chimpanzees (Pan troglodytes)". Journal of Comparative Psychology. 113 (4): 365–75. doi:10.1037/0735-7036.113.4.365. PMID 10608560.
- ↑ Moran M (June 20, 2003). "Animals Can Model Psychiatric Symptoms". Psychiatric News. 38 (12): 20–30. doi:10.1176/pn.38.12.0020.
- ↑ Sánchez, M. MAR; Ladd, Charlotte O.; Plotsky, Paul M. (2001). "Early adverse experience as a developmental risk factor for later psychopathology: Evidence from rodent and primate models". Development and Psychopathology. 13 (3): 419–49. doi:10.1017/S0954579401003029. PMID 11523842.
- ↑ Matthews, Keith; Christmas, David; Swan, John; Sorrell, Eleanor (2005). "Animal models of depression: Navigating through the clinical fog". Neuroscience & Biobehavioral Reviews. 29 (4–5): 503–13. doi:10.1016/j.neubiorev.2005.03.005. PMID 15925695.
- ↑ https://www.nimh.nih.gov/about/strategic-planning-reports/strategic-research-priorities/srp-objective-3/index.shtml
Further reading
- Atkinson, J. (2006) Private and Public Protection: Civil Mental Health Legislation, Edinburgh, Dunedin Academic Press ISBN 1-903765-61-7
- Hockenbury, Don and Sandy (2004). Discovering Psychology. Worth Publishers. ISBN 0-7167-5704-4.
- Fried, Yehuda; Joseph Agassi, (1976). Paranoia: A Study in Diagnosis. Boston Studies in the Philosophy of Science, 50. ISBN 90-277-0704-9.
- Fried, Yehuda; Joseph Agassi, (1983). Psychiatry as Medicine. The Hague, Nijhoff. ISBN 90-247-2837-1.
- National Academies of Sciences, Engineering, and Medicine (2016). Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. Washington, DC: National Academies Press. ISBN 978-0-309-43912-1. doi:10.17226/23442

- Porter, Roy (2002). Madness: a brief history. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-280266-6.
- Weller M.P.I. and Eysenck M. The Scientific Basis of Psychiatry, W.B. Saunders, London, Philadelphia, Toronto etc. 1992
- Wiencke, Markus (2006) Schizophrenie als Ergebnis von Wechselwirkungen: Georg Simmels Individualitätskonzept in der Klinischen Psychologie. In David Kim (ed.), Georg Simmel in Translation: Interdisciplinary Border-Crossings in Culture and Modernity (pp. 123–155). Cambridge Scholars Press, Cambridge, ISBN 1-84718-060-4
External links
| Wikimedia Commons has media related to Mental and behavioural diseases and disorders. |
- NIMH.NIH.gov – National Institute of Mental Health
- International Committee of Women Leaders on Mental Health
- Psychology Dictionary
- Mental Illness Watch
- Metapsychology Online Reviews: Mental Health
- The New York Times: Mental Health & Disorders
- The Guardian: Mental Health
- Perring, Christian (22 February 2010). "Mental Illness". Stanford Encyclopedia of Philosophy.
-
 "Insane, Statistics of". Encyclopedia Americana. 1920.
"Insane, Statistics of". Encyclopedia Americana. 1920. - Adverse Childhood Experiences: Risk Factors for Substance Misuse and Mental Health Dr. Robert Anda of the U.S. Centers for Disease Control describes the relation between childhood adversity and mental health (video)
| Library resources about Mental illness |
