Kegel exercise
| Kegel exercise | |
|---|---|
| Intervention | |
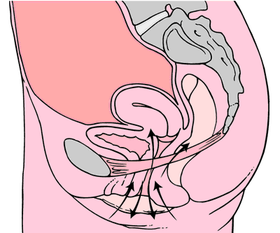 Kegel exercises diagram | |
| Pronunciation | Kegel /ˈkeɪɡəl/ |
Pelvic floor exercise, also known as Kegel exercise, consists of repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise needs to be performed multiple times each day, for several minutes at a time, for one to three months, to begin to have an effect.[1][2]
Exercises are usually done to reduce urinary stress incontinence[2] (especially after childbirth)[3] and reduce premature ejaculatory occurrences in men,[4] as well as to increase the size and intensity of erections.[5]
Several tools exist to help with these exercises, although various studies debate the relative effectiveness of different tools versus traditional exercises.[6][7]
They were first described in 1948 by Arnold Kegel.
Health effects for women
Factors such as pregnancy, childbirth, aging, being overweight, and abdominal surgery such as cesarean section, often result in the weakening of the pelvic muscles. This can be assessed by either digital examination of vaginal pressure or using a Kegel perineometer. Kegel exercises are useful in regaining pelvic floor muscle strength in such cases.
Urinary health
Pelvic floor exercise is the recommended first-line conservative treatment for women with urinary incontinence of the stress, urge, or mixed types.[8] There is tentative evidence that biofeedback may give added benefit when used with pelvic floor muscle training.[9]
Pelvic prolapse
The symptoms of prolapse and its severity can be decreased with pelvic floor exercises.[10] Effectiveness can be improved with feedback on how to do the exercises.[11]
Sexual function
In 1952, Dr. Kegel published a report in which he stated that the women doing this exercise were attaining orgasm more easily, more frequently and more intensely: "it has been found that dysfunction of the pubococcygeus exists in many women complaining of lack of vaginal feeling during coitus and that in these cases sexual appreciation can be increased by restoring function of the pubococcygeus".[12]
Health effects for men
Though most commonly used by women, men can also use Kegel exercises. Kegel exercises are employed to strengthen the pubococcygeal muscle and other muscles of the pelvic diaphragm. Kegels can help men achieve stronger erections, maintain healthy hips, and gain greater control over ejaculation.[5] The objective of this may be similar to that of the exercise in women with weakened pelvic floor: to increase bladder and bowel control and sexual function.
Urinary health
After a prostatectomy there is no clear evidence that teaching pelvic floor exercises alters the risk of urinary incontinence (leakage of urine).[13]
Sexual function
A paper found that pelvic floor exercises could help restore erectile function in men with erectile dysfunction.[14] There are said to be significant benefits for the problem of premature ejaculation from having more muscular control of the pelvis.[15]
Mechanism of action
The aim of Kegel exercises is to improve muscle tone by strengthening the pubococcygeus muscles of the pelvic floor. Kegel is a popular prescribed exercise for pregnant women to prepare the pelvic floor for physiological stresses of the later stages of pregnancy and childbirth. Kegel exercises are said to be good for treating vaginal prolapse[16] and preventing uterine prolapse[17] in women and for treating prostate pain and swelling resulting from benign prostatic hyperplasia (BPH) and prostatitis in men. Kegel exercises may be beneficial in treating urinary incontinence in both men and women.[2] Kegel exercises may also increase sexual gratification, allowing women to complete pompoir and aid in reducing premature ejaculation[4] in men. The many actions performed by Kegel muscles include holding in urine and avoiding defecation. Reproducing this type of muscle action can strengthen the Kegel muscles. The action of slowing or stopping the flow of urine may be used as a test of correct pelvic floor exercise technique.[18]
It is now known that the components of levator ani (the pelvic diaphragm), namely pubococcygeus, puborectalis and ileococcygeus, contract and relax as one muscle. Hence, pelvic floor exercises involve the entire levator ani rather than pubococcygeus alone. Pelvic floor exercises may be of benefit in cases of fecal incontinence and pelvic organ prolapse conditions e.g. rectal prolapse.[19]
Pelvic toning devices
A pelvic toning device (generically referred to as a Kegel exerciser,[20] pelvic floor toner, pelvic floor muscle toner or pelvic toner) is a medical or pseudo-medical device designed to help women exercise their pelvic floor muscle and improve the muscle tone of the pubococcygeal or vaginal muscle.
The original pelvic toning device was the perineometer, invented by Arnold Kegel to facilitate the measurement of the strength of the pubococcygeus muscle when it was resting and being actively squeezed—sometimes referred to as the Kegel tone.
His device was a combination of rubber balloons and tubes that measured pressure using a column of water. It was neither easy to use nor portable.
During the latter part of the 20th century, a number of medical and pseudo-medical devices were developed and launched on to the market. Some of these are used in a clinical setting, but most are designed for women to use in the privacy of their own home.
Pelvic toning devices fall into a number of different types:
- a Kegel ball, a small ball, typically 20–35 mm in diameter, of different weight, designed to be held in the vagina.
- barbells, vaginal weights or cones designed to be held in the vagina. The action of passively/actively retaining the device internally is supposed to improve muscle tone. Barbells are made of smooth, polished solid stainless steel, cylindrical in shape, with a rounded bulge at each end. They typically weigh one pound (454 g) and measure approximately 6 3⁄4 inches (17 cm) in length with a diameter of one inch (2.5 cm) at the widest part. Being made of stainless steel, vaginal barbells are nonporous and can be wiped clean with a cloth moistened with mild soap and water.
- electro-stimulation or TENS devices that administer an electric current through an internal probe. The current stimulates the adjacent muscles to twitch.
- rubber resistance balls and indicators. These devices provide a nominal resistance to squeeze against. An advantage of rubber bulb devices is that they provide visual feedback (via a gauge) of how much pressure is being applied.
- progressive resistance vaginal exercisers with springs are the only devices that meet all of Kegel's criteria. They provide a biofeedback that the correct muscles are being engaged and are capable of fulfilling the fundamentals of an exercise regimen by applying a variable and increasing resistive force to maximize the exercise effort.
Regular Kegel exercises should achieve tangible results (such as less frequent urine leakage) within about 8 to 12 weeks. For some women, the improvement could be dramatic.[21] Unfortunately, there are a number of products on the market that have no impact at all on the pubococcygeus muscle. If the PC muscle is not engaged then it is impossible to improve the muscle tone or strengthen the muscle. Devices that are used externally, for example between the thighs, may exercise the adductor muscle but do nothing for the pelvic floor.
Clinical research published in the British Medical Journal [6] compared pelvic floor exercises, vaginal weights and electro-stimulation in a randomised trial. The research recommended that pelvic floor exercise should be the first choice of treatment for genuine stress incontinence because simple exercises proved to be far more effective than electro-stimulation or vaginal cones.
This situation was confirmed in a comprehensive review of the treatment of stress incontinence published in the British Journal of Urology International in 2010.[7] The report author noted that electrical stimulation devices and weighted vaginal cones are not recommended by the UK National Institute for Clinical Excellence (NICE) and "are not universally advocated by clinicians as they have yet to produce sufficient evidence of efficacy".
Clinical trials[7] of a progressive resistance vaginal exerciser concluded that the device was as effective as supervised pelvic floor muscle training, the gold standard treatment of the UK NHS where patients are referred to a specialist continence advisor for one on one training over a three-month period. The report also noted that the device can help overcome the fundamental weaknesses associated with pelvic floor muscle exercises (PFME), i.e. poor training, lack of patient confidence and poor compliance with the exercise recommendations.
Key points noted by the research are that:
- the device gives "confidence to women that they were correctly contracting their pelvic floor, and this may be helpful encouragement when a woman is starting out on a regimen of PFME".
- the biofeedback given by the device "may be particularly helpful to demonstrate to the woman that she is carrying out the PFME appropriately".
- the device is particularly relevant to those women "who do not consult their physician and wish to maintain confidentiality regarding their SUI symptom".
A progressive resistance vaginal exerciser is the only form of pelvic toning device available on prescription in the UK to women presenting with symptoms of urinary stress incontinence or pelvic floor weakness.
See also
- Ben Wa balls
- Hypopressive exercise
- Taoist sexual practices
- Vacuum exercise
- Vaginal cone
- Vaginal weightlifting
References
- ↑ Bridgeman, Bruce; Roberts, Steven G. (2010-03-01). "The 4-3-2 method for Kegel exercises". American Journal of Men's Health. 4 (1): 75–76. doi:10.1177/1557988309331798. ISSN 1557-9891. PMID 19477754.
- 1 2 3 "MedlinePlus Medical Encyclopedia: Kegel exercises". Nlm.nih.gov. 2011-08-29. Retrieved 2011-09-02.
- ↑ Dumoulin C, Lemieux MC, Bourbonnais D et al 2004 Physiotherapy for persistent postnatal stress urinary incontinence: a randomised controlled trial. Obstetrics and Gynaecology 104:504-510
- 1 2 La Pera, G; Nicastro, A (1996). "A new treatment for premature ejaculation: the rehabilitation of the pelvic floor". Journal of sex & marital therapy. 22 (1): 22–6. doi:10.1080/00926239608405302. PMID 8699493.
- 1 2 Alan P. Brauer; Donna J. Brauer (2001). ESO: How You and Your Lover Can Give Each Other Hours of Extended Sexual Orgasm (Revised ed.). Warner Books. p. 59. ISBN 0-446-67762-0. Retrieved 2009-09-11.
Learning to tighten, to relax, and to push out the PC muscle allows a man to control his sexual system the way he controls a car. Tightening is the accelerator, increasing arousal. Pushing out is the brake—it can help stop ejaculation.
- 1 2 Bø; et al. "Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones and no treatment in management of genuine stress incontinence in women". bmj.com. p. 487. Retrieved 2011-09-02.
- 1 2 3 "A randomised controlled trial of the PelvicToner Device in female stress urinary incontinence". BJUI.org. Retrieved 2011-09-02.
- ↑ Dumoulin C, Hay-Smith J (14 May 2014). "Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women". Cochrane Database of Systematic Reviews. 2014 (5): CD005654. doi:10.1002/14651858.CD005654.pub3. PMID 24823491.
- ↑ Herderschee R, Hay-Smith EJ, Herbison GP, Roovers JP, Heineman MJ (6 July 2011). "Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women.". The Cochrane Database of Systematic Reviews (7): CD009252. doi:10.1002/14651858.CD009252. PMID 21735442.
- ↑ Hagen S, Stark D (2011). "Conservative prevention and management of pelvic organ prolapse in women". Cochrane Database Syst Rev. 12 (12): CD003882. doi:10.1002/14651858.CD003882.pub4. PMID 22161382.
- ↑ Herderschee, R; Hay-Smith, EJ; Herbison, GP; Roovers, JP; Heineman, MJ (6 July 2011). "Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women.". The Cochrane database of systematic reviews (7): CD009252. PMID 21735442.
- ↑ "Do the Kegel - Dr Arnold Kegel". Archived from the original on 26 October 2010. Retrieved 4 July 2012.
- ↑ Campbell SE, Glazener CM, Hunter KF, Cody JD, Moore KN (2012). "Conservative management for postprostatectomy urinary incontinence". Cochrane Database Syst Rev. 1: CD001843. doi:10.1002/14651858.CD001843.pub4. PMID 22258946.
- ↑ Dorey, Grace; Speakman, Mark J.; Feneley, Roger C.L.; Swinkels, Annette; Dunn, Christopher D.R. (2005). "Pelvic floor exercises for erectile dysfunction". BJU International. 96 (4): 595–7. doi:10.1111/j.1464-410X.2005.05690.x. PMID 16104916.
- ↑ "Management of premature Ejaculation, Baum and Spiedler, Medical concepts of human sexuality 2001" (PDF). Retrieved 2011-09-02.
- ↑ September 2, 2011 (2011-02-09). "Vaginal Prolapse". eMedicineHealth. Retrieved 2011-09-02.
- ↑ "MedlinePlus Medical Encyclopedia: Uterine prolapse". Nlm.nih.gov. 2011-08-29. Retrieved 2011-09-02.
- ↑ Kenway, M., and Goh, J. (2009). Inside Out: The Essential Women's Guide to Pelvic Support.
- ↑ Bø, K (2006). "Can pelvic floor muscle training prevent and treat pelvic organ prolapse?". Acta Obstet Gynecol Scand. 85 (3): 263–8. doi:10.1080/00016340500486800. PMID 16553172.
- ↑ http://kegelmaster.com.au/why-the-kegelmaster-was-invented/
- ↑ "Kegel exercises: A how-to guide for women". Mayo Clinic. July 10, 2010. Retrieved July 4, 2012.
External links
- Judith Florendo, PT. Kegels De-Mystified for Women. A Healthy Balance (National Association for Continence) Fall 2008 Vol 26 No 3
- MayoClinic.com. Kegel exercises: how to strengthen pelvic floor muscles
- Kegel Exercises: Treating Male Urinary Incontinence