IUD with copper
| IUD with copper | |
|---|---|
|
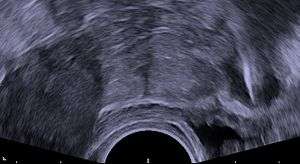
Photo of a common IUD (Paragard T 380A) | |
| Background | |
| Type | Intra-uterine |
| First use | 1909–1929 |
| Failure rates (first year) | |
| Perfect use | 0.6%[1] |
| Typical use | 0.8%[2] |
| Usage | |
| Duration effect | 5–12+ years |
| Reversibility | Immediate |
| User reminders | Check thread position after each period. Have removed shortly after menopause, if not before. |
| Clinic review | Annually |
| Advantages and disadvantages | |
| STD protection | No |
| Periods | May be heavier and more painful |
| Benefits |
Unnecessary to take any daily action. Emergency contraception if inserted within 5 days |
| Risks |
Small transient risk of PID in first 20 days following insertion. Rarely, uterine perforation. |
| IUD with copper | |
|---|---|
| Intervention | |
| ICD-9-CM | 69.7 |
A copper IUD (ATC G02BA (WHO)) (also intrauterine device, IUD, copper-T, or coil) is a type of intrauterine device. The copper IUD is a type of long-acting reversible contraception and is one of the most effective forms of birth control.[3]
It is on the World Health Organization's List of Essential Medicines, the most important medication needed in a basic health system.[4]
Medical uses
Copper IUDs are a form of long-acting reversible contraception and are one of the most effective forms of birth control available.[3] The type of frame and amount of copper can affect the effectiveness of different copper IUD models.[5] The failure rates for different models vary between 0.1 and 2.2% after 1 year of use. The T-shaped models with a surface area of 380 mm² of copper have the lowest failure rates. The TCu 380A (ParaGard) has a one-year failure rate of 0.8% and a cumulative 12-year failure rate of 2.2%.[5] Over 12 years of use, the models with less surface area of copper have higher failure rates. The TCu 220A has a 12-year failure rate of 5.8%, whereas the TCu 380A has a 12-year failure rate of 2.2%.[5] The frameless GyneFix also has a failure rate of less than 1% per year.[6] Worldwide, older IUD models with lower effectiveness rates are no longer produced.[7]
Unlike other forms of reversible contraception, the typical use failure rate and the perfect use failure rate for the copper IUDs are the same because the IUD does not depend on user action.[3] A 2008 review of the available T-shaped copper IUDs recommended that the TCu 380A and the TCu 280S be used as the first choice for copper IUDs because those two models have the lowest failure rates and the longest lifespans.[5] The effectiveness of the copper IUD is comparable to tubal sterilization, which has a first year failure rate of 0.5%.[8] However, the effects of the copper IUD are reversible, which can be viewed as either an advantage or a disadvantage, depending on a person's goals for contraception.
Emergency contraception
It was first discovered in 1976 that the copper IUD could be used as a form of emergency contraception (EC).[9] The copper IUD is the most effective form of emergency contraception. It is more effective than the hormonal EC pills currently available.[10] The pregnancy rate among those using the copper IUD for EC is 0.09%. It can be used for EC up to 5 days after the act of unprotected sex and does not decrease in effectiveness during the 5 days.[11] An additional advantage of using the copper IUD for emergency contraception is that it can be used as a form of birth control for 10–12 years after insertion.[11]
Removal and return to fertility
Removal of the copper IUD should also be performed by a qualified medical practitioner. Fertility has been shown to return to previous levels quickly after removal of the device.[12] One study found that the median amount of time from removal to planned pregnancy was three months for those women using the TCu 380Ag.[13]
Adverse effects
Expulsion: Sometimes the copper IUD can be spontaneously expelled from the uterus.[12] Expulsion rates can range from 2.2% to 11.4% of users from the first year to the 10th year. The TCu380A may have lower rates of expulsion than other models.[14] Unusual vaginal discharge, cramping or pain, spotting between periods, postcoital (after sex) spotting, dyspareunia, or the absence or lengthening of the strings can be signs of a possible expulsion.[12] If expulsion occurs, the woman is not protected against pregnancy. If an IUD with copper is inserted after an expulsion has occurred, the risk of re-expulsion has been estimated in one study to be approximately one third of cases after one year.[15]
Perforation: Very rarely, the IUD can move through the wall of the uterus.[12] Risk of perforation is mostly determined by the skill of the practitioner performing the insertion. For experienced medical practitioners, the risk of perforation is 1 per 1,000 insertions or less.[16] If perforation does occur it can damage the internal organs, and in some cases surgery is needed to remove the IUD.
Infection: The insertion of a copper IUD poses a transient risk of pelvic inflammatory disease (PID) in the first 21 days after insertion. However, it is a small risk and is attributable to preexisting gonorrhea or chlamydia infection at the time of insertion, and not to the IUD itself.[17][18] Proper infection prevention procedures have little or no effect on the course of gonorrhea or chlamydia infections, but is important in helping protect both clients and providers from infection in general.[18] Such infection prevention practices include washing hands and then putting on gloves, cleaning the cervix and vagina, making minimal contact with non-sterile surfaces (using a "no touch insertion technique") and, after the procedure, washing hands again and then processing instruments.[7] The device itself carries no increased risk of PID beyond the time of insertion.[12]
Cramping: Many women feel cramping or pain during the IUD insertion process and immediately after as a result of cervix dilation during insertion.[7] Taking NSAIDS before the procedure can reduce discomfort,[19] as can the use of a local anaesthetic. Misoprostol 6 to 12 hrs before insertion can help with cervical dilation.[19] Some women may have cramps for 1 to 2 weeks following insertion. The copper IUD can also increase cramps during a woman’s period. This symptom will clear up for some women in 3 to 6 months, but may not for others.[12]
Heavier periods: The copper IUD increases the amount of blood flow during a woman’s menstrual periods.[7] On average, menstrual blood loss increases by 20–50% after insertion of a copper-T IUD; increased menstrual discomfort is the most common medical reason for IUD removal. This symptom may clear up for some women after 3 to 6 months, but may not for others.[20]
Irregular bleeding and spotting: For the first 3 to 6 months after insertion, the copper IUD can cause irregular periods and spotting between periods.[12]

String problems: A small portion of men report that they can feel the strings during intercourse. In this case, strings can be trimmed. However, very short strings can prevent the woman from checking the strings for expulsion.[12] Medical ultrasonography may be required in such cases to check the location of the IUD.
Pregnancy: Although rare, if pregnancy does occur with the copper IUD in place there can be serious side effects. The risk of ectopic pregnancy to a woman using an IUD is lower than the risk of ectopic pregnancy to a woman using no form of birth control. However, of pregnancies that do occur during IUD use, a higher than expected percentage (3–4%) are ectopic.[7] If a pregnancy occurs with the IUD in place there is a higher risk of miscarriage or early delivery. If this occurs and the IUD strings are visible, the IUD should be removed immediately by a clinician.[12] Although the Dalkon Shield IUD was associated with septic abortions (infections associated with miscarriage), other brands of IUD are not. IUDs are also not associated with birth defects.[7]
Some barrier contraceptives protect against STIs. Hormonal contraceptives reduce the risk of developing pelvic inflammatory disease (PID), a serious complication of certain STIs. IUDs, by contrast, do not protect against STIs or PID.[21][12]
Contraindications
A category 3 condition indicates conditions where the theoretical or proven risks usually outweigh the advantages of inserting a copper IUD. A category 4 condition indicates conditions that represent an unacceptable health risk if a copper IUD is inserted.
Women should not use a copper IUD if they:
(Category 4)
- Are pregnant or think they may be pregnant
- Septic pregnancy or abortion
- Have unexplained abnormal vaginal bleeding
- Have untreated cervical cancer
- Have malignant gestational trophoblastic disease
- Have uterine cancer
- Have certain uterine abnormalities
- Have or may have had a pelvic infection within the past three months
- Have or may have an STI
- Have pelvic tuberculosis
(Category 3)
- Are postpartum between 48 hours and 4 weeks (increased IUD expulsion rate with delayed postpartum insertion). The CDC and WHO criteria differ in their recommendation for women postpartum between 48 hours and 4 weeks. The CDC does not list this as a contraindication.
- Have benign gestational trophoblastic disease
- Have ovarian cancer
- Have AIDS (unless clinically well on anti-retroviral therapy)
- Have very high individual likelihood of exposure to gonorrhea or chlamydial STIs
A full list of contraindications can be found in the WHO Medical Eligibility Criteria for Contraceptive Use[20] and the CDC United States Medical Eligibility Criteria for Contraceptive Use.[22]
While nulliparous women (women who have never given birth) are somewhat more likely to have side effects, this is not a contraindication for IUD use. Overall, IUDs are safe and acceptable also in young nulliparous women.[23] The same is likely the case for virgin women, unless there is a microperforate hymen that obstructs any insertion of the IUD.
Device description
There are a number of models of the copper IUD available around the world. Most copper devices consist of a plastic core that is wrapped in a copper wire.[5] Many of the devices have a T-shape similar to the hormonal IUD. However, there are "frameless" copper IUDs available around the world as well. ParaGard is the only model currently available in the United States. At least three copper IUD models are available in Canada, two of which are a slimmer T-shape version used for women who have not had children. Early copper IUDs had copper around only the vertical stem, but more recent models have copper sleeves wrapped around the horizontal arms as well, increasing effectiveness.[24] Some newer models also contain a silver core instead of a plastic core to delay copper fragmentation as well as increase the lifespan of the device. The lifespan of the devices range from 3 years to 10 years; however, some studies have demonstrated that the TCu 380A may be effective through 12 years.[16]
Insertion
The copper IUD must be inserted by a qualified medical practitioner. A copper IUD can be inserted at any phase of the menstrual cycle, but the optimal time is right after the menstrual period, when the cervix is softest and the woman is least likely to be pregnant.[25] The insertion process generally takes five minutes or less. The procedure can cause cramping or be painful for some women. Before placement of an IUD, a medical history and physical examination by a medical professional is useful to check for any contraindications or concerns.[25] It is also recommended by some clinicians that patients be tested for gonorrhea and chlamydia, as these two infections increase the risk of contracting pelvic inflammatory disease shortly after insertion.[17] Immediately prior to insertion, the clinician will perform a pelvic exam to determine the position of the uterus.[12] After the pelvic exam, the vagina is held open with a speculum.[25] A tenaculum is used to steady the cervix and uterus.[25] Uterine sounding may be used to measure the length and direction of the cervical canal and uterus in order to decrease the risk of uterine perforation.[26] The IUD is placed using a narrow tube, which is inserted through the cervix into the uterus. Short monofilament plastic/nylon strings hang down from the uterus into the vagina. The clinician will trim the threads so that they only protrude 3 to 4 cm out of the cervix and remain in the upper vagina. The strings allow the patient or clinician to periodically check to ensure the IUD is still in place and to enable easy removal of the device.[12]
The copper IUD can be inserted at any time in a woman's menstrual cycle as long as the woman is not pregnant.[16] An IUD can also be inserted immediately postpartum and post-abortion as long as no infection has occurred.[22] Breastfeeding is not a contraindication for the use of the copper IUD. The IUD can be inserted in women with HIV or AIDS as it does not increase the risk of transmission.[20] Although previously not recommended for nulliparous women (women who have not had children), the IUD is now recommended for most women who are past menarche (their first period), including adolescents.[27]
After the insertion is finished, normal activities such as sex, exercise, and swimming can be performed as soon as it feels comfortable.[25] Strenuous physical activity does not affect the position of the IUD.[25]
Types
Many different types of copper IUDs are currently manufactured worldwide, but availability varies by country. In the United States, only one type of copper IUD is approved for use, while in the United Kingdom, over ten varieties are available.[28] One company, Mona Lisa N.V. offers generic versions of many existing IUDs.[29]
| IUD | Type | Copper (mm2) | Life (years) | Manufacturer | Distinguishing characteristics |
|---|---|---|---|---|---|
| Gyneplus Cu 380 | T-shaped | 380 | 5 | Dispo.Cont. | |
| Multiload Cu375 | U-shaped | 375 | 5 | Multilan | |
| Multiload Cu250 | U-shaped | 250 | 3 | Multilan | |
| Multi-Safe 375 | U-shaped | 375 | 5 | Williams Medical Supplies | |
| Multi-Safe 375 Short Loop | U-shaped | 375 | 5 | Williams Medical Supplies | |
| Load 375 | U-shaped | 375 | 5 | 7-MED Industrie | |
| Nova-T 380 | T-shaped (plain) | 380 | 5 | Bayer | |
| Neo-Safe T 380 | T-shaped (plain) | 380 | 5 | Durbin | |
| UT 380 | T-shaped (plain) | 380 | 5 | 7-MED Industrie | |
| UT 380 Short | T-shaped (plain) | 380 | 5 | 7-MED Industrie | |
| Flexi-T 300 | T-shaped (plain) | 300 | 5 | Prosan | |
| Flexi-T + 300 | T-shaped (plain) | 300 | 5 | Prosan | Wider arms than Flexi-T 300 |
| T-safe CU 380A | T-shaped (banded) | 380 | 8 | Durbin | |
| Flexi-T + 380 | T-shaped (banded) | 380 | 5 | Prosan | |
| TT 380 Slimline | T-shaped (banded) | 380 | 10 | 7-MED Industrie | |
| TT 380 Mini | T-shaped (banded) | 380 | 5 | 7-MED Industrie | |
| Paragard | T-shaped (banded) | 380 | 10 | Duramed | Only copper IUD currently approved by the U.S. FDA |
| Gynefix 330 (standard) | Frameless | 330 | 5 | Contrel | Only frameless IUD brand available |
| Gynefix 200 (mini) | Frameless | 200 | 3 | Contrel | Only frameless IUD brand available |
| IUB SCu300A/B | Spherical (3D) | 300 | 5 | OCON | Nitinol alloy cored frame |
Frameless IUDs
The frameless IUD eliminates the use of the frame that gives conventional IUDs their signature T-shape. This change in design was made to reduce discomfort and expulsion associated with prior IUDs; without a solid frame, the frameless IUD should mold to the shape of the uterus. It may reduce expulsion and discontinuation rates compared to framed copper IUDs.[30]
Gynefix is the only frameless IUD brand currently available. It consists of hollow copper tubes on a polypropylene thread. It is inserted through the cervix with a special applicator that sutures the thread to the fundus (top) of the uterus; the thread is then cut with a tail hanging outside of the cervix, similar to frame IUDs. When this tail is pulled, the suture comes undone and the device can be removed. This requires more force than removing a T-shaped IUD, but results in comparable discomfort during removal.[31] Gynefix is not approved for use in the United States.
Mechanism of action

The copper IUD's primary mechanism of action is to prevent fertilization.[12][32][33][34] Copper acts as a spermicide within the uterus. The presence of copper increases the levels of copper ions, prostaglandins, and white blood cells within the uterine and tubal fluids.[12][32]
Although not a primary mechanism of action, some experts in human reproduction believe there is sufficient evidence to suggest that IUDs with copper can disrupt implantation,[35] especially when used for emergency contraception.[36][2] Despite this, there has been no definitive evidence that IUD users have higher rates of embryonic loss than women not using contraception.[32] Therefore, the copper IUD is considered to be a true contraceptive and not an abortifacient.[12]
Usage
Globally, the IUD is the most widely used method of reversible birth control.[37] The most recent data indicates that there are 169 million IUD users around the world. This includes both the nonhormonal and hormonal IUDs. IUDs are most popular in Asia, where the prevalence is almost 30%. In Africa and Europe the prevalence is around 20%.[37] As of 2009, levels of IUD use in the United States are estimated to be 5.5%.[8] Data in the United States does not distinguish between hormonal and nonhormonal IUDs. In Europe, copper IUD prevalence ranges from under 5% in the United Kingdom to over 10% in Denmark in 2006.[38]
History
According to popular legend, Arab traders inserted small stones into the uteruses of their camels to prevent pregnancy during long desert treks. The story was originally a tall tale to entertain delegates at a scientific conference on family planning; although it was later repeated as truth, it has no known historical basis.[39]
Precursors to IUDs were first marketed in 1902. Developed from stem pessaries (where the stem held the pessary in place over the cervix), the 'stem' on these devices actually extended into the uterus itself. Because they occupied both the vagina and the uterus, this type of stem pessary was also known as an interuterine device. Use of interuterine devices was associated with high rates of infection; for this reason, they were condemned by the medical community.[40]
The first intrauterine device (contained entirely in the uterus) was described in a German publication in 1909, although the author appears to have never marketed his product.[41]
In 1929, Ernst Gräfenberg of Germany published a report on an IUD made of silk suture. He had found a 3% pregnancy rate among 1,100 women using his ring. In 1930, Gräfenberg reported a lower pregnancy rate of 1.6% among 600 women using an improved ring wrapped in silver wire. Unbeknownst to Gräfenberg, the silver wire was contaminated with 26% copper. Copper's role in increasing IUD efficacy would not be recognized until nearly 40 years later.
In 1934, Japanese physician Tenrei Ota developed a variation of the Gräfenberg ring that contained a supportive structure in the center. The addition of this central disc lowered the IUD's expulsion rate. These devices still had high rates of infection, and their use and development was further stifled by World War II politics: contraception was forbidden in both Nazi Germany and Axis-allied Japan. The Allies did not learn of the work by Gräfenberg and Ota until well after the war ended.[41]
The first plastic IUD, the Margulies Coil or Margulies Spiral, was introduced in 1958. This device was somewhat large, causing discomfort to a large proportion of women users, and had a hard plastic tail, causing discomfort to their male partners. The modern colloquialism "coil" is based on the coil-shaped design of early IUDs.
The Lippes Loop, a slightly smaller device with a monofilament tail, was introduced in 1962 and gained in popularity over the Margulies device.[40]
The stainless steel single-ring IUD was developed in the 1970s[42] and widely used in China because of low manufacturing costs. The Chinese government banned production of steel IUDs in 1993 due to high failure rates (up to 10% per year).[7][43]
Howard Tatum, in the USA, conceived the plastic T-shaped IUD in 1968. Shortly thereafter Jaime Zipper, in Chile, introduced the idea of adding copper to the devices to improve their contraceptive effectiveness.[40][44] It was found that copper-containing devices could be made in smaller sizes without compromising effectiveness, resulting in fewer side effects such as pain and bleeding.[7] T-shaped devices had lower rates of expulsion due to their greater similarity to the shape of the uterus.[41]
The poorly designed Dalkon Shield plastic IUD (which had a multifilament tail) was manufactured by the A. H. Robins Company and sold by Robins in the United States for three and a half years from January 1971 through June 1974, before sales were suspended by Robins on June 28, 1974 at the request of the FDA because of safety concerns following reports of 110 septic spontaneous abortions in women with the Dalkon Shield in place, seven of whom had died.[45][46] Robins stopped international sales of the Dalkon Shield in April 1975.[47]
Tatum developed many different models of the copper IUD. He created the TCu220 C, which had copper collars as opposed to copper filament, which prevented metal loss and increased the lifespan of the device. Second-generation copper-T IUDs were also introduced in the 1970s. These devices had higher surface areas of copper, and for the first time consistently achieved effectiveness rates of greater than 99%.[7] The last model Tatum developed was the TCu380A, the model that is most recommended today.[5] In addition to T-shaped IUDs, there are also U-shaped IUDs (such as the Multiload) and 7-shaped Gravigard Copper 7 (with a mini version for nulliparous women introduced in the 1980s). More recently, a frameless IUD called Gynefix was introduced.
Brands
The ParaGard T-380A is an IUD with copper, manufactured and marketed in the United States by Duramed Pharmaceuticals. It is the only copper-containing intrauterine device approved for use in the U.S. (three hormonal uterine devices, Mirena, Skyla and Liletta are also approved). The ParaGard consists of a T-shaped polyethylene frame wound with copper wire, along with two monofilament threads to aid in removal of the IUD.
The ParaGard T 380A was developed in the 1970s by the Population Council and Finishing Enterprises Inc. (FEI). The Population Council's ParaGard new drug application (NDA) was approved by the U.S. Food and Drug Administration (FDA) and FEI began manufacturing it for distribution outside the United States in 1984. GynoPharma (originally GynoMed) began marketing it in the U.S. in May 1988. On August 2, 1995, Ortho-McNeil acquired GynoPharma and began marketing ParaGard in the U.S. On January 1, 2004, FEI Women's Health acquired the patent from the Population Council and U.S. marketing rights from Ortho-McNeil. On November 10, 2005, Duramed Pharmaceuticals, a subsidiary of Barr Pharmaceuticals, acquired FEI Women's Health and ParaGard. On July 18, 2008, it was announced that Teva Pharmaceutical Industries Ltd. would acquire Barr Pharmaceuticals.
The original FDA approval of ParaGard in 1984 was for 4 years continuous use, this was later extended to 6 years in 1989, then 8 years in 1991, then 10 years in 1994. (ATC code G02BA02 (WHO))
See also
References
- ↑ Trussell, James (2011). "Contraceptive efficacy". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States.
- 1 2 Trussell, James; Schwarz, Eleanor Bimla (2011). "Emergency contraception". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 113–145. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. p. 121:
Mechanism of action
Copper-releasing IUCs
When used as a regular or emergency method of contraception, copper-releasing IUCs act primarily to prevent fertilization. Emergency insertion of a copper IUC is significantly more effective than the use of ECPs, reducing the risk of pregnancy following unprotected intercourse by more than 99%.2,3 This very high level of effectiveness implies that emergency insertion of a copper IUC must prevent some pregnancies after fertilization.
Pregnancy begins with implantation according to medical authorities such as the US FDA, the National Institutes of Health79 and the American College of Obstetricians and Gynecologists (ACOG).80 - 1 2 3 Winner, B; Peipert, JF; Zhao, Q; Buckel, C; Madden, T; Allsworth, JE; Secura, GM. (2012), "Effectiveness of Long-Acting Reversible Contraception", New England Journal of Medicine, 366 (21): 1998–2007, doi:10.1056/NEJMoa1110855, PMID 22621627
- ↑ "19th WHO Model List of Essential Medicines (April 2015)" (PDF). WHO. April 2015. Retrieved May 10, 2015.
- 1 2 3 4 5 6 Kulier R, O'Brien P, Helmerhorst FM, Usher-Patel M, d'Arcangues C (2008), "Copper containing, framed intra-uterine devices for contraception (Review)", Cochrane Database of Systematic Reviews (4), doi:10.1002/14651858.CD005347.PUB3, PMID 17943851
- ↑ O'Brien, PA; Marfleet C (January 25, 2005). "Frameless versus classical intrauterine device for contraception". Cochrane Database of Systematic Reviews (1): CD003282. doi:10.1002/14651858.CD003282. PMID 11687184.
- 1 2 3 4 5 6 7 8 9 Treiman, Katherine; Liskin, Laurie; Kols, Adrienne; Rinehart, Ward (December 1995). "IUDs—an update" (PDF). Population Reports. Series B, Intrauterine Devices. Baltimore: Johns Hopkins School of Public Health, Population Information Program (6): 1–35. PMID 8724322. Retrieved July 9, 2006.
- 1 2 The Guttmacher Institute (2012). "Contraceptive Use in the United States". Retrieved 2013-10-04.
- ↑ Lippes, J; Malik, T; Tatum, HJ (1976). "The postcoital copper-T". Adv Plan Parent. 11: 24–9.
- ↑ Cheng, L; Gulmezoglu, AM; Piaggio, G; Ezcurra, E; Van Look, PF (2008). "Interventions for emergency contraception". Cochrane Database of Systematic Reviews: CD001324. doi:10.1002/14651858.cd001324.pub3.
- 1 2 Cleland K, Zhu H, Goldstruck N, Cheng L, Trussel T (2012). "The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience". Human Reproduction. 27 (7): 1994–2000. doi:10.1093/humanrep/des140.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Dean, Gillian; Schwarz, Eleanor Bimla (2011). "Intrauterine contraceptives (IUCs)". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 147–191. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. p.150:
Mechanism of action
Although the precise mechanism of action is not known, currently available IUCs work primarily by preventing sperm from fertilizing ova.26 IUCs are not abortifacients: they do not interrupt an implanted pregnancy.27 Pregnancy is prevented by a combination of the "foreign body effect" of the plastic or metal frame and the specific action of the medication (copper or levonorgestrel) that is released. Exposure to a foreign body causes a sterile inflammatory reaction in the intrauterine environment that is toxic to sperm and ova and impairs implantation.28,29 The production of cytotoxic peptides and activation of enzymes lead to inhibition of sperm motility, reduced sperm capacitation and survival, and increased phagocytosis of sperm.30,31 The TCu380A causes an increase in copper ions, enzymes, prostaglandins, and white blood cells (macrophages) in uterine and tubal fluids; these impair sperm function and prevent fertilization.
p. 162:
Table 7-1. Myths and misconceptions about IUCs
Myth: IUCs are abortifacients. Fact: IUCs prevent fertilization and are true contraceptives. - ↑ Belhadj, H; et al. (1986), "Recovery of fertility after use of the Levonorgestrel 20 mcg/d or copper T 380 Ag intrauterine device", Contraception, 34 (3): 261–267, doi:10.1016/0010-7824(86)90007-7, PMID 3098498
- ↑ Kaneshiro B, Aeby T (2010). "Long-term safety, efficacy, and patient acceptability of the intrauterine Copper T-380A contraceptive device". International Journal of Women's Health. 2: 211–220. doi:10.2147/ijwh.s6914. PMC 2971735
 . PMID 21072313.
. PMID 21072313. - ↑ Bahamondes L, Díaz J, Marchi NM, Petta CA, Cristofoletti ML, Gomez G (November 1995). "Performance of copper intrauterine devices when inserted after an expulsion". Hum. Reprod. 10 (11): 2917–8. PMID 8747044.
- 1 2 3 World Health Organization (1987), Mechanism of action, safety, and efficacy of intrauterine deices: technical report series 753, Geneva: World Health Organization
- 1 2 Mohllajee, AP; Curtis, KM; Peterson, HB (2006), "Does insertion of an intrauterine device increase the risk of pelvic inflammatory disease among women with sexually transmitted infection? A systematic review", Contraception, 73: 143–153, doi:10.1016/j.contraception.2005.08.007
- 1 2 maqweb.org > Infection Prevention Practices for IUD Insertion and Removal By the United States Agency for International Development (USAID). Retrieved on Feb 14, 2010
- 1 2 Hutten-Czapski P, Goertzen J (2008). "The occasional intrauterine contraceptive device insertion" (PDF). Can J Rural Med. 13 (1): 31–5. PMID 18208650.
- 1 2 3 WHO (2010). "Intrauterine devices (IUDs)". Medical Eligibility Criteria for Contraceptive Use (4th ed.). Geneva: Reproductive Health and Research, WHO. ISBN 978 92 4 1563888.
- ↑ Farley TM, Rosenberg MJ, Rowe PJ, Chen JH, Meirik O (1992). "Intrauterine devices and pelvic inflammatory disease: an international perspective". Lancet. 339 (8796): 785–8. doi:10.1016/0140-6736(92)91904-M. PMID 1347812.
Grimes DA (2000). "Intrauterine device and upper-genital-tract infection". Lancet. 356 (9234): 1013–9. doi:10.1016/S0140-6736(00)02699-4. PMID 11041414. - 1 2 Centers for Disease Control and Prevention (2010), United States Medical Eligibility Criteria for Contraceptive Use., retrieved 2013-10-04
- ↑ Forthofer KV (2009). "A clinical review of the intrauterine device as an effective method of contraception". J Obstet Gynecol Neonatal Nurs. 38 (6): 693–8. doi:10.1111/j.1552-6909.2009.01067.x. PMID 19930283.
- ↑ Sivin I, Stern J (1979), "Long-acting, more effective Copper T IUDs: a summary of U.S. experience, 1970-1975", Studies in Family Planning, 10: 263–281, doi:10.2307/1965507, JSTOR 1965507
- 1 2 3 4 5 6 Birth Control Intrauterine Devices (IUDs) Author: Omnia M Samra. Last Editorial Review: 5/18/2006
- ↑ about.com > What To Expect During an IUD Insertion By Dawn Stacey M.Ed. Updated April 30, 2010
- ↑ ACOG Committee Opinion 450 (December 2009). "Increasing the Use of Contraceptive Implants and Intrauterine Devices To Reduce Unintended Pregnancy". American Congress of Obstetricians and Gynecologists. Retrieved 2012-06-28.
- ↑ "Contraceptive coils (IUDs)". NetDoctor.co.uk. 2006. Retrieved 2006-07-05.
- ↑ Mona Lisa N.V., a manufacturer of generic IUDs
- ↑ Wu S, Hu J, Wildemeersch D (February 2000). "Performance of the frameless GyneFix and the TCu380A IUDs in a 3-year multicenter, randomized, comparative trial in parous women". Contraception. 61 (2): 91–8. doi:10.1016/s0010-7824(00)00087-1. PMID 10802273.
- ↑ D'Souza RE, Bounds W, Guillebaud J (April 2003). "Comparative trial of the force required for, and pain of, removing GyneFix versus Gyne-T380S following randomised insertion". J Fam Plann Reprod Health Care. 29 (2): 29–31. doi:10.1783/147118903101197494. PMID 12681034.
- 1 2 3 Ortiz, María Elena; Croxatto, Horacio B. (June 2007). "Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action". Contraception. 75 (6 Suppl): S16‒S30. doi:10.1016/j.contraception.2007.01.020. PMID 17531610. p. S28:
Conclusions
Active substances released from the IUD or IUS, together with products derived from the inflammatory reaction present in the luminal fluids of the genital tract, are toxic for spermatozoa and oocytes, preventing the encounter of healthy gametes and the formation of viable embryos. The current data do not indicate that embryos are formed in IUD users at a rate comparable to that of nonusers. The common belief that the usual mechanism of action of IUDs in women is destruction of embryos in the uterus is not supported by empirical evidence. The bulk of the data indicate that interference with the reproductive process after fertilization has taken place is exceptional in the presence of a T-Cu or LNG-IUD and that the usual mechanism by which they prevent pregnancy in women is by preventing fertilization. - ↑ Speroff, Leon; Darney, Philip D. (2011). "Intrauterine contraception". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 239–280. ISBN 978-1-60831-610-6. p. 246:
Mechanism of action
The contraceptive action of all IUDs is mainly in the intrauterine cavity. Ovulation is not affected, and the IUD is not an abortifacient.58–60 It is currently believed that the mechanism of action for IUDs is the production of an intrauterine environment that is spermicidal.
Nonmedicated IUDs depend for contraception on the general reaction of the uterus to a foreign body. It is believed that this reaction, a sterile inflammatory response, produces tissue injury of a minor degree but sufficient enough to be spermicidal. Very few, if any, sperm reach the ovum in the fallopian tube… In women using copper IUDs, sensitive assays for human chorionic gonadotropin do not find evidence of fertilization.62,63 This is consistent with the fact that the copper IUD protects against both intrauterine and ectopic pregnancies.
The copper IUD releases free copper and copper salts that have both a biochemical and morphological impact on the endometrium and also produce alterations in cervical mucus and endometrial secretions... An additional spermicidal effect probably takes place in the cervical mucus. - ↑ Jensen, Jeffrey T.; Mishell, Daniel R. Jr. (2012). "Family planning: contraception, sterilization, and pregnancy termination". In Lentz, Gretchen M.; Lobo, Rogerio A.; Gershenson, David M.; Katz, Vern L. Comprehensive gynecology. Philadelphia: Mosby Elsevier. pp. 215–272. ISBN 978-0-323-06986-1. p. 259:
Intrauterine devices
Mechanisms of action
The common belief that the usual mechanism of action of IUDs in women is destruction of embryos in the uterus is not supported by empirical evidence... Because concern over mechanism of action represents a barrier to acceptance of this important and highly effective method for some women and some clinicians, it is important to point out that there is no evidence to suggest that the mechanism of action of IUDs is abortifacient... the principal mechanism of action of the copper T 380A IUD is to interfere with sperm action, preventing fertilization of the ovum. - ↑ ESHRE Capri Workshop Group (May–June 2008). "Intrauterine devices and intrauterine systems". Human Reproduction Update. 14 (3): 197‒208. doi:10.1093/humupd/dmn003. PMID 18400840. p. 199:
Mechanisms of action
Thus, both clinical and experimental evidence suggests that IUDs can prevent and disrupt implantation. It is unlikely, however, that this is the main IUD mode of action, … The best evidence indicates that in IUD users it is unusual for embryos to reach the uterus.
In conclusion, IUDs may exert their contraceptive action at different levels. Potentially, they interfere with sperm function and transport within the uterus and tubes. It is difficult to determine whether fertilization of the oocyte is impaired by these compromised sperm. There is sufficient evidence to suggest that IUDs can prevent and disrupt implantation. The extent to which this interference contributes to its contraceptive action is unknown. The data are scanty and the political consequences of resolving this issue interfere with comprehensive research.
p. 205:
Summary
IUDs that release copper or levonorgestrel are extremely effective contraceptives... Both copper IUDs and levonorgestrel releasing IUSs may interfere with implantation, although this may not be the primary mechanism of action. The devices also create barriers to sperm transport and fertilization, and sensitive assays detect hCG in less than 1% of cycles, indicating that significant prevention must occur before the stage of implantation. - ↑ Speroff, Leon; Darney, Philip D. (2011). "Special uses of oral contraception: emergency contraception, the progestin-only minipill". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 153–166. ISBN 978-1-60831-610-6. p. 157:
Emergency postcoital contraception
Other methods
Another method of emergency contraception is the insertion of a copper IUD, anytime during the preovulatory phase of the menstrual cycle and up to 5 days after ovulation. The failure rate (in a small number of studies) is very low, 0.1%.34,35 This method definitely prevents implantation, but it is not suitable for women who are not candidates for intrauterine contraception, e.g., multiple sexual partners or a rape victim. The use of a copper IUD for emergency contraception is expensive, but not if it is retained as an ongoing method of contraception. - 1 2 Brigid Fitzgerald Reading. "Growth in World Contraceptive Use Stalling; 215 Million Women's Needs Still Unmet". Earth Policy Institute. Retrieved 2013-10-04.
- ↑ Sonfield, Adam (2012). "Popularity Disparity: Attitudes About the IUD in Europe and the United States". The Guttmacher Institute.
- ↑ "A History of Birth Control Methods". Planned Parenthood. June 2002. Archived from the original on 2008-05-17. Retrieved 2007-10-14., which cites:
- Thomas, Patricia (1988-03-14). "Contraceptives". Medical World News. 29 (5): 48.
- Bullough, Vern L.; Bullough, Bonnie (1990). Contraception: A Guide to Birth Control Methods. Buffalo, NY: Prometheus Books.
- 1 2 3 Lynch, Catherine M. "History of the IUD". Contraception Online. Baylor College of Medicine. Archived from the original on 2006-01-27. Retrieved 2006-07-09.
- 1 2 3 "Evolution and Revolution: The Past, Present, and Future of Contraception". Contraception Online (Baylor College of Medicine). 10 (6). February 2000. Archived from the original on September 26, 2006.
- ↑ Bradley, Jeff (August 1998). "Ultrasound Interactive Case Study: Ring IUD". OBGYN.net. Retrieved 2006-07-09. (Has pictures of various IUD designs.)
- ↑ Kaufman, J. (May–Jun 1993). "The cost of IUD failure in China". Studies in Family Planning. 24 (3): 194–6. doi:10.2307/2939234. JSTOR 2939234. PMID 8351700.
- ↑ Van Kets, H.E. (1997). C. Coll Capdevila; L. Iglesias Cortit; G. Creatsas, eds. "Importance of intrauterine contraception". Contraception Today, Proceedings of the 4th Congress of the European Society of Contraception. The Parthenon Publishing Group. pp. 112–116. Retrieved 2006-07-09. (Has pictures of many IUD designs, both historic and modern.)
- ↑ Sivin I (1993). "Another look at the Dalkon Shield: meta-analysis underscores its problems". Contraception. 48 (1): 1–12. doi:10.1016/0010-7824(93)90060-K. PMID 8403900.
- ↑ Mintz, Morton (January 15, 1986). "A Crime Against Women. A. H. Robins and the Dalkon Shield". Multinational Monitor. 7 (1).
- ↑ Salem R (February 2006). "New Attention to the IUD: Expanding Women's Contraceptive Options To Meet Their Needs". Popul Rep B (7).
