Hydroxylapatite
| Hydroxylapatite | |
|---|---|
|
Hydroxylapatite crystals on matrix | |
| General | |
| Category |
Phosphate mineral Apatite group |
| Formula (repeating unit) | Ca5(PO4)3(OH) |
| Strunz classification | 8.BN.05 |
| Crystal system | Hexagonal |
| Crystal class |
Dipyramidal (6/m) H-M Symbol (6/m) |
| Space group | P63/m |
| Unit cell | a = 9.41 Å, c = 6.88 Å; Z = 2 |
| Identification | |
| Formula mass | 502.31 g/mol |
| Color | Colorless, white, gray, yellow, yellowish green |
| Crystal habit | As tabular crystals and as stalagmites, nodules, in crystalline to massive crusts |
| Cleavage | Poor on {0001} and {1010} |
| Fracture | Conchoidal |
| Tenacity | Brittle |
| Mohs scale hardness | 5 |
| Luster | Vitreous to subresinous, earthy |
| Streak | White |
| Diaphaneity | Transparent to translucent |
| Specific gravity | 3.14–3.21 (measured), 3.16 (calculated) |
| Optical properties | Uniaxial (-) |
| Refractive index | nω = 1.651 nε = 1.644 |
| Birefringence | δ = 0.007 |
| References | [1][2][3] |
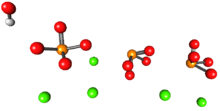
Hydroxylapatite, also called hydroxyapatite (HA), is a naturally occurring mineral form of calcium apatite with the formula Ca5(PO4)3(OH), but is usually written Ca10(PO4)6(OH)2 to denote that the crystal unit cell comprises two entities. Hydroxylapatite is the hydroxyl endmember of the complex apatite group. The OH− ion can be replaced by fluoride, chloride or carbonate, producing fluorapatite or chlorapatite. It crystallizes in the hexagonal crystal system. Pure hydroxylapatite powder is white. Naturally occurring apatites can, however, also have brown, yellow, or green colorations, comparable to the discolorations of dental fluorosis.
Up to 50% by volume and 70% by weight of human bone is a modified form of hydroxylapatite (known as bone mineral).[4] Carbonated calcium-deficient hydroxylapatite is the main mineral of which dental enamel and dentin are composed. Hydroxylapatite crystals are also found in the small calcifications (within the pineal gland and other structures) known as corpora arenacea or 'brain sand'.
Chemical synthesis of hydroxyapatite
Hydroxyapatite can be synthesized via several methods such as wet chemical deposition, biomimetic deposition, sol-gel route (wet-chemical precipitation) or electrodeposition.[5] Yagai and Aoki proposed the hydroxyapatite nanocrystal suspension can be prepared by a wet chemical precipitation reaction following the reaction equation below:[6]
10 Ca(OH)2 + 6 H3PO4 → Ca10(PO4)6(OH)2 + 18 H2O
Several studies have shown that hydroxyapatite synthesis via wet-chemical route can be improved by power ultrasound. The ultrasonically assisted synthesis (sono-synthesis) of hydroxyapatite is a successful technique to produce nanostructured hydroxyapatite at high quality standards. The ultrasonic route allows to produce nano-crystalline hydroxyapatite as well as modified particles, e.g. core-shell nanospheres, and composites.[7]
Calcium deficient hydroxyapatite
Calcium deficient (non-stochiometric) hydroxyapatite, Ca10-x(PO4)6-x(HPO4)x(OH)2-x (where x is between 0 and 1) has a Ca/P ratio between 1.67 and 1.5. The Ca/P ratio is often used in the discussion of calcium phosphate phases.[8] Stoichiometric apatite Ca10(PO4)6(OH)2 has a Ca/P ratio of 10:6 normally expressed as 1.67. The non-stoichiometric phases have the hydroxyapatite structure with cation vacancies (Ca2+) and anion (OH–) vacancies. The sites occupied solely by phosphate anions in stochiometric hydroxyapatite, are occupied by phosphate or hydrogen phosphate, HPO42–, anions.[8] Preparation of these calcium deficient phases can be prepared by precipitation from a mixture of calcium nitrate and diammonium phosphate with the desired Ca/P ratio, for example to make a sample with a Ca/P ratio of 1.6:[9]
- 9.6 Ca(NO3)2 + 6 (NH4)2HPO4 → Ca9.6(PO4)5.6(HPO4)0.4(OH)1.6
Sintering these non-stoichiometric phases forms a solid phase which is an intimate mixture of tricalcium phosphate and hydroxyapatite, termed biphasic calcium phosphate:[10]
- Ca10-x(PO4)6-x(HPO4)x(OH)2-x → (1-x) Ca10(PO4)6(OH)2 + 3x Ca3(PO4)2
Medical uses

Hydroxylapatite can be found in teeth and bones within the human body. Thus, it is commonly used as a filler to replace amputated bone or as a coating to promote bone ingrowth into prosthetic implants.[11] Although many other phases exist with similar or even identical chemical makeup, the body responds to them very differently. Coral skeletons can be transformed into hydroxylapatite by high temperatures; their porous structure allows relatively rapid ingrowth at the expense of initial mechanical strength. The high temperature also burns away any organic molecules such as proteins, preventing an immune response and rejection.
Many modern implants, e.g. hip replacements, dental implants and bone conduction implants, are coated with hydroxylapatite. It has been suggested that this may promote[12] osseointegration. Porous hydroxylapatite implants are used for local drug delivery in bone.[13][14] It is also being used to repair early lesions in tooth enamel.[15]
In spite of attractive biological properties, hydroxylapatite, and materials based thereon, have some drawbacks, such as low bioresorption rate in vivo, poor stimulating effect on the growth of new bone tissues, low crack resistance and small fatigue durability in the physiological environment. The application of modified hydroxylapatite opens up the opportunities for the preparation of artificial bone substances for implants and a large variety of drugs for curing different lesions of bone, soft and mucous tissues of the individual. A promising method of modification is the introduction of fluorine or silicon into the primary structure with the formation of fluorine- or silicon-substituted hydroxylapatite.[16] The introduction of fluorine increases the resistance to biodegradation[17] and improves the adsorption of proteins and adhesion of the coating to the metal substrate.[18]
Pathology
Hydroxylapatite deposits in tendons around joints resulting in the medical condition calcific tendinitis.
Supplement
Microcrystalline hydroxylapatite (MH) is marketed as a "bone-building" supplement with superior absorption in comparison to calcium.[19] It is a second-generation calcium supplement derived from bovine bone.[19] In the 1980s, bone meal calcium supplements were found to be contaminated with heavy metals,[19] and although the manufacturers claim their MH is free from contaminants, people are advised to avoid it because its effect in the body has not been well-tested.[19] However, the limited tests seem to show positive results. A 1995 randomized placebo-controlled study of 40 people in Europe found that it was more effective than calcium carbonate in slowing bone loss.[19] A 2007 randomized double-blind controlled study of an MH supplement called the Bone Builder found significant positive effects in bone mineral density (BMD) compared to control.[20] Hydroxylapatite has been used by Noel Fitzpatrick to facilitate bionic development in animals, by coating steel rods in hydroxylapatite to encourage natural growth of skin around it. As a component of nanocomposites, hydroxylapatite is finding uses as a potential new bone replacement materials.
Chromatography
The mechanism of hydroxylapatite (HA) chromatography is complicated and has been described as "mixed-mode" ion exchange. It involves nonspecific interactions between positively charged calcium ions and negatively charged phosphate ions on the stationary phase HA resin with protein negatively charged carboxyl groups and positively charged amino groups. It may be difficult to predict the effectiveness of HA chromatography based on physical and chemical properties of the desired protein to be purified. For elution, a buffer with increasing phosphate concentration is typically used for application.
Use in archaeology
In archaeology, hydroxylapatite from human and animal remains can be analysed to reconstruct ancient diets, migrations and palaeoclimate. The mineral fractions of bone and teeth act as a reservoir of trace elements, including carbon, oxygen and strontium. Stable isotope analysis of human and faunal hydroxylapatite can be used to indicate whether a diet was predominantly terrestrial or marine in nature (carbon, strontium);[21] the geographical origin and migratory habits of an animal or human (oxygen, strontium)[22] and to reconstruct past temperatures and climate shifts (oxygen).[23] Post-depositional alteration of bone can contribute to the degradation of bone collagen, the protein required for stable isotope analysis.[24]
Animal structures and potential uses in materials science
The clubbing appendages of the Odontodactylus scyllarus (peacock mantis shrimp) are made of an extremely dense form of the mineral which has a higher specific strength and toughness than any synthetic composite material; these properties have led to its investigation for potential synthesis and engineering use.[25] Their dactyl appendages have excellent impact resistance due to the impact region being composed of mainly crystalline hydroxyapatite, which offers significant hardness. Crack propagation of the impact region is reduced by thin layers of chitosan in between the highly organized crystal hydroxyapatite structures. Once a hydroxyapatite prism fractures, the chitosan inter-layers aid in preventing further cracks. This form of layered crack retardation is also seen in teeth enamel, where the hydroxyapatite prisms that make up an enamel rod are padded by thin layers of protein which fulfill the same function.[26] A periodic layer underneath the impact layer composed of hydroxyapatite with lower calcium and phosphorus content (thus resulting in a much lower modulus) inhibits crack growth by forcing new cracks to change directions. This periodic layer also reduces the energy transferred across both layers due to the large difference in modulus, even reflecting some of the incident energy.[27] Armor models based on nanoscale composites of hydroxyapatite designed in a similar fashion would help optimize impact resistance, reducing the weight needed to produce armor.[28]
The addition of hydroxyapatite particles to a magnesium alloy in the form of a metal matrix composite stabilized the corrosion rate of the alloy, resulting in a cyto-compatible, biodegradable material with adjustable corrosion rates and mechanical properties.[29]
Experimental nanostructure composite air filters containing hydroxyapatite were found to be efficient in absorbing and decomposing CO which could eventually lead to utilization in reducing automotive exhaust pollutants.[30]
In 2014 an alginate/nano-hydroxyapatite composite was synthesized and field-tested as an adsorbent for fluoride. The biocomposite removes fluoride through an ion-exchange mechanism, and is both biocompatible and biodegradable.[31]
Research into hydroxyapatite's proton conductivity resulted in the diffusion path and conduction mechanism of the mineral, allowing for potential use as developmental material for energy conversion devices.[32]
Recent developments have allowed the synthesis of ceramic microspheres made from hydroxyapatite with a diameter of 1.5 micrometers; the microspheres can be utilized in a variety of fields including filters, grinding media, and light-weight concrete.[33][34]
See also
| Wikimedia Commons has media related to Apatit-(CaOH) (Hydroxylapatite). |
References
- ↑ Hydroxylapatite. Mindat
- ↑ Hydroxylapatite. Webmineral
- ↑ Anthony, John W.; Bideaux, Richard A.; Bladh, Kenneth W.; Nichols, Monte C., eds. (2000). "Hydroxylapatite". Handbook of Mineralogy (PDF). IV (Arsenates, Phosphates, Vanadates). Chantilly, VA, US: Mineralogical Society of America. ISBN 0962209732.
- ↑ Junqueira, Luiz Carlos; José Carneiro (2003). Foltin, Janet; Lebowitz, Harriet; Boyle, Peter J., eds. Basic Histology, Text & Atlas (10th ed.). McGraw-Hill Companies. p. 144. ISBN 0-07-137829-4.
Inorganic matter represents about 50% of the dry weight of bone ... crystals show imperfections and are not identical to the hydroxylapatite found in the rock minerals
- ↑ Ferraz, M. P.; Monteiro, F. J.; Manuel, C. M. (2004). "Hydroxyapatite nanoparticles: A review of preparation methodologies". Journal of applied biomaterials & biomechanics : JABB. 2 (2): 74–80. PMID 20803440.
- ↑ Bouyer, E.; Gitzhofer, F.; Boulos, M. I. (2000). "Morphological study of hydroxyapatite nanocrystal suspension". Journal of Materials Science: Materials in Medicine. 11 (8): 523–31. doi:10.1023/A:1008918110156. PMID 15348004.
- ↑ Sono-Synthesis of Nano-Hydroxyapatite. hielscher.com
- 1 2 Rey, C.; Combes, C.; Drouet, C.; Grossin, D. (2011). "1.111 – Bioactive Ceramics: Physical Chemistry". In Ducheyne, Paul. Comprehensive Biomaterials. 1. Elsevier. pp. 187–281. doi:10.1016/B978-0-08-055294-1.00178-1. ISBN 978-0-08-055294-1.
- ↑ Raynaud, S.; Champion, E.; Bernache-Assollant, D.; Thomas, P. (2002). "Calcium phosphate apatites with variable Ca/P atomic ratio I. Synthesis, characterisation and thermal stability of powders". Biomaterials. 23 (4): 1065–72. doi:10.1016/S0142-9612(01)00218-6. PMID 11791909.
- ↑ Valletregi, M. (1997). "Synthesis and characterisation of calcium deficient apatite". Solid State Ionics. 101-103: 1279–1285. doi:10.1016/S0167-2738(97)00213-0.
- ↑ Sadat-Shojai, Mehdi (2010). Hydroxyapatite: Inorganic Nanoparticles of Bone (Properties, Applications, and Preparation Methodologies) (PDF). Iranian Students Book Agency (ISBA). ISBN 9786001020926.
- ↑ Jeong, KI (2012). "Experimental Study of Osseointegration and Stability of Intentionally Exposed Hydroxyapatite Coating Implants". Journal of the Korean Maxillofacial Reconstructive Surgery. 34 (1): 12–16.
- ↑ Kundu, B.; Soundrapandian, C.; Nandi, S. K.; Mukherjee, P.; Dandapat, N.; Roy, S.; Datta, B. K.; Mandal, T. K.; Basu, D.; Bhattacharya, R. N. (2010). "Development of new localized drug delivery system based on ceftriaxone-sulbactam composite drug impregnated porous hydroxyapatite: a systematic approach for in vitro and in vivo animal trial". Pharmaceutical Research. 27 (8): 1659–76. doi:10.1007/s11095-010-0166-y. PMID 20464462.
- ↑ Kundu, B.; Lemos, A.; Soundrapandian, C.; Sen, P. S.; Datta, S.; Ferreira, J. M. F.; Basu, D. (2010). "Development of porous HAp and β-TCP scaffolds by starch consolidation with foaming method and drug-chitosan bilayered scaffold based drug delivery system". Journal of Materials Science: Materials in Medicine. 21 (11): 2955–69. doi:10.1007/s10856-010-4127-0. PMID 20644982.
- ↑ Brunton, P. A.; Davies, R. P. W.; Burke, J. L.; Smith, A.; Aggeli, A.; Brookes, S. J.; Kirkham, J. (2013). "Treatment of early caries lesions using biomimetic self-assembling peptides – a clinical safety trial". BDJ. 215 (4): E6. doi:10.1038/sj.bdj.2013.741. PMID 23969679.
- ↑ Bogdanova, E.A.; Sabirzyanov, N. A. (2014). "Adsorption capacity of wateroxidized lanthanum-doped aluminum alloy powder" (PDF). Nanosystems: physics, chemistry, mathematics. 5 (4): 590–596.
- ↑ Cheng, Kui; Weng, Wenjian; Qu, Haibo; Du, Piyi; Shen, Ge; Han, Gaorong; Yang, Juan; Ferreira, J. M. F. (15 April 2004). "Sol-gel preparation andin vitro test of fluorapatite/hydroxyapatite films". Journal of Biomedical Materials Research. 69B (1): 33–37. doi:10.1002/jbm.b.20027.
- ↑ Zhang, Sam; Xianting, Zeng; Yongsheng, Wang; Kui, Cheng; Wenjian, Weng (June 2006). "Adhesion strength of sol–gel derived fluoridated hydroxyapatite coatings". Surface and Coatings Technology. 200 (22-23): 6350–6354. doi:10.1016/j.surfcoat.2005.11.033.
- 1 2 3 4 5 Straub, D.A. (2007). "Calcium Supplementation in Clinical Practice: A Review of Forms, Doses, and Indications". NCP- Nutrition in Clinical Practice. 22 (3): 286–96. doi:10.1177/0115426507022003286. PMID 17507729.
- ↑ Tucker, L. A.; Nokes, N.; Adams, T. (2007). "Effect of a Dietary Supplement on Hip and Spine BMD". Medicine & Science in Sports & Exercise. 39: S230. doi:10.1249/01.mss.0000273874.34214.2e.
- ↑ Richards, M. P.; Schulting, R. J.; Hedges, R. E. M. (2003). "Archaeology: Sharp shift in diet at onset of Neolithic" (PDF). Nature. 425 (6956): 366. Bibcode:2003Natur.425..366R. doi:10.1038/425366a. PMID 14508478.
- ↑ Britton, K.; Grimes, V.; Dau, J.; Richards, M. P. (2009). "Reconstructing faunal migrations using intra-tooth sampling and strontium and oxygen isotope analyses: A case study of modern caribou (Rangifer tarandus granti)". Journal of Archaeological Science. 36 (5): 1163–1172. doi:10.1016/j.jas.2009.01.003.
- ↑ Daniel Bryant, J.; Luz, B.; Froelich, P. N. (1994). "Oxygen isotopic composition of fossil horse tooth phosphate as a record of continental paleoclimate". Palaeogeography, Palaeoclimatology, Palaeoecology. 107 (3–4): 303–316. doi:10.1016/0031-0182(94)90102-3.
- ↑ Van Klinken, G. J. (1999). "Bone Collagen Quality Indicators for Palaeodietary and Radiocarbon Measurements". Journal of Archaeological Science. 26 (6): 687–695. doi:10.1006/jasc.1998.0385.
- ↑ Weaver, J. C.; Milliron, G. W.; Miserez, A.; Evans-Lutterodt, K.; Herrera, S.; Gallana, I.; Mershon, W. J.; Swanson, B.; Zavattieri, P.; Dimasi, E.; Kisailus, D. (2012). "The Stomatopod Dactyl Club: A Formidable Damage-Tolerant Biological Hammer". Science. 336 (6086): 1275–80. Bibcode:2012Sci...336.1275W. doi:10.1126/science.1218764. PMID 22679090.
- ↑ Simmons, L. M.; Al-Jawad, M.; Kilcoyne, S. H.; Wood, D. J. (2011). "Distribution of enamel crystallite orientation through an entire tooth crown studied using synchrotron X-ray diffraction". European Journal of Oral Sciences. 119: 19–24. doi:10.1111/j.1600-0722.2011.00909.x.
- ↑ Tanner, K. E. (2012). "Small but Extremely Tough". Science. 336 (6086): 1237–8. Bibcode:2012Sci...336.1237T. doi:10.1126/science.1222642. PMID 22679085.
- ↑ Barthelat, F.; Rabiei, R. (2011). "Toughness amplification in natural composites". Journal of the Mechanics and Physics of Solids. 59 (4): 829–840. doi:10.1016/j.jmps.2011.01.001.
- ↑ Witte, F.; Feyerabend, F.; Maier, P.; Fischer, J.; Störmer, M.; Blawert, C.; Dietzel, W.; Hort, N. (2007). "Biodegradable magnesium–hydroxyapatite metal matrix composites". Biomaterials. 28 (13): 2163–2174. doi:10.1016/j.biomaterials.2006.12.027.
- ↑ Nasr-Esfahani, M.; Fekri, S. (2012). "Alumina/TiO2/hydroxyapatite interface nanostructure composite filters as efficient photocatalysts for the purification of air". Reaction Kinetics, Mechanisms and Catalysis. 107: 89–103. doi:10.1007/s11144-012-0457-x.
- ↑ Pandi, K.; Viswanathan, N. (2014). "Synthesis of alginate bioencapsulated nano-hydroxyapatite composite for selective fluoride sorption". Carbohydrate Polymers. 112: 662–667. doi:10.1016/j.carbpol.2014.06.029.
- ↑ Yashima, M.; Kubo, N.; Omoto, K.; Fujimori, H.; Fujii, K.; Ohoyama, K. (2014). "Diffusion Path and Conduction Mechanism of Protons in Hydroxyapatite". The Journal of Physical Chemistry C. 118 (10): 5180–5187. doi:10.1021/jp412771f.
- ↑ Li, S.; Wu, H. H.; Xu, G. J.; Xiao, X. F. (2014). "Facile Biomimetic Fabrication of Hollow Hydroxyapatite with Hierarchically Porous Microstructure Using Hyperbranched Gemini Surfactant as Template". Advanced Materials Research. 1015: 355–358. doi:10.4028/www.scientific.net/AMR.1015.355.
- ↑ Korolev, E. V.; Inozemtcev, A. S. (2013). "Preparation and Research of the High-Strength Lightweight Concrete Based on Hollow Microspheres". Advanced Materials Research. 746: 285–288. doi:10.4028/www.scientific.net/AMR.746.285.
