Hypoplastic left heart syndrome
| Hypoplastic left heart syndrome | |
|---|---|
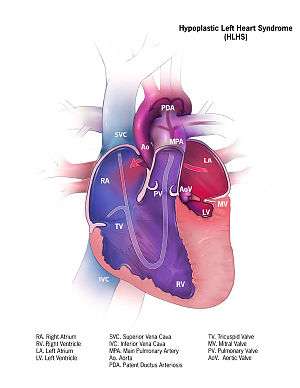 | |
| Illustration of heart suffering from Hypoplastic left heart syndrome | |
| Classification and external resources | |
| Specialty | cardiology |
| ICD-10 | Q23.4 |
| ICD-9-CM | 746.7 |
| OMIM | 241550 |
| DiseasesDB | 31507 |
| MedlinePlus | 001106 |
| eMedicine | ped/1131 |
| MeSH | C14.240.400.625 |
Hypoplastic left heart syndrome (HLHS) is a rare congenital heart defect in which the left heart is severely underdeveloped. The International Working Group for Mapping and Coding of Nomenclatures for Paediatric and Congenital Heart Disease defined HLHS as[1]
... a spectrum of cardiac malformations with normally aligned great arteries without a common atrioventricular junction, characterized by underdevelopment of the left heart with significant hypoplasia of the left ventricle including atresia, stenosis, or hypoplasia of the aortic or mitral valve, or both valves, and hypoplasia of the ascending aorta and aortic arch.— Tchervenkov et al., p. 344

Signs and symptoms

In typical anatomy, the left side of the heart receives oxygen-rich blood from the lungs and pumps it to the rest of the body. In people with HLHS, the aorta and left ventricle are underdeveloped (beginning in utero),[2] and the aortic and mitral valves are either too small to allow sufficient blood flow or are atretic (closed) altogether.[3] As blood returns from the lungs to the left atrium, it must pass through an atrial septal defect to the right side of the heart so it can be pumped to the rest of the body. This blood must flow through a patent (open) ductus arteriosus. Since the ductus arteriosus usually closes within eleven days after birth, blood flow may be severely restricted and eventually blocked, leading to dangerously low circulation and, eventually, shock. Babies are often cyanotic at birth to varying degrees, depending on the severity of their defects.
Causes

There is no known cause in the majority of HLHS cases.[4] There is likely a genetic component, as HLHS has been shown to be heritable and associated with specific gene mutations.[5][6]
In a retrospective analysis of over 1,300 newborns (born between 1996 and 2006) from 24 children’s hospitals in the United States, researchers at Cincinnati Children’s Hospital in Ohio found that babies with HLHS were more likely to be born in summer months, suggesting that seasonality and environmental factors play a significant role in causation.[7]
Genetics
HLHS usually occurs as an isolated cardiac defect. Genetic loci associated with HLHS include GJA1 (connexin 43), HAND1, NKX2.5, 10q, and 6q.[8][9] There is a slight risk of recurrence in future pregnancies, estimated to be 2-4%, which increases to 25% in families with two affected children.[4] HLHS has been seen in the following genetic syndromes: Trisomy 13 (Patau syndrome), Trisomy 18 (Edwards syndrome), Partial Trisomy 9, Turner's syndrome, Jacobsen syndrome, Holt-Oram Syndrome, and Smith-Lemli-Opitz Syndrome.[8]
Management
Medical
Without life-prolonging interventions, HLHS is fatal, but with intervention, an infant may survive. A cardiothoracic surgeon may perform a series of operations or a full heart transplant. While surgical intervention has emerged as the standard of care in the United States, other national health systems, notably in France, approach diagnosis of HLHS in a more conservative manner, with an emphasis on termination of pregnancy or compassionate care after delivery.[10]
Before surgery, the ductus must be kept open to allow blood-flow using medication containing prostaglandin. Air with less oxygen than normal is used for infants with hypoplastic left heart syndrome. These low oxygen levels increases the pulmonary vascular resistance (PVR) and thus improve blood flow to the rest of the body, due to the greater pressure difference between the lungs and body. Achieving oxygen levels below atmosphere requires the use of inhaled nitrogen.[11] Nitric oxide is a potent pulmonary vasodilator, and thus reduces PVR and improves venous return. Any factor that increases PVR will impede right sided flow.[12][13]
Surgical
Surgical operations to assist with hypo-plastic left heart are complex and need to be individualized for each patient. A cardiologist must assess all medical and surgical options on a case-by-case basis.
Currently, infants undergo either the staged reconstructive surgery (Norwood or Sano procedure within a few days of birth, Glenn or Hemi-Fontan procedure at 3 to 6 months of age, and the Fontan procedure at 1 1/2 to 5 years of age) or cardiac transplantation.[14] Current expectations are that 70% of those with HLHS will reach adulthood.[8] Many studies show that the higher the volume (number of surgeries performed) at a hospital, the lower the mortality (death) rate.[15][16] Factors that increase an infant's risk include lower birth weight, additional congenital anomalies, a genetic syndrome or those with a highly restrictive atrial septum.) For patients without these additional risk factors, 5 year survival now approaches 80%. Further, studies show that about 50% of those children who survived surgery in the early development of staged reconstruction have developmental delay or need special education; about 25% of these surgical survivors have severe disabilities. There is growing evidence that while the incidence of developmental and behavioral disabilities continues to be higher than that in the general population, children operated upon in the more current era have shown significantly better neurological outcomes. An alternative to the traditional Norwood is the Hybrid procedure.
Some physicians offer "compassionate care", instead of the surgeries, which results in the child's death, usually within 2 weeks of birth. Compassionate care is overseen by a physician, and may be carried out either in the hospital or at home. However, due to the vast improvement of surgical intervention, with many hospitals achieving over 90% survival, there is debate on whether or not "compassionate care" should still be offered to families.[17] A study in 2003 concluded that a selection of physicians who are experts in the care of children with HLHS were evenly split when asked what they would do if their own children were born with HLHS, with 1/3 stating that they would choose surgery, 1/3 stating that they would choose palliative (compassionate) treatment without surgery, and 1/3 stating that they are uncertain which choice they would make.[18]
The three-stage procedure is a palliative procedure (not a cure), as the child's circulation is made to work with only two of the heart's four chambers.
Norwood procedure
The first step is the Norwood procedure.[19] In this procedure, the right ventricle is used to pump blood into the systemic circulation. Since the right ventricle is no longer directly pumping blood to the lungs, a shunt is required in order to pass deoxygenated blood through the lungs. Either the subclavian artery can be connected to the pulmonary circulation (Blalock-Taussig shunt), or a shunt is made directly from the right ventricle to the pulmonary circulation (Sano shunt). The narrow aorta is enlarged using a patch to improve blood flow to the body.[20]
During this time the baby may be medically fragile and have feeding problems because the heart is working very hard. There is a considerable degree of venous mixing in the right ventricle, leading to lower oxygenation saturation. In addition, both the Blalock-Taussig and the Sano shunts expose the lungs to systemic arterial pressures, leading to long-term pulmonary hypertension and eventually heart failure.[19]
Hybrid procedure
The Hybrid procedure may be used in place of the Norwood.[19][21][22] The Hybrid procedure does not necessitate the use of heart-lung bypass or performing a sternotomy. Instead of a six-hour surgery, the Hybrid typically takes one to two hours. In this procedure, a stent is placed in the ductus arteriosus to maintain its patency, and bands are placed over both the left and right pulmonary artery branches to limit pressure and over-circulation to the lungs.[23] Outcomes with the Hybrid approach are comparable to those with the Norwood.[24]
Glenn procedure
The second stage—the bidirectional Glenn or Hemi-Fontan (see also Kawashima procedure)—relieves some of the problems introduced by Stage I palliation.[19] In this operation, the superior vena cava is ligated from the heart and connected to the pulmonary circulation. At this time, the Blalock-Taussig or Sano shunt is taken down. The lungs are no longer exposed to systemic arterial pressures, but much lower venous pressures. Although venous blood from the upper half of the body is no longer mixing with oxygenated blood in the right ventricle, there is still venous mixing from the lower half of the body, leading to some degree of oxygen desaturation.[19]
Fontan procedure

The final procedure, the Fontan procedure, completes the repair of the hypoplastic left heart.[19] Although there are several variations, the functional effect is to redirect venous blood from the lower body (through the inferior vena cava) away from the right atrium to the pulmonary artery. This should eliminate any mixing of oxygenated and deoxygenated blood in the right ventricle. The right ventricle performs the traditional job of the left, supplying the body with oxygenated blood, while the passive systemic venous pressure performs the traditional job of the right, passing deoxygenated blood to the lungs.[19]
Prognosis
Early survival has improved since the introduction of the Norwood procedure.[8] Since there are no long-term studies of HLHS adults, statistics are usually derived from post-Fontan patients; it is estimated that 70% of HLHS patients will reach adulthood.[8]
As is true for patients with other types of heart defects involving malformed valves,[25] HLHS patients run a high risk of endocarditis, and must be monitored by a cardiologist for the rest of their lives to check on their heart function.
Heart transplantation may be indicated, typically after Fontan completion.[8] One multi-center study (of patients undergoing the Fontan from 1993-2001) reported a 76% 1-year survival rate in patients who survived to transplant.[26]
Epidemiology
The National Birth Defects Prevention Network estimates that birth defects occur in about 3% of live births in the United States; of these, HLHS occurs in 1 out of 4,344 live births, or an estimated total of 960 live births per year in the United States.[27][28][29] HLHS occurs at 1/6 the rate of the most common birth defect, trisomy 21 (Down syndrome).
References
- ↑ Tchervenkov, C. I., Jacobs, J. P., Weinberg, P. M., Aiello, V. D., Béland, M. J., Colan, S. D., ... & Stellin, G. (2006). "The nomenclature, definition and classification of hypoplastic left heart syndrome". Cardiology in the Young. 16 (04): 339–368. doi:10.1017/s1047951106000291. PMID 16839428.
- ↑ Galindo, A., Nieto, O., Villagrá, S., Grañeras, A., Herraiz, I., & Mendoza, A. (2009). "Hypoplastic left heart syndrome diagnosed in fetal life: associated findings, pregnancy outcome and results of palliative surgery". Ultrasound in Obstetrics & Gynecology. 33 (5): 560–566. doi:10.1002/uog.6355. PMID 19367583.
- ↑ Hypoplastic Left Heart Syndrome | Congenital Heart Disease - Cove Point Foundation | Johns Hopkins Children's Hospital
- 1 2 Barron, D. J., Kilby, M. D., Davies, B., Wright, J. G., Jones, T. J., & Brawn, W. J. (2009). "Hypoplastic left heart syndrome". The Lancet. 374 (9689): 551–564. doi:10.1016/s0140-6736(09)60563-8. PMID 19683641.
- ↑ Hinton, R. B., Martin, L. J., Tabangin, M. E., Mazwi, M. L., Cripe, L. H., & Benson, D. W. (2007). "Hypoplastic left heart syndrome is heritable". Journal of the American College of Cardiology. 50 (16): 1590–1595. doi:10.1016/j.jacc.2007.07.021. PMID 17936159.
- ↑ Dasgupta C, Martinez AM, Zuppan CW, Shah MM, Bailey LL, Fletcher WH (2001). "Identification of connexin43 (alpha1) gap junction gene mutations in patients with hypoplastic left heart syndrome by denaturing gradient gel electrophoresis (DGGE)". Mutat. Res. 479 (1–2): 173–86. doi:10.1016/S0027-5107(01)00160-9. PMID 11470490.
- ↑ Eghtesady P, Brar A, Hall M (February 2011). "Seasonality of hypoplastic left heart syndrome in the United States: a 10-year time-series analysis". J. Thorac. Cardiovasc. Surg. 141 (2): 432–8. doi:10.1016/j.jtcvs.2010.06.060. PMID 20817208.
- 1 2 3 4 5 6 Feinstein, JA; Benson, DW; Dubin, AM; Cohen, MS; Maxey, DM; Mahle, WT; Pahl, E; Villafañe, J; Bhatt, AB; Peng, LF; Johnson, BA; Marsden, AL; Daniels, CJ; Rudd, NA; Caldarone, CA; Mussatto, KA; Morales, DL; Ivy, DD; Gaynor, JW; Tweddell, JS; Deal, BJ; Furck, AK; Rosenthal, GL; Ohye, RG; Ghanayem, NS; Cheatham, JP; Tworetzky, W; Martin, GR (3 January 2012). "Hypoplastic left heart syndrome: current considerations and expectations.". Journal of the American College of Cardiology. 59 (1 Suppl): S1–42. doi:10.1016/j.jacc.2011.09.022. PMID 22192720.
- ↑ Hinton, R. B., Martin, L. J., Rame-Gowda, S., Tabangin, M. E., Cripe, L. H., & Benson, D. W. (2009). "Hypoplastic left heart syndrome links to chromosomes 10q and 6q and is genetically related to bicuspid aortic valve". Journal of the American College of Cardiology. 53 (12): 1065–1071. doi:10.1016/j.jacc.2008.12.023. PMC 2703749
 . PMID 19298921.
. PMID 19298921. - ↑ Noseda C, Mialet-Marty T, Basquin A (April 2012). "Hypoplasies sévères du ventricule gauche : soins palliatifs après un diagnostic prénatal". Archives de pediatrie. 19 (4): 374–380. doi:10.1016/j.arcped.2012.01.022. PMID 22397767.
- ↑ Green A, Pye S, Yetman AT (August 2002). "The physiologic basis for and nursing considerations in the use of subatmospheric concentrations of oxygen in HLHS". Advances in Neonatal Care. 2 (4): 177–86. doi:10.1053/adnc.2002.33542. PMID 12881932.
- ↑ Khambadkone S.; Li J.; De Leval M. R.; Cullen S.; Deanfield J. E.; Redington A. N. (2003). "Basal pulmonary vascular resistance and nitric oxide responsiveness late after Fontan-type operation". Circulation. 107 (25): 3204–3208. doi:10.1161/01.cir.0000074210.49434.40.
- ↑ Norwood W. I. (1991). "Hypoplastic left heart syndrome. The". Annals of Thoracic Surgery. 52 (3): 688–695. doi:10.1016/0003-4975(91)90978-y.
- ↑ Hypoplastic Left Heart Syndrome (HLHS) | The Children's Hospital of Philadelphia
- ↑ McHugh, KE; Hillman, DG; Gurka, MJ; Gutgesell, HP (Jan–Feb 2010). "Three-stage palliation of hypoplastic left heart syndrome in the University HealthSystem Consortium". Congenital heart disease. 5 (1): 8–15. doi:10.1111/j.1747-0803.2009.00367.x. PMID 20136852.
- ↑ Hirsch, JC; Gurney, JG; Donohue, JE; Gebremariam, A; Bove, EL; Ohye, RG (July 2008). "Hospital mortality for Norwood and arterial switch operations as a function of institutional volume". Pediatric cardiology. 29 (4): 713–7. doi:10.1007/s00246-007-9171-2. PMID 18080151.
- ↑ Wernovsky, Gil (1 September 2008). "The Paradigm Shift Toward Surgical Intervention for Neonates With Hypoplastic Left Heart Syndrome". Archives of Pediatrics & Adolescent Medicine. 162 (9): 849–54. doi:10.1001/archpedi.162.9.849. PMID 18762602.
- ↑ Kon, Alexander A.; Ackerson, Lynn; Lo, Bernard (31 May 2003). "Choices physicians would make if they were the parents of a child with hypoplastic left heart syndrome". The American Journal of Cardiology. 91 (12): 1506–1509. doi:10.1016/S0002-9149(03)00412-0. PMID 12804748.
- 1 2 3 4 5 6 7 Feinstein, Jeffrey A.; Benson, D. Woodrow; Dubin, Anne M.; Cohen, Meryl S.; Maxey, Dawn M.; Mahle, William T.; Pahl, Elfriede; Villafañe, Juan; Bhatt, Ami B. (Jan 2012). "Hypoplastic Left Heart Syndrome". Journal of the American College of Cardiology. 59 (1): S1–S42. doi:10.1016/j.jacc.2011.09.022. PMID 22192720.
- ↑ "new norwood.gif". Archived from the original on November 24, 2010.
- ↑ Murphy, Michael O.; Bellsham-Revell, Hannah; Morgan, Gareth J.; Krasemann, Thomas; Rosenthal, Eric; Qureshi, Shakeel A.; Salih, Caner; Austin, Conal B.; Anderson, David R. "Hybrid Procedure for Neonates With Hypoplastic Left Heart Syndrome at High-Risk for Norwood: Midterm Outcomes". The Annals of Thoracic Surgery. 100: 2286–2292. doi:10.1016/j.athoracsur.2015.06.098.
- ↑ Chauhan, Monika; Mastropietro, Christopher W. "Hypoplastic Left Heart Syndrome in the Emergency Department: An Update". The Journal of Emergency Medicine. 46 (2): e51–e54. doi:10.1016/j.jemermed.2013.08.061.
- ↑ Children's Hospital Boston | Pediatric Views
- ↑ Galantowicz M, Cheatham JP, Phillips A, et al. (June 2008). "Hybrid approach for hypoplastic left heart syndrome: intermediate results after the learning curve". Ann. Thorac. Surg. 85 (6): 2063–70; discussion 2070–1. doi:10.1016/j.athoracsur.2008.02.009. PMID 18498821.
- ↑ "Endocarditis: Risk factors". MayoClinic.com. Retrieved 2007-10-23.
- ↑ Taylor, D. O., Stehlik, J., Edwards, L. B., Aurora, P., Christie, J. D., Dobbels, F., ... & Hertz, M. I. (2009). "Registry of the International Society for Heart and Lung Transplantation: twenty-sixth official adult heart transplant report—2009.". The Journal of Heart and Lung Transplantation. 28 (10): 1007–1022. doi:10.1016/j.healun.2009.08.014. PMID 19782283.
- ↑ CDC - Congenital Heart Defects, Facts about Hypoplastic Left Heart Syndrome - NCBDDD
- ↑ CDC Data & Statistics | Feature: Updated Estimates for Selected Birth Defects
- ↑ Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, Correa A; National Birth Defects Prevention Network. (2010). "Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004-2006.". Birth Defects Res A Clin Mol Teratol. 88 (12): 1008–16. doi:10.1002/bdra.20735. PMID 20878909.
Further reading
- Mastropietro CW, Clark JA, Grimaldi L, Killinger J, Richmond M. The Infant with a Single Cardiac Ventricle. Current Pediatric Reviews 2012, 8: 253–276. http://www.eurekaselect.com/101572/article
External links
| Wikimedia Commons has media related to Hypoplastic left heart syndrome. |
- Hypoplastic Left Heart Syndrome - Stanford Children's Health
- Hypoplastic Left Heart Syndrome Program from Mayo Clinic HLHS Cause to Cure
- HLHS Information Page Questions to ask medical professionals and insurance company, plus resources
- Hypoplastic Left Heart Syndrome information from Seattle Children's Hospital Heart Center
- Card-AG, The Cardiologycal Working Group of the University Pediatric Clinic Munster
- Hypoplastic Left Heart Syndrome, American Heart Association
- Overview at Cincinnati Children's Hospital Medical Center
- Overview at University of Michigan Congenital Heart Center
- Cardiac Center at The Children's Hospital of Philadelphia
- Hypoplastic left heart syndrome information for parents.
- Little Hearts Matter, a charity providing support and information on HLHS and other single ventricle heart defects
- Baby Hearts Press
- www.congenitalheartdefects.com
- 120+ stories of children born with Hypoplastic Left Heart Syndrome hosted by the The Congenital Heart Information Network.
- HLHS email support groups/discussion list hosted by the The Congenital Heart Information Network (membership required).
- Little Hearts, Inc. — Providing hope with stories of children with HLHS and other CHDs. Email support group (membership required)
- HeartLine, a charity for children with heart conditions and their families
- Designer Heart, A Congenital Heart Defect Network.
- It's My Heart, a non-profit organization created to provide support to and advocating for those affected by Acquired and Congenital Heart Defects.