Legionella
The genus Legionella is a pathogenic group of Gram-negative bacteria that includes the species L. pneumophila, causing legionellosis[1] (all illnesses caused by Legionella) including a pneumonia-type illness called Legionnaires' disease and a mild flu-like illness called Pontiac fever.[1]
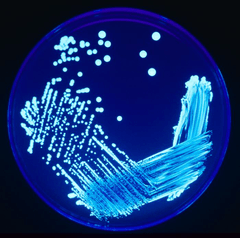
Legionella may be readily visualized with a silver stain or cultured in cysteine-containing media such as BCYE. It is common in many environments, including soil and aquatic systems, with at least 50 species and 70 serogroups identified. The bacterium, however, is not transmissible from person to person:[2] furthermore, most people exposed to the bacteria do not become ill.[3]
The side chains of the cell wall carry the bases responsible for the somatic antigen specificity of these organisms. The chemical composition of these side chains both with respect to components and arrangement of the different sugars determines the nature of the somatic or O antigen determinants, which are essential means of serologically classifying many Gram-negative bacteria.
Legionella acquired its name after an outbreak of a then-unknown "mystery disease" sickened 221 persons, causing 34 deaths. The outbreak was first noticed among people attending a convention of the American Legion—an association of U.S. military veterans. The convention occurred in Philadelphia during the U.S. Bicentennial year in July 21–24, 1976. This epidemic among U.S. war veterans, occurring in the same city as—and within days of the 200th anniversary of—the signing of the Declaration of Independence, was widely publicized and caused great concern in the United States.[4]
On January 18, 1977, the causative agent was identified as a previously unknown bacterium subsequently named Legionella. See Legionnaires' disease for full details.
Detection
Legionella is traditionally detected by culture on buffered charcoal yeast extract (BCYE) agar. Legionella requires the presence of cysteine and iron to grow, so does not grow on common blood agar media used for laboratory-based total viable counts or on-site dipslides. Common laboratory procedures for the detection of Legionella in water[5] concentrate the bacteria (by centrifugation and/or filtration through 0.2-μm filters) before inoculation onto a charcoal yeast extract agar containing antibiotics (e.g. glycine, vancomycin, polymixin, cyclohexamide, GVPC) to suppress other flora in the sample. Heat or acid treatment are also used to reduce interference from other microbes in the sample.
After incubation for up to 10 days, suspect colonies are confirmed as Legionella if they grow on BCYE containing cysteine, but not on agar without cysteine added. Immunological techniques are then commonly used to establish the species and/or serogroups of bacteria present in the sample.
Although the plating method is quite specific for most species of Legionella, one study has shown that a coculture method that accounts for the close relationship with amoebae may be more sensitive since it can detect the presence of the bacteria even when masked by its presence inside the amoeba.[6] Consequently, the true clinical and environmental prevalence of the bacteria is likely to be underestimated due to false negatives inherent in the current lab methodology.
Many hospitals use the Legionella urinary antigen test for initial detection when Legionella pneumonia is suspected. Some of the advantages offered by this test are that the results can be obtained in a matter of hours rather than the five days required for culture, and that a urine specimen is generally more easily obtained than a sputum specimen. Disadvantages are that the urine antigen test only detects antigen of Legionella pneumophila serogroup 1 (LP1); only a culture will detect infection by non-LP1 strains or other Legionella species and that isolates of Legionella are not obtained, which impairs public health investigations of outbreaks of LD.[7]
New techniques for the rapid detection of Legionella in water samples are emerging, including the use of polymerase chain reaction and rapid immunological assays. These technologies can typically provide much faster results.
Government public health surveillance has demonstrated increasing proportions of drinking water–associated outbreaks specifically in healthcare settings.[8]
Pathogenesis

In the natural environment, Legionella lives within amoebae such as Acanthamoeba spp., Naegleria spp., Tetrahymena pyriformis, and Vermamoeba vermiformis.[9]
Upon inhalation, the bacteria can infect alveolar macrophages, subverting the normal host cell machinery to create a niche where the bacteria can replicate. This results in Legionnaires' disease and the lesser form, Pontiac fever. Legionella transmission is airborne via respiratory droplets containing the bacteria .
Once inside a host, incubation may take up to two weeks. Prodromal symptoms are flu-like, including fever, chills, and dry cough. Advanced stages of the disease cause problems with the gastrointestinal tract and the nervous system and lead to diarrhea and nausea. Other advanced symptoms of pneumonia may also present. However, the disease is generally not a threat to most healthy individuals, and tends to lead to harmful symptoms only in the immunocompromised host and the elderly. Consequently, it should be actively checked for in the water systems of hospitals and nursing homes. The Texas Department of State Health services provides recommendations for hospitals to detect and prevent the spread of hospital acquired disease due to Legionella infection.[10] According to Infection Control and Hospital Epidemiology, hospital-acquired Legionella pneumonia has a fatality rate of 28%, and the source is the water distribution system.[11]
In the United States, the disease affects between 8,000 and 18,000 individuals a year.[12]
Person-to-person transmission of Legionella has not been demonstrated.[2]
Legionella species typically exist in nature at low concentrations, in groundwater, lakes, and streams. After entering man-made equipment, given the right environmental conditions, it may reproduce.
Sources of Legionella
Documented sources include cooling towers,[13] swimming pools (especially in Scandinavian countries), domestic water systems and showers, ice-making machines,[14] refrigerated cabinets, whirlpool spas,[15][16] hot springs,[17] fountains,[18] dental equipment,[19] Soil,[20] automobile windshield washer fluid,[21] and industrial coolant.[22]
Airborne transmission from cooling towers
The largest[23] and most common source of Legionnaires' disease outbreaks are cooling towers (heat rejection equipment used in air conditioning and industrial cooling water systems) primarily because of the risk for widespread circulation. Many governmental agencies, cooling tower manufacturers, and industrial trade organisations have developed design and maintenance guidelines for controlling the growth and proliferation of Legionella within cooling towers.
Recent research in the Journal of Infectious Diseases provides evidence that L. pneumophila, the causative agent of Legionnaires' disease, can travel at least 6 km from its source by airborne spread. It was previously believed that transmission of the bacterium was restricted to much shorter distances. A team of French scientists reviewed the details of an epidemic of Legionnaires' disease that took place in Pas-de-Calais, northern France, in 2003–2004. Of 86 confirmed cases during the outbreak, 18 resulted in death. The source of infection was identified as a cooling tower in a petrochemical plant, and an analysis of those affected in the outbreak revealed that some infected people lived as far as 6–7 km from the plant.[24]
Vaccine research
No vaccine is available for legionellosis, and antibiotic prophylaxis is not effective. Any licensed vaccine for humans in the US is most probably still many years away. Vaccination studies using heat-killed or acetone-killed cells have been carried out, and guinea pigs were challenged intraperitoneally or by using the aerosol model of infection. Both vaccines were shown to give moderately high levels of protection. Protection was found to be dose-dependent and correlated with antibody levels as measured by enzyme-linked immunosorbent assay to an outer membrane antigen and by indirect immunofluorescence to heat-killed cells.
Molecular biology
Legionella has been discovered to be a genetically diverse species with 7-11% of genes strain-specific. The molecular function of some of the proven virulence factors of Legionella have been discovered.[25]
Legionella control
Control of Legionella growth can occur through chemical or thermal methods. The most expensive of these two options is temperature control—i.e., keeping all cold water below 25 °C (78 °F) and all hot water above 51 °C (124 °F). The high cost incurred with this method arises from the extensive retrofitting required for existing complex distribution systems in large facilities and the energy cost of chilling or heating the water and maintaining the required temperatures at all times and at all distal points within the system.
According to the 2007 book Legionella and the prevention of legionellosis[1] from the World Health Organization, temperature affects the survival of Legionella as follows:
- Above 70 °C (158 °F) – Legionella dies almost instantly
- At 60 °C (140 °F) – 90% die in 2 minutes (Decimal reduction time (D) = 2 minutes)
- At 50 °C (122 °F) – 90% die in 80–124 minutes, depending on strain (Decimal reduction time (D) = 80–124 minutes)
- 48 to 50 °C (118 to 122 °F) – can survive but do not multiply
- 32 to 42 °C (90 to 108 °F) – ideal growth range
- 25 to 45 °C (77 to 113 °F) – growth range
- Below 20 °C (68 °F) – can survive, even below freezing, but are dormant
Other sources[26][27][28] claim alternate temperature ranges:
- 60 to 70 °C (140 to 158 °F) to 80 °C (176 °F) – Disinfection range
- 66 °C (151 °F) – Legionella dies within 2 minutes
- 60 °C (140 °F) – Legionella dies within 32 minutes
- 55 °C (131 °F) – Legionella dies within 5 to 6 hours
- 20 to 45 °C (68 to 113 °F) – Legionella multiplies
- 20 °C (68 °F) and below – Legionella is dormant
Chlorine
A very effective chemical treatment is chlorine. For systems with marginal issues, chlorine provides effective results at 0.5 ppm residual in the hot water system. For systems with significant Legionella problems, temporary shock chlorination—where levels are raised to higher than 2 ppm for a period of 24 hours or more and then returned to 0.5 ppm may be effective. Hyperchlorination can also be used where the water system is taken out of service and the chlorine residual is raised to 50 ppm or higher at all distal points for 24 hours or more. The system is then flushed and returned to 0.5 ppm chlorine prior to being placed back into service. These high levels of chlorine penetrate biofilm, killing both the Legionella bacteria and the host organisms. Annual hyperchlorination can be an effective part of a comprehensive Legionella preventive action plan.
Copper-silver (CuAg) ionization
Industrial-size copper-silver ionization is recognized by the U.S. Environmental Protection Agency and WHO for Legionella control and prevention. Copper and silver ion concentrations must be maintained at optimal levels, taking into account both water flow and overall water usage, to control Legionella. The disinfection function within all of a facility's water distribution network occurs within 30 to 45 days. Key engineering features such as 10 amps per ion chamber cell and automated variable voltage outputs having no less than 100 VDC are but a few of the required features for proper Legionella control and prevention, using a specific, nonreferenced CuAg system. Swimming pool ion generators are not designed for potable water treatment.
Questions remain whether the silver and copper ion concentrations required for effective control of symbiotic hosts could exceed those allowed under the U.S. Safe Drinking Water Act's Lead and Copper Rule. In any case, any facility or public water system using CuAg for disinfection should monitor its copper and silver ion concentrations to ensure they are within intended levels – both minimum and maximum. Further, no current standards for silver in the EU and other regions allow use of this technology.
CuAg ionization is an effective process to control Legionella in potable water distribution systems found in health facilities, hotels, nursing homes, and most large buildings. CuAg is not intended for cooling towers because of pH levels over 8.6 that cause ionic copper to precipitate. In 2003, researchers who heavily support ionization developed a validation process that supports their research on ionization. Ionization became the first such hospital disinfection process to have fulfilled a proposed four-step modality evaluation; by then it had been adopted by over 100 hospitals.[29] Additional studies indicate ionization is superior to thermal eradication.[30]
Chlorine dioxide
Chlorine dioxide has been EPA approved as a primary potable water disinfectant since 1945. Chlorine dioxide does not produce any carcinogenic byproducts like chlorine when used in the purification of drinking water that contains natural organic compounds such as humic and fulvic acids, chlorine tends to form halogenated disinfection by-products such as trihalomethanes (THMs). Drinking water containing such disinfection by-products has been shown to increase the risk of cancer. ClO2 works differently to chlorine; its action is one of pure oxidation rather than halogenation, so these halogenated by-products are not formed.[31] Chlorine Dioxide is not a restricted heavy metal like copper. It has proven excellent control of Legionella in cold and hot water systems and its ability as a biocide is not affected by pH, or any water corrosion inhibitors such as silica or phosphate. Monochloramine is an alternative. Like chlorine and chlorine dioxide, monochloramine is EPA approved as a primary potable water disinfectant. EPA registration requires an EPA biocide label which lists toxicity and other data required by the EPA for all registered biocides. If the product is being sold as a biocide, then the manufacturer is legally required to supply a biocide label, and the purcharser is legally required to apply the biocide per the biocide label. When first applied to a system, chlorine dioxide can be added at disinfection levels of 2 ppm for 6 hours to clean up a system. This will not remove all biofilm, but will effectively remediate the system of Legionella.
Moist heat sterilization
Moist heat sterilization (superheating to 140 °F (60 °C) and flushing) is a nonchemical treatment that typically must be repeated every 3–5 weeks.
European standards
Several European countries established the European Working Group for Legionella Infections (EWGLI)[32] to share knowledge and experience about monitoring potential sources of Legionella. The EWGLI has published guidelines about the actions to be taken to limit the number of colony-forming units (that is, live bacteria that are able to multiply) of Legionella per litre:
| Legionella bacteria CFU/litre | Action required (35 samples per facility are required, including 20 water and 10 swabs) |
|---|---|
| 1000 or less | System under control |
| more than 1000 up to 10,000 | Review program operation: The count should be confirmed by immediate resampling. If a similar count is found again, a review of the control measures and risk assessment should be carried out to identify any remedial actions. |
| more than 10,000 | Implement corrective action: The system should immediately be resampled. It should then be "shot dosed" with an appropriate biocide, as a precaution. The risk assessment and control measures should be reviewed to identify remedial actions. (150+ CFU/ml in healthcare facilities or nursing homes require immediate action.) |
Monitoring guidelines are stated in Approved Code of Practice (ACOP) L8 in the UK. These are not mandatory, but are widely regarded as so. An employer or property owner must follow an ACOP, or achieve the same result. Failure to show monitoring records to at least this standard has resulted in several high-profile prosecutions, e.g. Nalco + Bulmers – neither could prove a sufficient scheme to be in place whilst investigating an outbreak, therefore both were fined about £300,000GBP. Important case law in this area is R v Trustees of the Science Museum 3 All ER 853, (1993) 1 WLR 1171[33]
Employers and those responsible for premises within the UK are required under COSHH to undertake an assessment of the risks arising from Legionella. This risk assessment may be very simple for low risk premises, however for larger or higher risk properties may include a narrative of the site, asset register, simplified schematic drawings, recommendations on compliance, and a proposed monitoring scheme.[34]
The L8 ACOP recommend that the risk assessment should be reviewed at least every 2 years and whenever a reason exists to suspect it is no longer valid, such as water systems have been amended or modified, or if the use of the water system has changed, or if there is reason to suspect that Legionella control measures are no longer working.
Weaponization
It has been suggested that Legionella could be used as a weapon, and indeed genetic modification of Legionella pneumophila has been shown where the mortality rate in infected animals can be increased to nearly 100%.[35][36][37] A former Soviet bioengineer, Sergei Popov, stated in 2000 that his team experimented with genetically enhanced bioweapons, including Legionella.[37] Popov worked as a lead researcher at the Vector Institute from 1976 to 1986, then at Obolensk until 1992, when he defected to the West. He later divulged much of the Soviet biological weapons program and settled in the United States.
See also
References
- 1 2 3 Legionella and the prevention of legionellosis (PDF).
- 1 2 Winn WC (1996). "Legionella". In Baron S. Baron's Medical Microbiology (4th ed.). University of Texas Medical Branch. ISBN 0-9631172-1-1.
- ↑ http://www.medscape.com/viewarticle/852874
- ↑ Lawrence K. Altman (August 1, 2006). "In Philadelphia 30 Years Ago, an Eruption of Illness and Fear". New York Times.
- ↑ ISO 11731-2:2004 Water quality -- Detection and enumeration of Legionella -- Part 2: Direct membrane filtration method for waters with low bacterial counts
- ↑ La Scola B, Mezi L, Weiller PJ, Raoult D (January 2001). "Isolation of Legionella anisa using an amoebic coculture procedure". Journal of Clinical Microbiology. 39 (1): 365–6. doi:10.1128/JCM.39.1.365-366.2001. PMC 87733
 . PMID 11136802.
. PMID 11136802. - ↑ Benin AL, Benson RF, Besser RE (November 2002). "Trends in legionnaires disease, 1980-1998: declining mortality and new patterns of diagnosis". Clinical Infectious Diseases. 35 (9): 1039–46. doi:10.1086/342903. PMID 12384836.
- ↑ Surveillance for Waterborne Disease Outbreaks Associated with Drinking Water — United States, 2011–2012. (August 14, 2015). Morbidity and Mortality Weekly Report (MMWR) Centers of Disease Control and Prevention. 64(31);pp. 842-848. Retrieved 6 April 2016. Centers for Disease Control website
- ↑ Swanson MS, Hammer BK (2000). "Legionella pneumophila pathogesesis: a fateful journey from amoebae to macrophages". Annual Review of Microbiology. 54: 567–613. doi:10.1146/annurev.micro.54.1.567. PMID 11018138.
- ↑ Report of the Texas Legionnaires' Disease Task Force, Texas Department of State Health Services
- ↑ Stout JE, Muder RR, Mietzner S, et al. (July 2007). "Role of environmental surveillance in determining the risk of hospital-acquired legionellosis: a national surveillance study with clinical correlations". Infection Control and Hospital Epidemiology. 28 (7): 818–24. doi:10.1086/518754. PMID 17564984.
- ↑ http://www.cdc.gov/legionella/fastfacts.html[]
- ↑ Osawa K, Shigemura K, Abe Y, et al. (January 2014). "A case of nosocomial Legionella pneumonia associated with a contaminated hospital cooling tower". Journal of Infection and Chemotherapy. 20 (1): 68–70. doi:10.1016/j.jiac.2013.07.007. PMID 24462430.
- ↑ Graman PS, Quinlan GA, Rank JA (September 1997). "Nosocomial legionellosis traced to a contaminated ice machine". Infection Control and Hospital Epidemiology. 18 (9): 637–40. doi:10.2307/30141491. PMID 9309436.
- ↑ Coetzee N, Duggal H, Hawker J, et al. (2012). "An outbreak of Legionnaires' disease associated with a display spa pool in retail premises, Stoke-on-Trent, United Kingdom, July 2012". Euro Surveillance. 17 (37). PMID 22995431.
- ↑ Campese C, Roche D, Clément C, et al. (July 2010). "Cluster of Legionnaires' disease associated with a public whirlpool spa, France, April-May 2010". Euro Surveillance. 15 (26). PMID 20619131.
- ↑ Kurosawa H, Fujita M, Kobatake S, et al. (January 2010). "A case of Legionella pneumonia linked to a hot spring facility in Gunma Prefecture, Japan". Japanese Journal of Infectious Diseases. 63 (1): 78–9. PMID 20093771.
- ↑ Palmore TN, Stock F, White M, et al. (August 2009). "A cluster of cases of nosocomial legionnaires disease linked to a contaminated hospital decorative water fountain". Infection Control and Hospital Epidemiology. 30 (8): 764–8. doi:10.1086/598855. PMC 2886954
 . PMID 19580436.
. PMID 19580436. - ↑ Kadaifciler DG, Cotuk A (June 2014). "Microbial contamination of dental unit waterlines and effect on quality of indoor air". Environmental Monitoring and Assessment. 186 (6): 3431–44. doi:10.1007/s10661-014-3628-6. PMID 24469014.
- ↑ Infection Due to Legionella Species Other Than L. pneumophila Barry S. Fields*, Robert F. Benson, and Richard E. Besser http://cid.oxfordjournals.org/content/35/8/990.full
- ↑ American Society for Microbiology, Windshield washer fluid a source of Legionnaires: Found in most school buses
- ↑ RR910 - Survival of Legionella pneumophila in metalworking fluids http://www.hse.gov.uk/research/rrhtm/rr910.htm
- ↑ http://wwwnc.cdc.gov/eid/article/9/8/03-0337_article.htm[]
- ↑ Nguyen TM, Ilef D, Jarraud S, et al. (January 2006). "A community-wide outbreak of legionnaires disease linked to industrial cooling towers--how far can contaminated aerosols spread?". The Journal of Infectious Diseases. 193 (1): 102–11. doi:10.1086/498575. PMID 16323138.
- ↑ Raychaudhury S, Farelli JD, Montminy TP, et al. (April 2009). "Structure and function of interacting IcmR-IcmQ domains from a type IVb secretion system in Legionella pneumophila". Structure. 17 (4): 590–601. doi:10.1016/j.str.2009.02.011. PMC 2693034
 . PMID 19368892.
. PMID 19368892. - ↑ "Safe Hot Water Temperature" (PDF).
- ↑ "Controlling Legionella in Domestic Hot Water Systems" (PDF).
- ↑ "Employers Guide to the control of Legionella" (PDF).
- ↑ Stout & Yu 2003 "(1) Demonstrated efficacy of Legionella eradication in vitro using laboratory assays, (2) anecdotal experiences in preventing legionnaires’ disease in individual hospitals, (3) controlled studies in individual hospitals, and (4) validation in confirmatory reports from multiple hospitals during a prolonged time."
- ↑ Block 2001.
- ↑ Legionella Control With Chlorine Dioxide. Retrieved from https://feedwater.co.uk/legionella-control-services/
- ↑ "European Working Group for Legionella Infections".
- ↑ http://www.hse.gov.uk/chemicals/workshop/legionella-09/law-and-legionella.pdf[]
- ↑ http://www.hse.gov.uk/legionnaires/what-you-must-do.htm
- ↑ http://www.aina.org/news/20081201063837.htm[]
- ↑ Gilsdorf JR, Zilinskas RA (April 2005). "New considerations in infectious disease outbreaks: the threat of genetically modified microbes". Clinical Infectious Diseases. 40 (8): 1160–5. doi:10.1086/428843. JSTOR 4463254. PMID 15791517.
- 1 2 http://www.homelandsecurity.org/journal/Interviews/PopovInterview_001107.htm Archive: http://web.archive.org/web/20110927023507/http://www.homelandsecurity.org/journal/Interviews/PopovInterview_001107.htm[]
External links
- CDC Division of bacterial and Mycotic Diseases: Legionellosis
- Directors of Health Promotion and Education page on Legionellosis
- European Working Group for Legionella Infections
- Legionnaires' disease outbreaks
- Legionella Information
- Legionella Risk management
- Legionella case studies
Maintenance guidelines
- Centers for Disease Control and Prevention - Procedure for Cleaning Cooling Towers and Related Equipment (pages 239 and 240 of 249)
- Cooling Technology Institute - Best Practices for Control of Legionella
- California Energy Commission - Cooling Water Management Program Guidelines For Wet and Hybrid Cooling Towers at Power Plants
- ASHRAE Guideline
- Guidelines for Control of Legionella in Ornamental Fountains
- Employers Guidelines for prevention of Legionella