List of signs and symptoms of diving disorders

Diving disorders are medical conditions specifically arising from underwater diving. The signs and symptoms of these may present during a dive, on surfacing, or up to several hours after a dive. Divers have to breathe a gas which is at the same pressure as their surroundings (ambient pressure), which can be much greater than on the surface. The ambient pressure underwater increases by 1 standard atmosphere (100 kPa) for every 10 metres (33 ft) of depth.[1]
The principal conditions are: decompression illness (which covers decompression sickness and arterial gas embolism); nitrogen narcosis; high pressure nervous syndrome; oxygen toxicity; and pulmonary barotrauma (burst lung). Although some of these may occur in other settings, they are of particular concern during diving activities.[1]
The disorders are caused by breathing gas at the high pressures encountered at depth, and divers will often breathe a gas mixture different from air to mitigate these effects. Nitrox, which contains more oxygen and less nitrogen, is commonly used as a breathing gas to reduce the risk of decompression sickness at recreational depths (up to about 40 metres (130 ft)). Helium may be added to reduce the amount of nitrogen and oxygen in the gas mixture when diving deeper, to reduce the effects of narcosis and to avoid the risk of oxygen toxicity. This is complicated at depths beyond about 150 metres (500 ft), because a helium–oxygen mixture (heliox) then causes high pressure nervous syndrome.[1] More exotic mixtures such as hydreliox, a hydrogen–helium–oxygen mixture, are used at extreme depths to counteract this.[2]
Decompression sickness

Decompression sickness (DCS) occurs when gas, which has been breathed under high pressure and dissolved into the body tissues, forms bubbles as the pressure is reduced on ascent from a dive. The results may range from pain in the joints where the bubbles form to blockage of an artery leading to damage to the nervous system, paralysis or death. While bubbles can form anywhere in the body, DCS is most frequently observed in the shoulders, elbows, knees, and ankles. Joint pain occurs in about 90% of DCS cases reported to the U.S. Navy, with neurological symptoms and skin manifestations each present in 10% to 15% of cases. Pulmonary DCS is very rare in divers.[3] The table below classifies the effects by affected organ and bubble location.[4]
| DCS type | Bubble location | Clinical manifestations |
|---|---|---|
| Musculoskeletal | Mostly large joints |
|
| Cutaneous | Skin |
|
| Neurologic | Brain |
|
| Neurologic | Spinal cord |
|
| Constitutional | Whole body | |
| Audiovestibular | Inner ear | |
| Pulmonary | Lungs |
|
Arterial gas embolism and pulmonary barotrauma
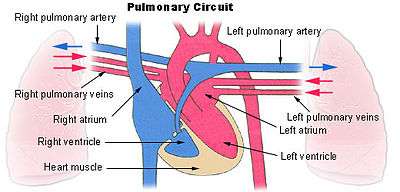
If the compressed air in a diver's lungs cannot freely escape during an ascent, particularly a rapid one, then the lung tissues may rupture, causing pulmonary barotrauma (PBT). The air may then enter the arterial circulation producing arterial gas embolism (AGE), with effects similar to severe decompression sickness.[5] Although AGE may occur as a result of other causes, it is most often secondary to PBT. AGE is the second most common cause of death while diving (drowning being the most common stated cause of death). Gas bubbles within the arterial circulation can block the supply of blood to any part of the body, including the brain, and can therefore manifest a vast variety of symptoms. The following table presents those signs and symptoms which have been observed in more than ten percent of cases diagnosed as AGE, with approximate estimates of frequency.[6]
| Symptom | Percentage |
|---|---|
| Loss of consciousness | 81 |
| Pulmonary rales or wheezes | 38 |
| Blood in the ear (Hemotympanum) | 34 |
| Decreased reflexes | 34 |
| Extremity weakness or paralysis | 32 |
| Chest pain | 29 |
| Irregular breathing or apnea | 29 |
| Vomiting | 29 |
| Coma without convulsions | 26 |
| Coughing blood (Hemoptysis) | 23 |
| Sensory loss | 21 |
| Stupor and confusion | 18 |
| Vision changes | 20 |
| Cardiac arrest | 16 |
| Headache | 16 |
| Unilateral motor changes | 16 |
| Change in gait or ataxia | 14 |
| Conjunctivitis | 14 |
| Sluggishly reactive pupils | 14 |
| Vertigo | 12 |
| Coma with convulsions | 11 |
Nitrogen narcosis

Nitrogen narcosis is caused by the pressure of dissolved gas in the body and produces impairment to the nervous system. This results in alteration to thought processes and a decrease in the diver's ability to make judgements or calculations. It can also decrease motor skills, and worsen performance in tasks requiring manual dexterity. As depth increases, so does the pressure and hence the severity of the narcosis. The effects may vary widely from individual to individual, and from day to day for the same diver. Because of the perception-altering effects of narcosis, a diver may not be aware of the symptoms, but studies have shown that impairment occurs nevertheless.[7] Since the choice of breathing gas also affects the depth at which narcosis occurs, the table below represents typical manifestations when breathing air.[8]
| Pressure (bar) | Depth (m) | Depth (ft) | Manifestations |
|---|---|---|---|
| 1–2 | 0–10 | 0–33 |
|
| 2–4 | 10–30 | 33–100 |
|
| 4–6 | 30–50 | 100–165 |
|
| 6–8 | 50–70 | 165–230 |
|
| 8–10 | 70–90 | 230–300 |
|
| 10+ | 90+ | 300+ |
|
High pressure nervous syndrome
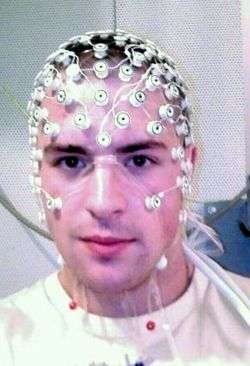
Helium is the least narcotic of all gases, and divers may use breathing mixtures containing a proportion of helium for dives exceeding about 40 metres (130 ft) deep. In the 1960s it was expected that helium narcosis would begin to become apparent at depths of 300 metres (1,000 ft). However, it was found that different symptoms, such as tremors, occurred at shallower depths around 150 metres (500 ft). This became known as high pressure nervous syndrome, and its effects are found to result from both the absolute depth and the speed of descent. Although the effects vary from person to person, they are stable and reproducible for each individual; the list below summarises the symptoms observed underwater and in studies using simulated dives in the dry, using recompression chambers and electroencephalography (EEG) monitors.[9]
| Symptom | Notes |
|---|---|
| Impairment | Both intellectual and motor performance are impaired. A 20% decrease in the ability to perform calculations and in manual dexterity is observed at 180 metres (600 ft), rising to 40% at depths of 240 metres (800 ft) |
| Dizziness | Vertigo, nausea, and vomiting may occur in divers at depths of 180 metres (600 ft). Animal studies under more extreme conditions have produced convulsions. |
| Tremors | Tremors of the hands, arms and torso are observed from 130 metres (400 ft) onward. The tremors occur with a frequency in the range of 5–8 hertz (Hz), and their severity is related to the speed of compression; the tremors reduce and may disappear when the pressure has stabilised. |
| EEG changes | At depths exceeding 300 metres (1,000 ft), changes in the electroencephalogram (EEG) are observed; the appearance of theta waves (4–6 Hz) and depression of alpha waves (8–13 Hz). |
| Somnolence | At depths beyond the onset of EEG changes, test subjects intermittently fall asleep, with sleep stages 1 and 2 observed in the EEG. Even when decompressed to shallower depths, the effect continues for 10–12 hours. |
Oxygen toxicity
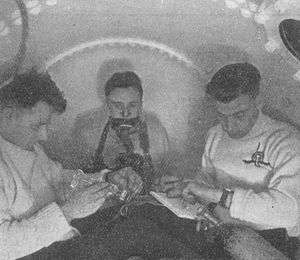
Although oxygen is essential to life, in concentrations greater than normal it becomes toxic, overcoming the body's natural defences (antioxidants), and causing cell death in any part of the body. The lungs and brain are particularly affected by high partial pressures of oxygen, such as are encountered in diving. The body can tolerate partial pressures of oxygen around 0.5 bars (50 kPa; 7.3 psi) indefinitely, and up to 1.4 bars (140 kPa; 20 psi) for many hours, but higher partial pressures rapidly increase the chance of the most dangerous effect of oxygen toxicity, a convulsion resembling an epileptic seizure.[10] Susceptibility to oxygen toxicity varies dramatically from person to person, and to a much smaller extent from day to day for the same diver.[11] Prior to convulsion, several symptoms may be present – most distinctly that of an aura.
During 1942 and 1943, Professor Kenneth W Donald, working at the Admiralty Experimental Diving Unit, carried out over 2,000 experiments on divers to examine the effects of oxygen toxicity. To date, no comparable series of studies has been performed. In one seminal experiment, Donald exposed 36 healthy divers to 3.7 bars (370 kPa; 54 psi) of oxygen in a chamber, equivalent to breathing pure oxygen at a depth of 27 metres (90 ft), and recorded the time of onset of various signs and symptoms. Five of the subjects convulsed, and the others recovered when returned to normal pressure following the appearance of acute symptoms. The table below summarises the results for the relative frequency of the symptoms, and the earliest and latest time of onset, as observed by Donald. The wide variety of symptoms and large variability of onset between individuals typical of oxygen toxicity are clearly illustrated.[12]
| Signs and symptoms | Frequency | Earliest onset (minutes) | Latest onset (minutes) |
|---|---|---|---|
| Lip-twitching | 25 | 6 | 67 |
| Vertigo | 5 | 9 | 62 |
| Convulsion | 5 | 20 | 33 |
| Nausea | 4 | 6 | 62 |
| Spasmodic respiration | 3 | 16 | 17 |
| Dazed | 2 | 9 | 51 |
| Syncope | 2 | 15 | 16 |
| Epigastric aura | 2 | 18 | 23 |
| Arm twitch | 2 | 21 | 62 |
| Dazzle | 2 | 51 | 96 |
| Diaphragmatic spasm | 1 | 7 | 7 |
| Tingling | 1 | 9 | 9 |
| Confusion | 1 | 15 | 15 |
| Inspiratory predominance[note 1] | 1 | 16 | 16 |
| Amnesia | 1 | 21 | 21 |
| Drowsiness | 1 | 26 | 26 |
| Fell asleep | 1 | 51 | 51 |
| Euphoria | 1 | 62 | 62 |
| Vomiting | 1 | 96 | 96 |
- Note
- ↑ Normally, breathing in takes less time than breathing out; inspiratory predominance is a reversal of this.
References
- 1 2 3 Brubakk, Alf O; Neuman, Tom S, eds. (2003). "9: Pressure Effects". Bennett and Elliott's physiology and medicine of diving (5th Revised ed.). United States: Saunders Ltd. pp. 265–418. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Abraini, JH; Gardette-Chauffour, MC; Martinez,, E; Rostain, JC; Lemaire, C (1994). "Psychophysiological reactions in humans during an open sea dive to 500 m with a hydrogen-helium-oxygen mixture". Journal of Applied Physiology. American Physiological Society. 76 (3): 1113–8. ISSN 8750-7587. PMID 8005852. Retrieved 1 March 2009.
- ↑ Powell, Mark (2008). Deco for Divers. Southend-on-Sea: Aquapress. p. 70. ISBN 1-905492-07-3.
- ↑ Francis, T James R; Mitchell, Simon J (2003). "10.6: Manifestations of Decompression Disorders". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th Revised ed.). United States: Saunders Ltd. pp. 578–99. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Neuman, Tom S (2003). "10.5: Arterial Gas Embolism and Pulmonary Barotrauma". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. pp. 557–8. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Neuman, Tom S (2003). "10.5: Arterial Gas Embolism and Pulmonary Barotrauma". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. pp. 568–71. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Bennett, Peter B; Rostain, Jean Claude (2003). "9.2: Inert Gas Narcosis". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. p. 301. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Lippmann, John; Mitchell, Simon J (2005). "Nitrogen narcosis". Deeper into Diving (2nd ed.). Victoria, Australia: J L Publications. p. 105. ISBN 0-9752290-1-X. OCLC 66524750.
- ↑ Bennett, Peter B; Rostain, Jean Claude (2003). "9.3: The High Pressure Nervous Syndrome". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. pp. 323–8. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Clark, James M; Thom, Stephen R (2003). "9.4: Oxygen under pressure". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. pp. 358–360. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Clark, James M; Thom, Stephen R (2003). "9.4: Oxygen under pressure". In Brubakk, Alf O; Neuman, Tom S. Bennett and Elliott's physiology and medicine of diving (5th ed.). United States: Saunders Ltd. p. 376. ISBN 0-7020-2571-2. OCLC 51607923.
- ↑ Donald, Kenneth W (1947). "Oxygen poisoning in man — part I". British Medical Journal. 1 (4506): 667–72. doi:10.1136/bmj.1.4506.667. PMC 2053251
 . PMID 20248086.
. PMID 20248086.
Further reading
- "Descriptive Classification of Diving Disorders" (PDF). European Committee for Hyperbaric Medicine. September 2003. Retrieved 22 November 2010.
- Donald, Kenneth W (1947). "Oxygen poisoning in man — part II". British Medical Journal. 1 (4507): 712–7. doi:10.1136/bmj.1.4507.712. PMC 2053400
 . PMID 20248096.
. PMID 20248096. - Francis T James R, Smith DJ (eds) (1991). "Describing Decompression Illness". 42nd Undersea and Hyperbaric Medical Society Workshop. UHMS Publication Number 79(DECO)5-15-91. Undersea and Hyperbaric Medical Society. Retrieved 2011-03-11.
- Bevan, John (1999). "Early diving problems and fatalities". South Pacific Underwater Medicine Society Journal. 29 (3). Retrieved 2011-06-13.

