Diabetes mellitus type 1
| Diabetes type 1 | |
|---|---|
| T1D, insulin-dependent diabetes,[1] juvenile diabetes[2] | |
|
A blue circle, the symbol for diabetes.[3] | |
| Classification and external resources | |
| Pronunciation | /daɪəbiːtiːs/ |
| Specialty | Endocrinology |
| ICD-10 | E10 |
| ICD-9-CM | 250.01 |
| OMIM | 222100 |
| DiseasesDB | 3649 |
| MedlinePlus | 000305 |
| eMedicine | med/546 |
| MeSH | D003922 |
Diabetes mellitus type 1 (also known as type 1 diabetes) is a form of diabetes mellitus in which not enough insulin is produced.[4] The lack of insulin results in high blood sugar levels.[1] The classical symptoms are frequent urination, increased thirst, increased hunger, and weight loss.[4] Additional symptoms may include blurry vision, feeling tired, and poor healing.[2] Symptoms typically develop over a short period of time.[1]
The cause of type 1 diabetes is unknown.[4] It however is believed to involve a combination of genetic and environmental factors.[1] Risk factors include having a family member with the condition.[5] The underlying mechanism involves an autoimmune destruction of the insulin-producing beta cells in the pancreas.[2] Diabetes is diagnosed by testing the level of sugar or A1C in the blood.[6][5] Type 1 diabetes may be distinguished from type 2 by autoantibody testing.[5]
There is no way to prevent type 1 diabetes.[4] Treatment with insulin is typically required for survival.[1] Insulin therapy is usually given by injection just under the skin but can also be delivered by an insulin pump.[7] A diabetic diet and exercise are an important part of management.[2] Untreated, diabetes can cause many complications.[4] Complications of relatively rapid onset include diabetic ketoacidosis and nonketotic hyperosmolar coma.[5] Long-term complications include heart disease, stroke, kidney failure, foot ulcers and damage to the eyes.[4] Furthermore, complications may arise from low blood sugar caused by excessive insulin treatment.[5]
Type 1 diabetes makes up an estimated 5–10% of all diabetes cases.[8] The number of people affected globally is unknown, although it is estimated that about 80,000 children develop the disease each year.[5] Within the United States the number of people affected is estimated at one to three million.[5][9] Rates of disease vary widely with approximately 1 new case per 100,000 per year in East Asia and Latin America and around 30 new cases per 100,000 per year in Scandinavia and Kuwait.[10][11] It typically begins in children and young adults.[1]
Signs and symptoms
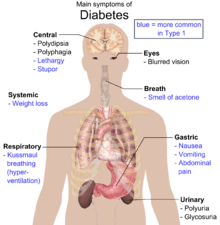
The classical symptoms of type 1 diabetes include: polyuria (excessive urination), polydipsia (increased thirst), dry mouth, polyphagia (increased hunger), fatigue, and weight loss.[4]
Many type 1 diabetics are diagnosed when they present with diabetic ketoacidosis. The signs and symptoms of diabetic ketoacidosis include dry skin, rapid deep breathing, drowsiness, increased thirst, frequent urination, abdominal pain, and vomiting.[12]
About 12 percent of people with type 1 diabetes have clinical depression.[13]
About 6 percent of people with type 1 diabetes have celiac disease, but in most cases there are no digestive symptoms[14][15] or are mistakenly attributed to poor control of diabetes, gastroparesis or diabetic neuropathy.[14] In most cases, celiac disease is diagnosed after onset of type 1 diabetes. The association of celiac disease with type 1 diabetes increases the risk of complications, such as retinopathy and mortality. This association can be explained by shared genetic factors, and inflammation or nutritional deficiencies caused by untreated celiac disease, even if type 1 diabetes is diagnosed first.[15]
Cause
The cause of type 1 diabetes is unknown.[4] A number of explanatory theories have been put forward, and the cause may be one or more of the following: genetic susceptibility, a diabetogenic trigger, and exposure to an antigen.[16]
Genetics
Type 1 diabetes is a disease that involves many genes. The risk of a child developing type 1 diabetes is about 5% if the father has it, about 8% if a sibling has it, about 3% if the mother has type 1 diabetes.[17] If one identical twin is affected there is about a 50% chance the other will also be affected.[18] Some studies of heritability has estimated it at 80 to 86%.[19][20]
More than 50 genes are associated with type 1 diabetes.[21] Depending on locus or combination of loci, they can be dominant, recessive, or somewhere in between. The strongest gene, IDDM1, is located in the MHC Class II region on chromosome 6, at staining region 6p21. Certain variants of this gene increase the risk for decreased histocompatibility characteristic of type 1. Such variants include DRB1 0401, DRB1 0402, DRB1 0405, DQA 0301, DQB1 0302 and DQB1 0201, which are common in North Americans of European ancestry and in Europeans.[22] Some variants also appear to be protective.[22]
Environmental
Environmental factors can influence expression of type 1. For identical twins, when one twin has type 1 diabetes, the other twin only has it 30%–50% of the time. Thus for 50%-70% of identical twins where one has the disease, the other will not, despite having exactly the same genome; this suggests environmental factors, in addition to genetic factors, can influence the disease's prevalence.[23] Other indications of environmental influence include the presence of a 10-fold difference in occurrence among Caucasians living in different areas of Europe, and that people tend to acquire the rate of disease of their particular destination country.[16]
Virus
One theory proposes that type 1 diabetes is a virus-triggered autoimmune response in which the immune system attacks virus-infected cells along with the beta cells in the pancreas.[24][25] Several viruses have been implicated, including enteroviruses (especially coxsackievirus B), cytomegalovirus, Epstein–Barr virus, mumps virus, rubella virus and rotavirus, but to date there is no stringent evidence to support this hypothesis in humans.[26] A 2011 systematic review and meta-analysis showed an association between enterovirus infections and type 1 diabetes, but other studies have shown that, rather than triggering an autoimmune process, enterovirus infections, as coxsackievirus B, could protect against onset and development of type 1 diabetes.[27]
Chemicals and drugs
Some chemicals and drugs selectively destroy pancreatic cells. Pyrinuron (Vacor), a rodenticide introduced in the United States in 1976, selectively destroys pancreatic beta cells, resulting in type 1 diabetes after accidental poisoning.[28] Pyrinuron was withdrawn from the U.S. market in 1979 and it is not approved by the Environmental Protection Agency for use in the U.S.[29] Streptozotocin (Zanosar), an antineoplastic agent, is selectively toxic to the beta cells of the pancreatic islets. It is used in research for inducing type 1 diabetes on rodents[30] and for treating metastatic cancer of the pancreatic islet cells in patients whose cancer cannot be removed by surgery.[31] Other pancreatic problems, including trauma, pancreatitis, or tumors (either malignant or benign) can also lead to loss of insulin production.
Gluten
Data suggest that gliadin (a protein present in gluten) may play a role in the development of type 1 diabetes, but the mechanism is not fully understood.[32][33] Increased intestinal permeability caused by gluten and the subsequent loss of intestinal barrier function, which allows the passage of pro-inflammatory substances into the blood, may induce the autoimmune response in genetically predisposed individuals to type 1 diabetes.[15][33] Early introduction of gluten-containing cereals in the diet increases the risk of developing islet cell autoantibodies, which are responsible for the destruction of the insulin-producing beta cells in the pancreas.[33]
Pathophysiology
The pathophysiology in diabetes type 1 is a destruction of beta cells in the pancreas, regardless of which risk factors or causative entities have been present.
Individual risk factors can have separate pathophysiological processes to, in turn, cause this beta cell destruction. Still, a process that appears to be common to most risk factors is an autoimmune response towards beta cells, involving an expansion of autoreactive CD4+ T helper cells and CD8+ T cells, autoantibody-producing B cells and activation of the innate immune system.[22][34]
After starting treatment with insulin a person's own insulin levels may temporarily improve.[35] This is believed to be due to altered immunity and is known as the "honeymoon phase".[35]
Diagnosis
| Condition | 2 hour glucose | Fasting glucose | HbA1c | |
|---|---|---|---|---|
| Unit | mmol/l(mg/dl) | mmol/l(mg/dl) | mmol/mol | DCCT % |
| Normal | <7.8 (<140) | <6.1 (<110) | <42 | <6.0 |
| Impaired fasting glycaemia | <7.8 (<140) | ≥6.1(≥110) & <7.0(<126) | 42-46 | 6.0–6.4 |
| Impaired glucose tolerance | ≥7.8 (≥140) | <7.0 (<126) | 42-46 | 6.0–6.4 |
| Diabetes mellitus | ≥11.1 (≥200) | ≥7.0 (≥126) | ≥48 | ≥6.5 |
Diabetes mellitus is characterized by recurrent or persistent hyperglycemia, and is diagnosed by demonstrating any one of the following:[38]
- Fasting plasma glucose level at or above 7.0 mmol/L (126 mg/dL).
- Plasma glucose at or above 11.1 mmol/L (200 mg/dL) two hours after a 75 g oral glucose load as in a glucose tolerance test.
- Symptoms of hyperglycemia and casual plasma glucose at or above 11.1 mmol/L (200 mg/dL).
- Glycated hemoglobin (hemoglobin A1C) at or above 48 mmol/mol (≥ 6.5 DCCT %). (This criterion was recommended by the American Diabetes Association in 2010, although it has yet to be adopted by the WHO.)[39]
About a quarter of people with new type 1 diabetes have developed some degree of diabetic ketoacidosis (a type of metabolic acidosis which is caused by high concentrations of ketone bodies, formed by the breakdown of fatty acids and the deamination of amino acids) by the time the diabetes is recognized. The diagnosis of other types of diabetes is usually made in other ways. These include ordinary health screening, detection of hyperglycemia during other medical investigations, and secondary symptoms such as vision changes or unexplained fatigue. Diabetes is often detected when a person suffers a problem that may be caused by diabetes, such as a heart attack, stroke, neuropathy, poor wound healing or a foot ulcer, certain eye problems, certain fungal infections, or delivering a baby with macrosomia or hypoglycemia (low blood sugar).
A positive result, in the absence of unequivocal hyperglycemia, should be confirmed by a repeat of any of the above-listed methods on a different day. Most physicians prefer to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete and offers no prognostic advantage over the fasting test.[40] According to the current definition, two fasting glucose measurements above 126 mg/dL (7.0 mmol/L) is considered diagnostic for diabetes mellitus.
In type 1, pancreatic beta cells in the islets of Langerhans are destroyed, decreasing endogenous insulin production. This distinguishes type 1's origin from type 2. Type 2 diabetes is characterized by insulin resistance, while type 1 diabetes is characterized by insulin deficiency, generally without insulin resistance. Another hallmark of type 1 diabetes is islet autoreactivity, which is generally measured by the presence of autoantibodies directed towards the beta cells.
Autoantibodies
The appearance of diabetes-related autoantibodies has been shown to be able to predict the appearance of diabetes type 1 before any hyperglycemia arises, the main ones being islet cell autoantibodies, insulin autoantibodies, autoantibodies targeting the 65-kDa isoform of glutamic acid decarboxylase (GAD), autoantibodies targeting the phosphatase-related IA-2 molecule, and zinc transporter autoantibodies (ZnT8).[16] By definition, the diagnosis of diabetes type 1 can be made first at the appearance of clinical symptoms and/or signs, but the emergence of autoantibodies may itself be termed "latent autoimmune diabetes". Not everyone with autoantibodies progresses to diabetes type 1, but the risk increases with the number of antibody types, with three to four antibody types giving a risk of progressing to diabetes type 1 of 60%–100%.[16] The time interval from emergence of autoantibodies to clinically diagnosable diabetes can be a few months in infants and young children, but in some people it may take years – in some cases more than 10 years.[16] Islet cell autoantibodies are detected by conventional immunofluorescence, while the rest are measured with specific radiobinding assays.[16]
Prevention
Type 1 diabetes is not currently preventable.[41] Some researchers believe it might be prevented at the latent autoimmune stage, before it starts destroying beta cells.[22]
Immunosuppressive drugs
Cyclosporine A, an immunosuppressive agent, has apparently halted destruction of beta cells (on the basis of reduced insulin usage), but its kidney toxicity and other side effects make it highly inappropriate for long-term use.[22]
Anti-CD3 antibodies, including teplizumab and otelixizumab, had suggested evidence of preserving insulin production (as evidenced by sustained C-peptide production) in newly diagnosed type 1 diabetes patients.[22] A probable mechanism of this effect was believed to be preservation of regulatory T cells that suppress activation of the immune system and thereby maintain immune system homeostasis and tolerance to self-antigens.[22] The duration of the effect is still unknown, however.[22] In 2011, Phase III studies with otelixizumab and teplizumab both failed to show clinical efficacy, potentially due to an insufficient dosing schedule.[42][43]
An anti-CD20 antibody, rituximab, inhibits B cells and has been shown to provoke C-peptide responses three months after diagnosis of type 1 diabetes, but long-term effects of this have not been reported.[22]
Diet
Some research has suggested breastfeeding decreases the risk in later life[44][45] and early introduction of gluten-containing cereals in the diet increases the risk of developing islet cell autoantibodies;[33] various other nutritional risk factors are being studied, but no firm evidence has been found.[46] Giving children 2000 IU of vitamin D daily during their first year of life is associated with reduced risk of type 1 diabetes, though the causal relationship is obscure.[47]
Children with antibodies to beta cell proteins (i.e. at early stages of an immune reaction to them) but no overt diabetes, and treated with niacinamide (vitamin B3), had less than half the diabetes onset incidence in a seven-year time span than did the general population, and an even lower incidence relative to those with antibodies as above, but who received no niacinamide.[48]
People with type 1 diabetes and undiagnosed celiac disease have worse glycaemic control and a higher prevalence of nephropathy and retinopathy. Gluten-free diet, when performed strictly, improves diabetes symptoms and appears to have a protective effect against developing long-term complications. Nevertheless, dietary management of both these diseases is challenging and these patients have poor compliance of the diet.[49]
Management
Lifestyle
A low-carbohydrate diet, in addition to medications, is useful in type 1 DM.[50] There are camps for children to teach them how and when to use or monitor their insulin without parental help.[51] As psychological stress may have a negative effect on diabetes, a number of measures have been recommended including: exercising, taking up a new hobby, or joining a charity among others.[52]
Insulin
There are four main types of insulin: rapid acting insulin, short acting insulin, intermediate acting insulin, and long acting insulin. The rapid acting insulin is used as a bolus dosage. The action onsets in 15 minutes with peak actions in 30 to 90 minutes. Short acting insulin action onsets within 30 minutes with the peak action around 2 to 4 hours. Intermediate acting insulin action onsets within 1 to 2 hours with peak action of 4 to 10 hours. Long acting insulin is usually given once per day. The action onset is roughly 1 to 2 hours with a sustained action of up to 24 hours.
Injections of insulin—either via subcutaneous injection or insulin pump— are necessary for those living with type 1 diabetes because it cannot be treated by diet and exercise alone.[53] In addition to insulin therapy dietary management is important. This includes keeping track of the carbohydrate content of food and careful monitoring of blood glucose levels using glucose meters. Today, the most common insulins are biosynthetic products produced using genetic recombination techniques; formerly, cattle or pig insulins were used, and even sometimes insulin from fish.[54]
Untreated type 1 diabetes can commonly lead to diabetic ketoacidosis which is a diabetic coma which can be fatal if untreated.[55] Diabetic ketoacidosis can cause cerebral edema (accumulation of liquid in the brain). This is a life-threatening issue and children are at a higher risk for cerebral edema than adults, causing ketoacidosis to be the most common cause of death in pediatric diabetes.[56]
Treatment of diabetes focuses on lowering blood sugar or glucose (BG) to the near normal range, approximately 80–140 mg/dl (4.4–7.8 mmol/L).[57] The ultimate goal of normalizing BG is to avoid long-term complications that affect the nervous system (e.g. peripheral neuropathy leading to pain and/or loss of feeling in the extremities), and the cardiovascular system (e.g. heart attacks, vision loss). This level of control over a prolonged period of time can be varied by a target HbA1c level of less than 7.5%.[5]
People with type 1 diabetes always need to use insulin, but treatment can lead to low BG (hypoglycemia), i.e. BG less than 70 mg/dl (3.9 mmol/l). Hypoglycemia is a very common occurrence in people with diabetes, usually the result of a mismatch in the balance among insulin, food and physical activity. Mild cases are self-treated by eating or drinking something high in sugar. Severe cases can lead to unconsciousness and are treated with intravenous glucose or injections with glucagon. Continuous glucose monitors can alert patients to the presence of dangerously high or low blood sugar levels, but technical issues have limited the effect these devices have had on clinical practice.
As of 2016 an artificial pancreas looks promising with safety issues still being studied.[58]
Pancreas transplantation
In some cases, a pancreas transplant can restore proper glucose regulation. However, the surgery and accompanying immunosuppression required may be more dangerous than continued insulin replacement therapy, so is generally only used with or some time after a kidney transplant. One reason for this is that introducing a new kidney requires taking immunosuppressive drugs such as cyclosporine. Nevertheless, this allows the introduction of a new pancreas to a person with diabetes without any additional immunosuppressive therapy. However, pancreas transplants alone may be beneficial in people with extremely labile type 1 diabetes mellitus.[59]
Islet cell transplantation
Islet cell transplantation may be an option for some people with type 1 diabetes that are not well controlled with insulin.[60] Difficulties include finding donors that are a compatible, getting the new islets to survive, and the side effects from the medications used to prevent rejection.[60] Success rates, defined as not needing insulin at 3 years follow the procedure occurred in 44% in on registry from 2010.[60]
Complications
Complications of poorly managed type 1 diabetes mellitus may include cardiovascular disease, diabetic neuropathy, and diabetic retinopathy, among others. However, cardiovascular disease[61] as well as neuropathy[62] may have an autoimmune basis, as well. Women with type 1 DM have a 40% higher risk of death as compared to men with type 1 DM.[63] The life expectancy of an individual with type 1 diabetes is 11 years less for men and 14 years less for women.[64]
Urinary tract infection
People with diabetes show an increased rate of urinary tract infection.[65] The reason is bladder dysfunction that is more common in diabetics than in non-diabetics due to diabetic nephropathy. When present, nephropathy can cause a decrease in bladder sensation, which in turn, can cause increased residual urine, a risk factor for urinary tract infections.[66]
Sexual dysfunction
Sexual dysfunction in diabetics is often a result of physical factors such as nerve damage and/or poor circulation, and psychological factors such as stress and/or depression caused by the demands of the disease.[67][68]
Males
The most common sexual issues in diabetic males are problems with erections and ejaculation: "With diabetes, blood vessels supplying the penis’s erectile tissue can get hard and narrow, preventing the adequate blood supply needed for a firm erection. The nerve damage caused by poor blood glucose control can also cause ejaculate to go into the bladder instead of through the penis during ejaculation, called retrograde ejaculation. When this happens, semen leaves the body in the urine."[67] Another cause for erectile dysfunction are the reactive oxygen species created as a result of the disease. Antioxidants can be used to help combat this.[69]
Females
While there is less material on the correlation between diabetes and female sexual dysfunction than male sexual dysfunction, studies have shown there to be a significant prevalence of sexual problems in diabetic women.[68] Common problems include reduced sensation in the genitals, dryness, difficulty/inability to orgasm, pain during sex, and decreased libido.[67] In some cases diabetes has been shown to decrease oestrogen levels in females, which can affect vaginal lubrication.[68]
Oral contraceptives can be taken by diabetics. Sometimes, contraceptive pills can cause a blood sugar imbalance, but this usually can be corrected by a dosage change.[68] As with any medication, side effects should be taken into account and monitored to prevent serious complications with diabetes.[68]
Women with type 1 diabetes show a higher than normal rate of polycystic ovarian syndrome (PCOS).[70] The reason may be that the ovaries are exposed to high insulin concentrations since women with type 1 diabetes can have frequent hyperglycemia.[71]
Epidemiology
Type 1 diabetes makes up an estimated 5–10% of all diabetes cases[8] or 11–22 million worldwide.[41] In 2006 it affected 440,000 children under 14 years of age and was the primary cause of diabetes in those less than 10 years of age.[72] The incidence of type 1 diabetes has been increasing by about 3% per year.[72]
Rates vary widely by country. In Finland, the incidence is a high of 57 per 100,000 per year, in Japan and China a low of 1 to 3 per 100,000 per year, and in Northern Europe and the U.S., an intermediate of 8 to 17 per 100,000 per year.[73][74]
In the United States, type 1 diabetes affected about 208,000 youths under the age of 20 in 2015. Over 18,000 youths are diagnosed with Type 1 diabetes every year. Compared to non-Hispanic whites, Asian Americans, Hispanic Americans and Hispanic-Black Americans have greater odds of being diagnosed with diabetes. Every year about 234,051 Americans die due to diabetes or diabetes-related complications, with 69,071 having it as the primary cause of death.[75]
History
Type 1 diabetes was described as an autoimmune disease in the 1970s, based on observations that autoantibodies against islets were discovered in diabetics with other autoimmune deficiencies.[76] It was also shown in the 1980s that immunosuppressive therapies could slow disease progression, further supporting the idea that type 1 diabetes is an autoimmune disorder.[77] The name juvenile diabetes was used earlier as it often first is diagnosed in childhood.
In Australia, approximately one million Australians have been diagnosed with type 1 diabetes and Australia ranks 7th-highest in the world with children under 14 years of age. Between 2000 and 2013, 31,895 new cases were established, with 2,323 in 2013, a rate of 10–13 cases per 100,00 people each year. Aboriginals and Torres Strait Islander people are less affected.[78][79]
Society and culture
The disease was estimated to cause $10.5 billion in annual medical costs ($875 per month per diabetic) and an additional $4.4 billion in indirect costs ($366 per month per person with diabetes) in the U.S.[80] In the United States $245 billion every year is attributed to diabetes. Individuals diagnosed with diabetes have 2.3 times the health care costs as individuals who do not have diabetes. One in 10 health care dollars are spent on individuals with diabetes.[75]
Research
Funding for research into type 1 diabetes originates from government, industry (e.g., pharmaceutical companies), and charitable organizations. Government funding in the United States is distributed via the National Institute of Health, and in the UK via the National Institute for Health Research or the Medical Research Council. JDRF, originally founded by parents of children with type 1 diabetes, is the world's largest provider of charity based funding for type 1 diabetes research. Other charities include the American Diabetes Association, Diabetes UK, Diabetes Research and Wellness Foundation,[81] Diabetes Australia, the Canadian Diabetes Association.
Treatments
A number of approaches have been explored to provide treatments for type 1.
Stem cells
Pluripotent stem cells can be used to generate beta cells but previously these cells did not function as well as normal beta cells.[82] In 2014 more mature beta cells were produced which released insulin in response to blood sugar when transplanted into mice.[83][84] Before these techniques can be used in humans more evidence of safety and effectiveness is needed.[82]
Vaccine
Vaccines to treat or prevent Type 1 diabetes are designed to induce immune tolerance to insulin or pancreatic beta cells.[85] While Phase II clinical trials of a vaccine containing alum and recombinant GAD65, an autoantigen involved in type 1 diabetes, were promising, as of 2014 Phase III had failed.[85] As of 2014, other approaches, such as a DNA vaccine encoding proinsulin and a peptide fragment of insulin, were in early clinical development.[85]
Diet
There is evidence from experiments conducted in animal models that removal of gluten from the diet may prevent the onset type 1 diabetes[32][86] but there has been conflicting research in humans.[86]
Labile diabetes
Insulin-dependent diabetes characterized by dramatic and recurrent swings in glucose levels, often occurring for no apparent reason, is sometimes known as brittle diabetes, unstable diabetes or labile diabetes, although some experts say the "brittle diabetes" concept "has no biologic basis and should not be used".[87] The results of such swings can be irregular and unpredictable hyperglycemias, sometimes involving ketoacidosis, and sometimes serious hypoglycemias. Brittle diabetes occurs no more frequently than in 1% to 2% of diabetics.[88] In a small study, 10 of 20 brittle diabetic patients aged 18–23 years who could be traced had died within 22 years, and the remainder, though suffering high rates of complications, were no longer brittle.[89] These results were similar to those of an earlier study by the same authors which found a 19% mortality in 26 patients after 10.5 years.[90]
Because labile diabetes is defined as "episodes of hypoglycemia or hyperglycemia that, whatever their cause, constantly disrupt a patient's life", it can have many causes, some of which include:[91]
- errors in diabetes management, which can include too much insulin being given, in relation to carbohydrate being consumed
- interactions with other medical conditions
- psychological problems
- biological factors that interfere with how insulin is processed within the body
- hypoglycemia and hyperglycemia due to strenuous exercise; however, hypoglycemia is more frequent
- insulin exposed to higher temperatures that reduces effectiveness of the insulin hormone in the body
- spontaneous production of insulin in the body due to activity in the beta cells during the period shortly after diagnosis of type 1 diabetes
Exercise related hyperglycemia is caused when hormones (such as adrenaline and cortisol) are released during moderate to strenuous exercise. This happens when the muscles signal the liver to release glucose into the bloodstream by converting stored glycogen into glucose. The cause of exercise related hypoglycemia, on the other hand, occurs when the muscle group being exercised uses up glucose faster than it can be replenished by the body.
One of these biological factors is the production of insulin autoantibodies. High antibody titers can cause episodes of hyperglycemia by neutralizing the insulin, thereby causing clinical insulin resistance requiring doses of over 200 IU/day. However, antibodies may also fail to buffer the release of the injected insulin into the bloodstream after subcutaneous injection, resulting in episodes of hypoglycemia. In some cases, changing the type of insulin administered can resolve this problem.[91] There have been a number of reports that insulin autoantibodies can act as a "sink" for insulin and affect the time to peak, half-life, distribution space, and metabolic clearance, though in most patients these effects are small.[92]
References
- 1 2 3 4 5 6 "Causes of Diabetes". NIDDK. August 2014. Retrieved 31 July 2016.
- 1 2 3 4 "Types of Diabetes". NIDDK. February 2014. Retrieved 31 July 2016.
- ↑ "Diabetes Blue Circle Symbol". International Diabetes Federation. 17 March 2006.
- 1 2 3 4 5 6 7 8 "Diabetes Fact sheet N°312". WHO. June 2016. Retrieved 31 July 2016.
- 1 2 3 4 5 6 7 8 Chiang, J. L.; Kirkman, M. S.; Laffel, L. M. B.; Peters, A. L. (16 June 2014). "Type 1 Diabetes Through the Life Span: A Position Statement of the American Diabetes Association". Diabetes Care. 37 (7): 2034–2054. doi:10.2337/dc14-1140. PMID 24935775.
- ↑ "Diagnosis of Diabetes and Prediabetes". NIDDK. May 2015. Retrieved 31 July 2016.
- ↑ "Alternative Devices for Taking Insulin". NIDDK. July 2016. Retrieved 31 July 2016.
- 1 2 Daneman D (11 March 2006). "Type 1 diabetes". Lancet. 367 (9513): 847–58. doi:10.1016/S0140-6736(06)68341-4. PMID 16530579.
- ↑ "FAST FACTS Data and Statistics about Diabetes". American Diabetes Association. Retrieved 25 July 2014.
- ↑ Global report on diabetes (PDF). World Health Organization. 2016. p. 26-27. ISBN 978-92-4-156525-7. Retrieved 31 July 2016.
- ↑ Skyler, Jay (2012). Atlas of diabetes (4th ed.). New York: Springer. p. 67-68. ISBN 978-1-4614-1028-7.
- ↑ "webmd Symptoms Type I Diabetes".
- ↑ Roy T, Lloyd CE (2012). "Epidemiology of depression and diabetes: a systematic review". J Affect Disord. 142 Suppl: S8–21. doi:10.1016/S0165-0327(12)70004-6. PMID 23062861.
- 1 2 See JA, Kaukinen K, Makharia GK, Gibson PR, Murray JA (Oct 2015). "Practical insights into gluten-free diets". Nat Rev Gastroenterol Hepatol (Review). 12 (10): 580–91. doi:10.1038/nrgastro.2015.156. PMID 26392070.
Coeliac disease in T1DM is asymptomatic ...Clinical manifestations of coeliac disease, such as abdominal pain, gas, bloating, diarrhoea and weight loss can be present in patients with T1DM, but are often attributed to poor control of diabetes, gastroparesis or diabetic neuropathy
- 1 2 3 Elfström P, Sundström J, Ludvigsson JF (2014). "Systematic review with meta-analysis: associations between coeliac disease and type 1 diabetes.". Aliment Pharmacol Ther. 40 (10): 1123–32. doi:10.1111/apt.12973. PMID 25270960.
- 1 2 3 4 5 6 Knip M, Veijola R, Virtanen SM, Hyöty H, Vaarala O, Akerblom HK (2005). "Environmental Triggers and Determinants of Type 1 Diabetes". Diabetes. 54: S125–S136. doi:10.2337/diabetes.54.suppl_2.S125. PMID 16306330.
- ↑ Pociot, F; Lernmark, Å (4 June 2016). "Genetic risk factors for type 1 diabetes.". Lancet (London, England). 387 (10035): 2331–9. PMID 27302272.
- ↑ Owen, Katharine (2014). Oxford Handbook of Endocrinology and Diabetes. Oxford University Press. p. 690. ISBN 9780199644438.
- ↑ Narayan, K. M. Venkat; Williams, Desmond; Gregg, Edward W.; Cowie, Catherine C. (2010). Diabetes Public Health: From Data to Policy. Oxford University Press. p. 671. ISBN 9780199749140.
- ↑ Melmed, Shlomo; Polonsky, Kenneth S.; Larsen, P. Reed; Kronenberg, Henry (2015). Williams Textbook of Endocrinology. Elsevier Health Sciences. p. 50. ISBN 9780323297387.
- ↑ Ionescu-Tîrgovişte, Constantin; Gagniuc, Paul Aurelian; Guja, Cristian. "Structural Properties of Gene Promoters Highlight More than Two Phenotypes of Diabetes". PLOS ONE. 10 (9): e0137950. doi:10.1371/journal.pone.0137950. PMC 4574929
 . PMID 26379145.
. PMID 26379145. - 1 2 3 4 5 6 7 8 9 Bluestone JA, Herold K, Eisenbarth G (2010). "Genetics, pathogenesis and clinical interventions in type 1 diabetes". Nature. 464 (7293): 1293–1300. Bibcode:2010Natur.464.1293B. doi:10.1038/nature08933. PMID 20432533.
- ↑ "OMIM Entry – %222100 – DIABETES MELLITUS, INSULIN-DEPENDENT; IDDM". Ncbi.nlm.nih.gov. Retrieved 29 November 2011.
- ↑ Rewers M, Ludvigsson J (2016). "Environmental risk factors for type 1 diabetes.". Lancet (Review). 387 (10035): 2340–8. doi:10.1016/S0140-6736(16)30507-4. PMID 27302273.
- ↑ Fairweather D, Rose NR (2002). "Type 1 diabetes: virus infection or autoimmune disease?". Nat. Immunol. 3 (4): 338–40. doi:10.1038/ni0402-338. PMID 11919574.
- ↑ Petzold A; Solimena M; Knoch KP (2015). "Mechanisms of Beta Cell Dysfunction Associated With Viral Infection.". Curr Diab Rep (Review). 15 (10): 73. doi:10.1007/s11892-015-0654-x. PMC 4539350
 . PMID 26280364.
. PMID 26280364. So far, none of the hypotheses accounting for virus-induced beta cell autoimmunity has been supported by stringent evidence in humans, and the involvement of several mechanisms rather than just one is also plausible.
- ↑ Butalia S, Kaplan GG, Khokhar B, Rabi DM (Aug 18, 2016). "Environmental Risk Factors and Type 1 Diabetes: Past, Present, and Future". Can J Diabetes (Review). pii: S1499-2671(15)30052–6. doi:10.1016/j.jcjd.2016.05.002. PMID 27545597.
- ↑ Thayer KA, Heindel JJ, Bucher JR, Gallo MA (Jun 2012). "Role of environmental chemicals in diabetes and obesity: a National Toxicology Program workshop review". Environ Health Perspect (Review). 120 (6): 779–89. doi:10.1289/ehp.1104597. PMC 3385443
 . PMID 22296744.
. PMID 22296744. - ↑ "Pyriminil". Pyriminil. U.S. National Library of Medicine.
- ↑ Wu J, Yan LJ (Apr 2015). "Streptozotocin-induced type 1 diabetes in rodents as a model for studying mitochondrial mechanisms of diabetic β cell glucotoxicity". Diabetes Metab Syndr Obes (Review). 8: 181–8. doi:10.2147/DMSO.S82272. PMC 4396517
 . PMID 25897251.
. PMID 25897251. - ↑ Brentjens R, Saltz L (2001). "Islet cell tumors of the pancreas: the medical oncologist's perspective". Surg Clin North Am (Review). 81 (3): 527–42. doi:10.1016/S0039-6109(05)70141-9. PMID 11459269.
- 1 2 Serena G, Camhi S, Sturgeon C, Yan S, Fasano A (2015). "The Role of Gluten in Celiac Disease and Type 1 Diabetes.". Nutrients. 7 (9): 7143–62. doi:10.3390/nu7095329. PMC 4586524
 . PMID 26343710.
. PMID 26343710. 
- 1 2 3 4 Visser J, Rozing J, Sapone A, Lammers K, Fasano A (2009). "Tight junctions, intestinal permeability, and autoimmunity: celiac disease and type 1 diabetes paradigms.". Ann N Y Acad Sci. 1165: 195–205. doi:10.1111/j.1749-6632.2009.04037.x. PMC 2886850
 . PMID 19538307.
. PMID 19538307. - ↑ Chatzigeorgiou A, Harokopos V, Mylona-Karagianni C, Tsouvalas E, Aidinis V, Kamper EF (September 2010). "The pattern of inflammatory/anti-inflammatory cytokines and chemokines in type 1 diabetic patients over time". Ann. Med. 42 (6): 426–38. doi:10.3109/07853890.2010.495951. PMID 20568978.
- 1 2 Aly H, Gottlieb P (Aug 2009). "The honeymoon phase: intersection of metabolism and immunology.". Current opinion in endocrinology, diabetes, and obesity. 16 (4): 286–92. doi:10.1097/med.0b013e32832e0693. PMID 19506474.
- ↑ Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation (PDF). Geneva: World Health Organization. 2006. p. 21. ISBN 978-92-4-159493-6.
- ↑ Vijan, S (March 2010). "Type 2 diabetes". Annals of Internal Medicine. 152 (5): ITC31-15. doi:10.7326/0003-4819-152-5-201003020-01003. PMID 20194231.
- ↑ World Health Organisation Department of Noncommunicable Disease Surveillance (1999). "Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications" (PDF).
- ↑ ""Diabetes Care" January 2010". American Diabetes Association. Retrieved 29 January 2010.
- ↑ Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL (August 2001). "Postchallenge hyperglycemia and mortality in a national sample of U.S. adults". Diabetes Care. 24 (8): 1397–402. doi:10.2337/diacare.24.8.1397. PMID 11473076.
- 1 2 "Diabetes". World Health Organization. Retrieved 24 January 2011.
- ↑ "''Tolerx, Inc. and GlaxoSmithKline (GSK) Announce Phase 3 Defend-1 Study of Otelixizumab in Type 1 Diabetes Did Not Meet Its Primary Endpoint''". Biospace. Retrieved 29 November 2011.
- ↑ "Macrogenics press release: ''MacroGenics and Lilly Announce Pivotal Clinical Trial of Teplizumab Did Not Meet Primary Efficacy Endpoint''". Macrogenics.com. 20 October 2010. Retrieved 29 November 2011.
- ↑ Borch-Johnsen K, Joner G, Mandrup-Poulsen T, Christy M, Zachau-Christiansen B, Kastrup K, Nerup J (November 1984). "Relation between breast-feeding and incidence rates of insulin-dependent diabetes mellitus. A hypothesis". Lancet. 2 (8411): 1083–6. doi:10.1016/S0140-6736(84)91517-4. PMID 6150150.
- ↑ Shehadeh N, Shamir R, Berant M, Etzioni A (2001). "Insulin in human milk and the prevention of type 1 diabetes". Pediatric Diabetes. 2 (4): 175–7. doi:10.1034/j.1399-5448.2001.20406.x. PMID 15016183.
- ↑ Virtanen SM, Knip M (December 2003). "Nutritional risk predictors of beta cell autoimmunity and type 1 diabetes at a young age". The American Journal of Clinical Nutrition. 78 (6): 1053–67. PMID 14668264.
- ↑ Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM (November 2001). "Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study". Lancet. 358 (9292): 1500–3. doi:10.1016/S0140-6736(01)06580-1. PMID 11705562.
- ↑ Elliott RB, Pilcher CC, Fergusson DM, Stewart AW (1996). "A population based strategy to prevent insulin-dependent diabetes using nicotinamide". Journal of Pediatric Endocrinology & Metabolism. 9 (5): 501–9. doi:10.1515/JPEM.1996.9.5.501. PMID 8961125.
- ↑ Hogg-Kollars S; Al Dulaimi D; Tait K; Rostami K (2014). "Type 1 diabetes mellitus and gluten induced disorders". Gastroenterol Hepatol Bed Bench (Review). 7 (4): 189–97. PMC 4185872
 . PMID 25289132.
. PMID 25289132. - ↑ Feinman, RD; Pogozelski, WK; Astrup, A; Bernstein, RK; Fine, EJ; Westman, EC; Accurso, A; Frassetto, L; Gower, BA; McFarlane, SI; Nielsen, JV; Krarup, T; Saslow, L; Roth, KS; Vernon, MC; Volek, JS; Wilshire, GB; Dahlqvist, A; Sundberg, R; Childers, A; Morrison, K; Manninen, AH; Dashti, HM; Wood, RJ; Wortman, J; Worm, N (January 2015). "Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base.". Nutrition (Burbank, Los Angeles County, Calif.). 31 (1): 1–13. doi:10.1016/j.nut.2014.06.011. PMID 25287761.
- ↑ Ly, Trang T (2015). "Technology and type 1 diabetes: Closed-loop therapies". Current Pediatrics Reports. 3: 170–176. doi:10.1007/s40124-015-0083-y.
- ↑ "Stress". www.diabetes.org. American Diabetes Association. Retrieved 11 November 2014.
- ↑ Shrivastava, Saurabh (5 March 2013). "Role of self-care in management of diabetes mellitus". Journal of Diabetes & Metabolic Disorders. 12: 14. doi:10.1186/2251-6581-12-14.
- ↑ Wright JR (2002). "From ugly fish to conquer death: J J R Macleod's fish insulin research, 1922-24". Lancet. 359 (9313): 1238–42. doi:10.1016/S0140-6736(02)08222-3. PMID 11955558.
- ↑ American Diabetes Association (2015). "DKA (ketoacidosis) and ketones". American Diabetes Association.
- ↑ Tasker, Robert. C (2014). "Cerebral edema in children with diabetic ketoacidosis: vasogenic rather than cellular?". Pediatric Diabetes. 15: 261–270. doi:10.1111/pedi.12153.
- ↑ American Diabetes Association Clinical Guidelines, 2010.
- ↑ Blauw, H; Keith-Hynes, P; Koops, R; DeVries, JH (November 2016). "A Review of Safety and Design Requirements of the Artificial Pancreas.". Annals of biomedical engineering. 44 (11): 3158–3172. PMID 27352278.
- ↑ Jennifer L. Larsen. "Pancreas Transplantation: Indications and Consequences". Edrv.endojournals.org. Retrieved 29 November 2011.
- 1 2 3 Bruni, A; Gala-Lopez, B; Pepper, AR; Abualhassan, NS; Shapiro, AJ (2014). "Islet cell transplantation for the treatment of type 1 diabetes: recent advances and future challenges.". Diabetes, metabolic syndrome and obesity : targets and therapy. 7: 211–23. doi:10.2147/DMSO.S50789. PMID 25018643.
- ↑ Devaraj S, Glaser N, Griffen S, Wang-Polagruto J, Miguelino E, Jialal I (March 2006). "Increased monocytic activity and biomarkers of inflammation in patients with type 1 diabetes". Diabetes. 55 (3): 774–9. doi:10.2337/diabetes.55.03.06.db05-1417. PMID 16505242.
- ↑ Granberg V, Ejskjaer N, Peakman M, Sundkvist G (2005). "Autoantibodies to autonomic nerves associated with cardiac and peripheral autonomic neuropathy". Diabetes Care. 28 (8): 1959–64. doi:10.2337/diacare.28.8.1959. PMID 16043739.
- ↑ Huxley, Rachel R; Peters, Sanne A E; Mishra, Gita D; Woodward, Mark (February 2015). "Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis". The Lancet Diabetes & Endocrinology. 3: 198–206. doi:10.1016/S2213-8587(14)70248-7.
- ↑ Livingstone, SJ; Levin, D; Looker, HC; Lindsay, RS; Wild, SH; Joss, N; Leese, G; Leslie, P; McCrimmon, RJ; Metcalfe, W; McKnight, JA; Morris, AD; Pearson, DW; Petrie, JR; Philip, S; Sattar, NA; Traynor, JP; Colhoun, HM; Scottish Diabetes Research Network epidemiology, group; Scottish Renal, Registry (6 January 2015). "Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010.". JAMA. 313 (1): 37–44. doi:10.1001/jama.2014.16425. PMC 4426486
 . PMID 25562264.
. PMID 25562264. - ↑ Chen, Hsin-Chui; Su, Li-Ting; Linn, Shin-Zong; Sung, Fung-Chang; Ko, Ming-Chung; Li, Chung-Yi (January 2012). "Increased Risk of Urinary Tract Calculi Among Patients With Diabetes Mellitus–A Population-Based Cohort Study". Urology. 79 (1): 86–92. doi:10.1016/j.urology.2011.07.1431. Retrieved 28 November 2014.
- ↑ James, R; Hijaz, A (October 2014). "Lower urinary tract symptoms in women with diabetes mellitus: a current review.". Current Urology Reports. 15 (10): 440. doi:10.1007/s11934-014-0440-3. PMID 25118849.
- 1 2 3 McCoy, Krisha. "Sexual Issues and Type 1 Diabetes". everyday Health. Everyday Health Media, LLC. Retrieved 28 November 2014.
- 1 2 3 4 5 "Sexual Dysfunction in Women". Diabetes.co.uk. Diabetes Digital Media Ltd. Retrieved 28 November 2014.
- ↑ Goswami, Sumanta; Vishwanath, Manikanta; Gangadarappa, Suma; Razdan, Rema; Inamdar, Mohammed (Jul–Sep 2014). "Efficacy of ellagic acid and sildenafil in diabetes-induced sexual dysfunction". Pharmacognosy Magazine. 10 (39): 581. doi:10.4103/0973-1296.139790. Retrieved 30 November 2014.
- ↑ Escobar-Morreale, Héctor F.; Roldán, Belén; Barrio, Raquel; Alonso, Milagros; Sancho, José; de la Calle, Hermenegildo; GarcÍa-Robles, Rafael (November 2000). "High Prevalence of the Polycystic Ovary Syndrome and Hirsutism in Women with Type 1 Diabetes Mellitus". The Journal of Clinical Endocrinology & Metabolism. 85 (11): 4182–4187. doi:10.1210/jcem.85.11.6931.
- ↑ Codner, Ethel; Escobar-Morreale, Héctor F. (April 2007). "Hyperandrogenism and Polycystic Ovary Syndrome in Women with Type 1 Diabetes Mellitus". The Journal of Clinical Endocrinology & Metabolism. 92 (4): 1209–1216. doi:10.1210/jc.2006-2641.
- 1 2 Aanstoot HJ, Anderson BJ, Daneman D, Danne T, Donaghue K, Kaufman F, Réa RR, Uchigata Y (October 2007). "The global burden of youth diabetes: perspectives and potential". Pediatric diabetes. 8. Suppl 8 (s8): 1–44. doi:10.1111/j.1399-5448.2007.00326.x. PMID 17767619.
- ↑ Kasper, Dennis L; Braunwald, Eugene; Fauci, Anthony; et al. (2005). Harrison's Principles of Internal Medicine (16th ed.). New York: McGraw-Hill. ISBN 0-07-139140-1.
- ↑ Soltesz G, Patterson CC, Dahlquist G (October 2007). "Worldwide childhood type 1 diabetes incidence—what can we learn from epidemiology?". Pediatric diabetes. 8. Suppl 6 (s6): 6–14. doi:10.1111/j.1399-5448.2007.00280.x. PMID 17727380.
- 1 2 "Fast Facts" (PDF). American Diabetes Association.
- ↑ Bottazzo, GF; Florin-Christensen, A; Doniach, D (Nov 30, 1974). "Islet-cell antibodies in diabetes mellitus with autoimmune polyendocrine deficiencies.". Lancet. 2 (7892): 1279–83. doi:10.1016/s0140-6736(74)90140-8. PMID 4139522.
- ↑ Herold, KC; Vignali, DA; Cooke, A; Bluestone, JA (April 2013). "Type 1 diabetes: translating mechanistic observations into effective clinical outcomes.". Nature reviews. Immunology. 13 (4): 243–56. doi:10.1038/nri3422. PMID 23524461.
- ↑ Shaw, Jonathan (2012). "diabetes: the silent pandemic and its impact on Australia" (PDF). Retrieved October 19, 2016.
- ↑ Australian Institute of Health and Welfare (2015). "Incidence of type 1 diabetes in Australia 2000–2013". Retrieved October 19, 2016.
- ↑ Johnson, Linda (18 November 2008). "Study: Cost of diabetes $218B". USA Today. Associated Press.
- ↑ Diabetes Research and Wellness Foundation
- 1 2 Minami, K; Seino, S (18 March 2013). "Current status of regeneration of pancreatic β-cells.". Journal of diabetes investigation. 4 (2): 131–41. doi:10.1111/jdi.12062. PMID 24843642.
- ↑ Pagliuca, FW; Millman, JR; Gürtler, M; Segel, M; Van Dervort, A; Ryu, JH; Peterson, QP; Greiner, D; Melton, DA (9 October 2014). "Generation of functional human pancreatic β cells in vitro.". Cell. 159 (2): 428–39. doi:10.1016/j.cell.2014.09.040. PMID 25303535.
- ↑ Rezania, A; Bruin, JE; Arora, P; Rubin, A; Batushansky, I; Asadi, A; O'Dwyer, S; Quiskamp, N; Mojibian, M; Albrecht, T; Yang, YH; Johnson, JD; Kieffer, TJ (November 2014). "Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells.". Nature Biotechnology. 32 (11): 1121–33. doi:10.1038/nbt.3033. PMID 25211370.
- 1 2 3 Lernmark A, Larsson HE (Feb 2013). "Immune therapy in type 1 diabetes mellitus". Nat Rev Endocrinol. 9 (2): 92–103. doi:10.1038/nrendo.2012.237. PMID 23296174.
- 1 2 Antvorskov, Julie C.; Josefsen, Knud; Engkilde, Kåre; Funda, David P.; Buschard, Karsten (2014-01-01). "Dietary gluten and the development of type 1 diabetes". Diabetologia (Review). 57 (9): 1770–1780. doi:10.1007/s00125-014-3265-1. ISSN 0012-186X. PMC 4119241
 . PMID 24871322.
. PMID 24871322. - ↑ "Diabetes Mellitus (DM): Diabetes Mellitus and Disorders of Carbohydrate Metabolism: Merck Manual Professional". Merck.com. Retrieved 30 July 2010.
- ↑ Dorner M, Pinget M, Brogard JM (May 1977). "[Essential labile diabetes (author's transl)]". MMW Munch Med Wochenschr. 119 (19): 671–4. PMID 406527.
- ↑ Cartwright A, Wallymahmed M, Macfarlane IA, Wallymahmed A, Williams G, Gill GV (2011). "The outcome of brittle type 1 diabetes--a 20 year study". QJM. 104 (7): 575–9. doi:10.1093/qjmed/hcr010. PMID 21285231.
- ↑ Kent LA, Gill GV, Williams G (September 1994). "Mortality and outcome of patients with brittle diabetes and recurrent ketoacidosis". Lancet. 344 (8925): 778–81. doi:10.1016/S0140-6736(94)92340-X. PMID 7916072.
- 1 2 Davidson MB, Kumar D, Smith W (1991). "Successful treatment of unusual case of brittle diabetes with sulfated beef insulin". Diabetes Care. 14 (11): 1109–10. doi:10.2337/diacare.14.1.1109b. PMID 1797500.
- ↑ Fineberg SE, Kawabata TT, Finco-Kent D, Fountaine RJ, Finch GL, Krasner AS (2007). "Immunological Responses to Exogenous Insulin". Endocrine Reviews. 28 (6): 625–52. doi:10.1210/er.2007-0002. PMID 17785428.
External links
- Diabetes mellitus type 1 at DMOZ
- Kids and Teens: Type 1 Diabetes at DMOZ
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Diabetes in America Textbook (PDFs)
- IDF Diabetes Atlas
- International Diabetes Federation
- type 1 Diabetes at the American Diabetes Association
- National Diabetes Information Clearinghouse