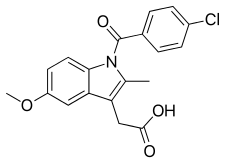
Indometacin
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ɪndoʊˈmɛtəsᵻn/ |
| Trade names | Indocid, Indocin |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category | |
| Routes of administration | Oral, rectal, IV, topical |
| ATC code | C01EB03 (WHO) M01AB01 (WHO), M02AA23 (WHO), S01BC01 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~100% (oral), 80–90% (rectal) |
| Protein binding | 99%[1] |
| Metabolism | Hepatic |
| Biological half-life | 2.6-11.2 hours (adults), 12-28 hours (infants)[1] |
| Excretion | Renal (60%), fecal (33%) |
| Identifiers | |
| |
| CAS Number |
53-86-1 |
| PubChem (CID) | 3715 |
| IUPHAR/BPS | 1909 |
| DrugBank |
DB00328 |
| ChemSpider |
3584 |
| UNII |
XXE1CET956 |
| KEGG |
D00141 |
| ChEBI |
CHEBI:49662 |
| ChEMBL |
CHEMBL6 |
| PDB ligand ID | IMN (PDBe, RCSB PDB) |
| ECHA InfoCard | 100.000.170 |
| Chemical and physical data | |
| Formula | C19H16ClNO4 |
| Molar mass | 357.787 g.mol−1 |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Indometacin (INN and BAN) or indomethacin (AAN, USAN and former BAN) is a nonsteroidal anti-inflammatory drug (NSAID) commonly used as a prescription medication to reduce fever, pain, stiffness, and swelling from inflammation. It works by inhibiting the production of prostaglandins, molecules known to cause these symptoms.[1][2]
It is marketed under more than twelve different trade names.[3] As of 2015 the cost for a typical month of medication in the United States is less than 25 USD.[4]
Medical uses
Clinical indications for indometacin include:
- ankylosing spondylitis
- arthritic gout
- Bartter syndrome
- bursitis
- cryoglobulinemia
- dysmenorrhea (menstrual cramps)
- fever and pain associated with malignant diseases (especially tumor fever associated with liver involvement, lymphogranulomatosis)
- headaches caused by the Valsalva maneuver
- hemicrania continua[5][6][7]
- hypnic headache[8]
- juvenile arthritis
- migraine[9]
- nephrogenic diabetes insipidus (prostaglandin inhibits vasopressin's action in the kidney)
- osteoarthritis
- Paget's disease of bone
- paroxysmal hemicrania[8]
- patent ductus arteriosus[10]
- pericarditis
- primary exertion headache
- primary stabbing headaches[8]
- pseudogout
- psoriatic arthritis
- reactive arthritis
- renal colic (pain due to kidney stones)
- retinopathy of prematurity
- rheumatoid arthritis
- tendinitis
- trigeminal autonomic cephalgias[8]
Indometacin has also been used clinically to delay premature labor, reduce amniotic fluid in polyhydramnios, and to close patent ductus arteriosus.
Indometacin is a potent drug with many serious side effects and should not be considered an analgesic for minor aches and pains or fever. The medication is better described as an anti-inflammatory, rather than an analgesic. Indometacin can also affect warfarin and subsequently raise INR.
Contraindications
- concurrent peptic ulcer, or history of ulcer disease
- allergy to indometacin, aspirin, or other NSAIDs
- patients with nasal polyps reacting with an angioedema to other NSAIDs
- children under 2 years of age (with the exception of neonates with patent ductus arteriosus)
- severe pre-existing renal and liver damage
- caution: pre-existing bone marrow damage (frequent blood cell counts are indicated)
- caution: bleeding tendencies of unknown origin (indometacin inhibits platelet aggregation)
- caution: Parkinson's disease, epilepsy, psychotic disorders (indometacin may worsen these conditions)[11]
- concurrent with potassium sparing diuretics
- patients who have a patent ductus arteriosus dependent heart defect (such as transposition of the great vessels)
- significant hypertension (high blood pressure)
- concomitant administration of lithium salts (such as lithium carbonate)
Adverse effects
Since indometacin inhibits both cyclooxygenase-1 and cyclooxygenase-2, it inhibits the production of prostaglandins in the stomach and intestines, which maintain the mucous lining of the gastrointestinal tract. Indometacin, therefore, like other non-selective COX inhibitors can cause peptic ulcers. These ulcers can result in serious bleeding and/or perforation requiring hospitalization of the patient.
To reduce the possibility of peptic ulcers, indometacin should be prescribed at the lowest dosage needed to achieve a therapeutic effect, usually between 50–200 mg/day. It should always be taken with food. Nearly all patients benefit from an ulcer protective drug (e.g. highly dosed antacids, ranitidine 150 mg at bedtime, or omeprazole 20 mg at bedtime). Other common gastrointestinal complaints, including dyspepsia, heartburn and mild diarrhea are less serious and rarely require discontinuation of indometacin.
Many NSAIDs, but particularly indometacin, cause lithium retention by reducing its excretion by the kidneys. Thus indometacin users have an elevated risk of lithium toxicity. For patients taking lithium (e.g. for treatment of depression or bipolar disorder), less toxic NSAIDs such as sulindac or aspirin are preferred.
Indometacin also increases plasma renin activity and aldosterone levels, and increases sodium and potassium retention. It also enhances the effects of vasopressin. Together these may lead to:
- edema (swelling due to fluid retention)
- hyperkalemia (high potassium levels)[12]
- hypernatremia (high sodium levels)
- hypertension
The drug may also cause elevations of serum creatinine and more serious renal damage such as acute renal failure, chronic nephritis and nephrotic syndrome. These conditions also often begin with edema and hyperkalemia.
Additionally, indometacin quite often causes headache (10 to 20%), sometimes with vertigo and dizziness, hearing loss, tinnitus, blurred vision (with or without retinal damage). There were reports of worsening Parkinson's disease, epilepsy, and psychiatric disorders but these are not substantiated. Cases of life-threatening shock (including angioedema, sweating, severe hypotension and tachycardia as well as acute bronchospasm), severe or lethal hepatitis and severe bone marrow damage have all been reported. Skin reactions and photosensitivity are also possible side effects.
Due to its strong antipyretic activity indometacin may obscure the clinical course of serious infections.
Psychosis has also been reported with prolonged use.
The frequency and severity of side effects and the availability of better tolerated alternatives make indometacin today a drug of second choice. Its use in acute gout attacks and in dysmenorrhea is well-established because in these indications the duration of treatment is limited to a few days only, therefore serious side effects are not likely to occur.
People should undergo regular physical examination to detect edema and signs of central nervous side effects. Blood pressure checks will reveal development of hypertension. Periodic serum electrolyte (sodium, potassium, chloride) measurements, complete blood cell counts and assessment of liver enzymes as well as of creatinine (renal function) should be performed. This is particularly important if Indometacin is given together with an ACE inhibitor or with potassium-sparing diuretics, because these combinations can lead to hyperkalemia and/or serious kidney failure. No examinations are necessary if only the topical preparations (spray or gel) are applied.
In women who are pregnant, it has been shown that use of this medication can have an effect of the fetal (Baby's) heart possibly resulting in fetal death.[13]
Toxicity
Indometacin has a high acute toxicity both for animals (in rats, 12 mg/kg) and for humans. Exact human data does not exist, but some fatal human cases, particularly in children and adolescents, have been seen.
Generally, overdose in humans causes drowsiness, dizziness, severe headache, mental confusion, paresthesia, numbness of limbs, nausea and vomiting. Severe gastrointestinal bleeding is also possible. Cerebral edema, and cardiac arrest with fatal outcome have been seen in children.
The treatment is symptomatic and largely the same as with diclofenac. However, the possibility of severe GI tract symptoms should be particularly noted.
The risk of overdose after exaggerated local treatment with gel or spray is very limited.
Mechanism of action
Indometacin is a nonselective inhibitor of cyclooxygenase (COX) 1 and 2, enzymes that participate in prostaglandin synthesis from arachidonic acid. Prostaglandins are hormone-like molecules normally found in the body, where they have a wide variety of effects, some of which lead to pain, fever, and inflammation.
Prostaglandins also cause uterine contractions in pregnant women. Indometacin is an effective tocolytic agent,[14] able to delay premature labor by reducing uterine contractions through inhibition of prostaglandin synthesis in the uterus and possibly through calcium channel blockade.
Indometacin has two additional modes of actions with clinical importance:
- it inhibits motility of polymorphonuclear leukocytes, similar to colchicine
- it uncouples oxidative phosphorylation in cartilaginous (and hepatic) mitochondria, like salicylates
These additional effects account as well for the analgesic and the anti-inflammatory properties.
Indometacin readily crosses the placenta and can reduce fetal urine production to treat polyhydramnios. It does so by reducing renal blood flow and increasing renal vascular resistance, possibly by enhancing the effects of vasopressin on the fetal kidneys.
History
Indometacin was discovered in 1963[15] and it was first approved for use in the U.S. by the Food and Drug Administration in 1965. Its mechanism of action, along with several other NSAIDs that inhibit COX, was described in 1971.[16]
See also
References
- 1 2 3 Brayfield, A, ed. (14 January 2014). "Indometacin". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. Retrieved 22 June 2014.
- ↑ "TGA Approved Terminology for Medicines, Section 1 – Chemical Substances" (PDF). Therapeutic Goods Administration, Department of Health and Ageing, Australian Government. July 1999: 70.
- ↑ Trade names are listed on DrugBank.ca entry DB00328
- ↑ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 8. ISBN 9781284057560.
- ↑ Sanders, Lisa (6 January 2012). "Think Like a Doctor: Ice Pick Pain Solved!". The New York Times.
- ↑ Garza, I & Schwedt, TJ. "Hemicrania continua." UpToDate. http://www.uptodate.com/contents/hemicrania-continua. Accessed 8/27/13.
- ↑ "Hemicrania Continua". www.migrainetrust.org. The Migraine Trust. Retrieved 11 June 2014.
- 1 2 3 4 Dodick, D.W. (8 February 2004). "Indomethacin-responsive headache syndromes". Current pain and headache reports. 8 (1): 19–26. doi:10.1007/s11916-004-0036-6. PMID 14731379.
- ↑ "Medication for Migraine". www.migrainetrust.org. The Migraine Trust. Retrieved 11 June 2014.
- ↑ Smyth JM, Collier PS, Darwish M, et al. (September 2004). "Intravenous indometacin in preterm infants with symptomatic patent ductus arteriosus. A population pharmacokinetic study". Br J Clin Pharmacol. 58 (3): 249–58. doi:10.1111/j.1365-2125.2004.02139.x. PMC 1884560
 . PMID 15327584.
. PMID 15327584. - ↑ "INDOMETHACIN". Hazardous Substances Data Bank (HSDB). National Library of Medicine's TOXNET. Retrieved April 4, 2013.
- ↑ Akbarpour F, Afrasiabi A, Vaziri N; Afrasiabi; Vaziri (1985). "Severe hyperkalemia caused by indomethacin and potassium supplementation". South Med J. 78 (6): 756–7. doi:10.1097/00007611-198506000-00039. PMID 4002013.
- ↑ Enzensberger, Christian; Wienhard, Julia; Weichert, Jan; Kawecki, Andreea; Degenhardt, Jan; Vogel, Melanie; Axt-Fliedner, Roland (2012-08-01). "Idiopathic Constriction of the Fetal Ductus Arteriosus Three Cases and Review of the Literature". Journal of Ultrasound in Medicine. 31 (8): 1285–1291. ISSN 0278-4297. PMID 22837295.
- ↑ Giles W, Bisits A; Bisits (October 2007). "Preterm labour. The present and future of tocolysis". Best Pract Res Clin Obstet Gynaecol. 21 (5): 857–68. doi:10.1016/j.bpobgyn.2007.03.011. PMID 17459777.
- ↑ Hart F, Boardman P; Boardman (October 1963). "Indomethacin: A New Non-steroid Anti-inflammatory Agent". Br Med J. 2 (5363): 965–70. doi:10.1136/bmj.2.5363.965. PMC 1873102
 . PMID 14056924.
. PMID 14056924. - ↑ Ferreira S, Moncada S, Vane J; Moncada; Vane (Jun 23, 1971). "Indomethacin and aspirin abolish prostaglandin release from the spleen". Nat New Biol. 231 (25): 237–9. doi:10.1038/newbio231237a0. PMID 5284362.
External links
- Effects of Perinatal Indomethacin Treatment on Preterm Infants, academic dissertation (PDF)
- Indomethacin, from MedicineNet
- Indomethacin, from Drugs.com
- Indocin: Description, chemistry, ingredients, from RxList.com