Hallucination
| Hallucination | |
|---|---|
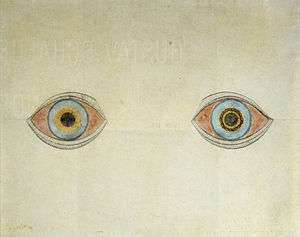 | |
| My eyes at the moment of the apparitions by August Natterer, a German artist who created many drawings of his hallucinations. | |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | R44 |
| ICD-9-CM | 780.1 |
| DiseasesDB | 19769 |
| MedlinePlus | 003258 |
| Patient UK | Hallucination |
| MeSH | D006212 |
A hallucination is a perception in the absence of external stimulus that has qualities of real perception. Hallucinations are vivid, substantial, and are perceived to be located in external objective space. They are distinguishable from these related phenomena: dreaming, which does not involve wakefulness; illusion, which involves distorted or misinterpreted real perception; imagery, which does not mimic real perception and is under voluntary control; and pseudohallucination, which does not mimic real perception, but is not under voluntary control.[1] Hallucinations also differ from "delusional perceptions", in which a correctly sensed and interpreted stimulus (i.e., a real perception) is given some additional (and typically absurd) significance.
Hallucinations can occur in any sensory modality—visual, auditory, olfactory, gustatory, tactile, proprioceptive, equilibrioceptive, nociceptive, thermoceptive and chronoceptive.
A mild form of hallucination is known as a disturbance, and can occur in most of the senses above. These may be things like seeing movement in peripheral vision, or hearing faint noises and/or voices. Auditory hallucinations are very common in schizophrenia. They may be benevolent (telling the subject good things about themselves) or malicious, cursing the subject etc. Auditory hallucinations of the malicious type are frequently heard, for example people talking about the subject behind his/her back. Like auditory hallucinations, the source of the visual counterpart can also be behind the subject's back. Their visual counterpart is the feeling of being looked or stared at, usually with malicious intent. Frequently, auditory hallucinations and their visual counterpart are experienced by the subject together.
Hypnagogic hallucinations and hypnopompic hallucinations are considered normal phenomena. Hypnagogic hallucinations can occur as one is falling asleep and hypnopompic hallucinations occur when one is waking up. Hallucinations can be associated with drug use (particularly deliriants), sleep deprivation, psychosis, neurological disorders, and delirium tremens.
The word "hallucination" itself was introduced into the English language by the 17th century physician Sir Thomas Browne in 1646 from the derivation of the Latin word alucinari meaning to wander in the mind.
Classification
Hallucinations may be manifested in a variety of forms.[2] Various forms of hallucinations affect different senses, sometimes occurring simultaneously, creating multiple sensory hallucinations for those experiencing them.
Visual
A visual hallucination is "the perception of an external visual stimulus where none exists".[3] Alternatively, a visual illusion is a distortion of a real external stimulus. Visual hallucinations are separated into simple and complex.
- Simple visual hallucinations (SVH) are also referred to as non-formed visual hallucinations and elementary visual hallucinations. These terms refer to lights, colors, geometric shapes, and indiscrete objects. These can be further subdivided into phosphenes which are SVH without structure, and photopsias which are SVH with geometric structures.
- Complex visual hallucinations (CVH) are also referred to as formed visual hallucinations. CVHs are clear, lifelike images or scenes such as people, animals, objects, etc.
For example, one may report hallucinating a giraffe. A simple visual hallucination is an amorphous figure that may have a similar shape or color to a giraffe (looks like a giraffe), while a complex visual hallucination is a discrete, lifelike image that is, unmistakably, a giraffe.
Auditory
Auditory hallucinations (also known as paracusia)[4] are the perception of sound without outside stimulus. Auditory hallucinations are the most common type of hallucination.[5] Auditory hallucinations can be divided into two categories: elementary and complex. Elementary hallucinations are the perception of sounds such as hissing, whistling, an extended tone, and more. In many cases, tinnitus is an elementary auditory hallucination. However, some people who experience certain types of tinnitus, especially pulsatile tinnitus, are actually hearing the blood rushing through vessels near the ear. Because the auditory stimulus is present in this situation, it does not qualify as a hallucination.
Complex hallucinations are those of voices, music, or other sounds that may or may not be clear, may be familiar or completely unfamiliar, and friendly or aggressive, among other possibilities. A hallucination of a single individual person of one or more talking voices are particularly associated with psychotic disorders such as schizophrenia, and hold special significance in diagnosing these conditions.
If a group of people experience a complex auditory hallucination, no single individual can be named psychotic or schizophrenic.[6][7][8][9]
Another typical disorder where auditory hallucinations are very common is dissociative identity disorder. In schizophrenia voices are normally perceived coming from outside the person but in dissociative disorders they are perceived as originating from within the person, commenting in their head not behind their back. Differential diagnosis between schizophrenia and dissociative disorders is challenging due to many overlapping symptoms especially scheinedrian first rank symptoms such as hallucinations.[10] However, many people not suffering from diagnosable mental illness may sometimes hear voices as well.[11] One important example to consider when forming a differential diagnosis for a patient with paracusia is lateral temporal lobe epilepsy. Despite the tendency to associate hearing voices, or otherwise hallucinating, and psychosis with schizophrenia or other psychiatric illnesses, it is crucial to take into consideration that, even if a person does exhibit psychotic features, he/she does not necessarily suffer from a psychiatric disorder on its own. Disorders such as Wilson's disease, various endocrine diseases, numerous metabolic disturbances, multiple sclerosis, systemic lupus erythematosus, porphyria, sarcoidosis, and many others can present with psychosis.
Musical hallucinations are also relatively common in terms of complex auditory hallucinations and may be the result of a wide range of causes ranging from hearing-loss (such as in musical ear syndrome, the auditory version of Charles Bonnet syndrome), lateral temporal lobe epilepsy,[12] arteriovenous malformation,[13] stroke, lesion, abscess, or tumor.[14]
The Hearing Voices Movement is a support and advocacy group for people who hallucinate voices, but do not otherwise show signs of mental illness or impairment.
High caffeine consumption has been linked to an increase in the likelihood of one's experiencing auditory hallucinations. A study conducted by the La Trobe University School of Psychological Sciences revealed that as few as five cups of coffee a day (approximately 500 mg of caffeine) could trigger the phenomenon.[15]
Command
Command hallucinations are hallucinations in the form of commands; they can be auditory or inside of the person's mind and/or consciousness.[16] The contents of the hallucinations can range from the innocuous to commands to cause harm to the self or others.[16] Command hallucinations are often associated with schizophrenia. People experiencing command hallucinations may or may not comply with the hallucinated commands, depending on the circumstances. Compliance is more common for non-violent commands.[17]
Command hallucinations are sometimes used in defense of a crime, often homicides.[18] In essence, it is a voice that one hears and it tells the listener what to do. Sometimes the commands are quite benign directives such as "Stand up" or "Shut the door."[19] Whether it is a command for something simple or something that is a threat, it is still considered a "command hallucination." Some helpful questions that can assist one in figuring out if he/she may be suffering from this include: "What are the voices telling you to do?", "When did your voices first start telling you to do things?", "Do you recognize the person who is telling you to harm yourself (or others)?", "Do you think you can resist doing what the voices are telling you to do?"[19]
Command hallucinations are sometimes referred to as "instructions" by patients. Usually, the beginning of these commands leads to lifestyle changes such as quitting work as the command tells them to do so. Many patients think of these commands as supernatural phenomenon because they seem intelligent. When command hallucinations are coupled with schizophrenia, a person can suffer a lot of abuses.
Example instructions or commands can be to speak specifically, hit a family member, or to shout at someone for a short or long duration. Patients suffering from a command hallucination do not have any choice but to obey. Some say their shoulders get tight when a command or instruction is given and they have no option but to act on the command. This can be a repeatedly occurring problem. Besides that, commands can be to keep in touch with a specific person by writing them an email or calling them on the phone and talking with or without a specific topic in mind.
Sometimes, these commands and hallucinations promise a better life after completion of a milestone. These promises are never met, and the episodes of command hallucinations keep stretching on.
There have been instances of recovery from Command Hallucinations. In a subject the period lasted for 7 years before it vanished mostly by itself.
Olfactory
Phantosmia (olfactory hallucinations), smelling an odor that is not actually there,[20] and parosmia (olfactory illusions), inhaling a real odor but perceiving it as different scent than remembered,[21] are distortions to the sense of smell (olfactory system) that, in most cases, are not caused by anything serious and usually go away on their own in time.[20] It can result from a range of conditions such as nasal infections, nasal polyps, dental problems, migraines, head injuries, seizures, strokes, or brain tumors.[20][22] Environmental exposures are sometimes the cause as well, such as smoking, exposure to certain types of chemicals (e.g., insecticides or solvents), or radiation treatment for head or neck cancer.[20] It can also be a symptom of certain mental disorders such as depression, bipolar disorder, intoxication or withdrawal from drugs and alcohol, or psychotic disorders (e.g., schizophrenia).[22] The perceived odors are usually unpleasant and commonly described as smelling burned, foul spoiled, or rotten.[20]
Tactile
Tactile hallucinations are the illusion of tactile sensory input, simulating various types of pressure to the skin or other organs. One subtype of tactile hallucination, formication, is the sensation of insects crawling underneath the skin and is frequently associated with prolonged cocaine use.[23] However, formication may also be the result of normal hormonal changes such as menopause, or disorders such as peripheral neuropathy, high fevers, Lyme disease, skin cancer, and more.[23]
Gustatory
This type of hallucination is the perception of taste without a stimulus. These hallucinations, which are typically strange or unpleasant, are relatively common among individuals who have certain types of focal epilepsy, especially temporal lobe epilepsy. The regions of the brain responsible for gustatory hallucination in this case are the insula and the superior bank of the sylvian fissure.[24][25]
General somatic sensations
General somatic sensations of a hallucinatory nature are experienced when an individual feels that his body is being mutilated, i.e. twisted, torn, or disembowelled. Other reported cases are invasion by animals in the person's internal organs such as snakes in the stomach or frogs in the rectum. The general feeling that one's flesh is decomposing is also classified under this type of hallucination.[25]
Cause
Hallucinations can be caused by a number of factors.
Hypnagogic hallucination
These hallucinations occur just before falling asleep, and affect a high proportion of the population: in one survey 37% of the respondents experienced them twice a week.[26] The hallucinations can last from seconds to minutes; all the while, the subject usually remains aware of the true nature of the images. These may be associated with narcolepsy. Hypnagogic hallucinations are sometimes associated with brainstem abnormalities, but this is rare.[27]
Peduncular hallucinosis
Peduncular means pertaining to the peduncle, which is a neural tract running to and from the pons on the brain stem. These hallucinations usually occur in the evenings, but not during drowsiness, as in the case of hypnagogic hallucination. The subject is usually fully conscious and then can interact with the hallucinatory characters for extended periods of time. As in the case of hypnagogic hallucinations, insight into the nature of the images remains intact. The false images can occur in any part of the visual field, and are rarely polymodal.[27]
Delirium tremens
One of the more enigmatic forms of visual hallucination is the highly variable, possibly polymodal delirium tremens. Individuals suffering from delirium tremens may be agitated and confused, especially in the later stages of this disease. Insight is gradually reduced with the progression of this disorder. Sleep is disturbed and occurs for a shorter period of time, with rapid eye movement sleep.
Parkinson's disease and Lewy body dementia
Parkinson's disease is linked with Lewy body dementia for their similar hallucinatory symptoms. The symptoms strike during the evening in any part of the visual field, and are rarely polymodal. The segue into hallucination may begin with illusions[28] where sensory perception is greatly distorted, but no novel sensory information is present. These typically last for several minutes, during which time the subject may be either conscious and normal or drowsy/inaccessible. Insight into these hallucinations is usually preserved and REM sleep is usually reduced. Parkinson's disease is usually associated with a degraded substantia nigra pars compacta, but recent evidence suggests that PD affects a number of sites in the brain. Some places of noted degradation include the median raphe nuclei, the noradrenergic parts of the locus coeruleus, and the cholinergic neurons in the parabrachial area and pedunculopontine nuclei of the tegmentum.[27]
Migraine coma
This type of hallucination is usually experienced during the recovery from a comatose state. The migraine coma can last for up to two days, and a state of depression is sometimes comorbid. The hallucinations occur during states of full consciousness, and insight into the hallucinatory nature of the images is preserved. It has been noted that ataxic lesions accompany the migraine coma.[27]
Charles Bonnet syndrome
Charles Bonnet syndrome is the name given to visual hallucinations experienced by a partially or severely sight impaired person. The hallucinations can occur at any time and can distress people of any age, as they may not initially be aware that they are hallucinating, they may fear initially for their own mental health which may delay them sharing with carers what is happening until they start to understand it themselves. The hallucinations can frighten and disconcert as to what is real and what is not and carers need to learn how to support sufferers. The hallucinations can sometimes be dispersed by eye movements, or perhaps just reasoned logic such as, "I can see fire but there is no smoke and there is no heat from it" or perhaps "We have an infestation of rats but they have pink ribbons with a bell tied on their necks." Over elapsed months and years the manifestation of the hallucinations may change, becoming more or less frequent with changes in ability to see. The length of time that the sight impaired person can suffer from these hallucinations varies according to the underlying speed of eye deterioration. A differential diagnosis are ophthalmopathic hallucinations.[29]
Focal epilepsy
Visual hallucinations due to focal seizures differ depending on the region of the brain where the seizure occurs. For example, visual hallucinations during occipital lobe seizures are typically visions of brightly colored, geometric shapes that may move across the visual field, multiply, or form concentric rings and generally persist from a few seconds to a few minutes. They are usually unilateral and localized to one part of the visual field on the contralateral side of the seizure focus, typically the temporal field. However, unilateral visions moving horizontally across the visual field begin on the contralateral side and move toward the ipsilateral side.[24][30]
Temporal lobe seizures, on the other hand, can produce complex visual hallucinations of people, scenes, animals, and more as well as distortions of visual perception. Complex hallucinations may appear real or unreal, may or may not be distorted with respect to size, and may seem disturbing or affable, among other variables. One rare but notable type of hallucination is heautoscopy, a hallucination of a mirror image of one's self. These "other selves" may be perfectly still or performing complex tasks, may be an image of a younger self or the present self, and tend to be only briefly present. Complex hallucinations are a relatively uncommon finding in temporal lobe epilepsy patients. Rarely, they may occur during occipital focal seizures or in parietal lobe seizures.[24]
Distortions in visual perception during a temporal lobe seizure may include size distortion (micropsia or macropsia), distorted perception of movement (where moving objects may appear to be moving very slowly or to be perfectly still), a sense that surfaces such as ceilings and even entire horizons are moving farther away in a fashion similar to the dolly zoom effect, and other illusions.[31] Even when consciousness is impaired, insight into the hallucination or illusion is typically preserved.
Drug-induced hallucination
Drug-induced hallucinations are caused by the consumption of psychoactive substances such as deliriants, psychedelics, and certain stimulants, which are known to cause visual and auditory hallucinations. Some psychedelics such as lysergic acid diethylamide and psilocybin can cause hallucinations that range from a spectrum of mild to severe. Some of these drugs can be used in psychotherapy to treat mental disorders, addiction, anxiety, and secondary to advanced stage cancers.[32]
Sensory deprivation hallucination
Hallucinations can be caused by sense deprivation when it occurs for prolonged periods of time, and almost always occur in the modality being deprived (visual for blindfolded/darkness, auditory for muffled conditions, etc.)
Experimentally-induced hallucinations
Anomalous experiences, such as so-called benign hallucinations, may occur in a person in a state of good mental and physical health, even in the apparent absence of a transient trigger factor such as fatigue, intoxication or sensory deprivation. It is now widely recognized that hallucinatory experiences are not merely the prerogative of those suffering from mental illness, or normal people in abnormal states, but that they occur spontaneously in a significant proportion of the normal population, when in good health and not undergoing particular stress or other abnormal circumstance.
The evidence for this statement has been accumulating for more than a century. Studies of benign hallucinatory experiences go back to 1886 and the early work of the Society for Psychical Research,[33][34] which suggested approximately 10% of the population had experienced at least one hallucinatory episode in the course of their life. More recent studies have validated these findings; the precise incidence found varies with the nature of the episode and the criteria of ‘hallucination’ adopted, but the basic finding is now well-supported.[35]
Pathophysiology
Visual
Sometimes internal imagery can overwhelm the sensory input from external stimuli when sharing neural pathways, or if indistinct stimuli is perceived and manipulated to match one's expectations or beliefs, especially about the environment. This can result in a hallucination,[36] and this effect is sometimes exploited to form an optical illusion.
There are three pathophysiologic mechanisms thought to account for complex visual hallucinations. These mechanisms consist of the following:
- Irritation of cortical centers responsible for visual processing (e.g., seizure activity). The irritation of the primary visual cortex causes simple elementary visual hallucinations.
- Lesions that cause deafferentation of the visual system may lead to cortical release phenomenon, which includes visual hallucination.
- The reticular activating system, which has been linked to the genesis of visual hallucinations.[30]
Some specific classifications include: elementary hallucinations, which may entail flicks, specks, and bars of light (called phosphenes). Closed eye hallucinations in darkness, which are common to psychedelic drugs (i.e., LSD, mescaline). Scenic or "panoramic" hallucinations, which are not superimposed but vividly replace the entire visual field with hallucinatory content similarly to dreams;[37] such scenic hallucinations may occur in epilepsy[38] (in which they are usually stereotyped and experimental[39] in character), hallucinogen use,[37] and more rarely in catatonic schizophrenia[40][41] (cf. oneirophrenia), mania,[42] and brainstem lesions,[43] among others.
Another thing that may cause visual hallucinations is prolonged visual deprivation. In a study where 13 healthy people were blindfolded for 5 days, 10 out of the 13 subjects reported visual hallucinations. This finding lends strong support to the idea that the simple loss of normal visual input is sufficient to cause visual hallucinations.[30]
Psychodynamic view
Various theories have been put forward to explain the occurrence of hallucinations. When psychodynamic (Freudian) theories were popular in psychology, hallucinations were seen as a projection of unconscious wishes, thoughts, and wants. As biological theories have become orthodox, hallucinations are more often thought of (by psychologists at least) as being caused by functional deficits in the brain. With reference to mental illness, the function (or dysfunction) of the neurotransmitters glutamate and dopamine are thought to be particularly important.[44] The Freudian interpretation may have an aspect of truth, as the biological hypothesis explains the physical interactions in the brain, while the Freudian interpretation addresses the psychological complexes related to the content of the hallucination, such as hallucinating persecutory voices due to guilt. Psychological research has argued that hallucinations may result from biases in what are known as metacognitive abilities.[45]
Information processing perspective
These are abilities that allow us to monitor or draw inferences from our own internal psychological states (such as intentions, memories, beliefs and thoughts). The ability to discriminate between internal (self-generated) and external (stimuli) sources of information is considered to be an important metacognitive skill, but one which may break down to cause hallucinatory experiences. Projection of an internal state (or a person's own reaction to another's) may arise in the form of hallucinations, especially auditory hallucinations. A recent hypothesis that is gaining acceptance concerns the role of overactive top-down processing, or strong perceptual expectations, that can generate spontaneous perceptual output (that is, hallucination).[46]
Stages of hallucination
- Emergence of surprising or warded-off memory or fantasy images[47]
- Frequent reality checks[47]
- Last vestige of insight as hallucinations become indistinguishable from reality.[47]
- Fantasy and distortion elaborated upon and confused with actual perception[47]
- Internal-external boundaries destroyed and possible pantheistic (or personally felt or believed, possibly profound, internal spiritual or religious) experience[47]
Biological perspective
Auditory hallucinations
Auditory hallucinations are the most prevalent type of hallucinations. They include hearing voices and music. Many times an individual suffering from auditory hallucinations will hear a voice or voices saying the individual's own thoughts out loud, commenting on all their actions, or commanding and ordering the individual around. These voices tend to be negative and critical toward the individual. People who suffer from schizophrenia and have auditory hallucinations will often speak to the voice as though they are speaking to a second person.[48]
Visual
The most common modality referred to when people speak of hallucinations include the phenomena of seeing things that are not present or visual perception, which does not reconcile with the physical, consensus reality. There are many different causes that have been classed as psychophysiologic (a disturbance of brain structure), psychobiochemical (a disturbance of neurotransmitters), psychodynamic (an emergence of the unconscious into consciousness), and psychological (e.g., meaningful experiences consciousness); this is also the case in Alzheimer's disease. Numerous disorders can involve visual hallucinations, ranging from psychotic disorders to dementia to migraine, but experiencing visual hallucinations does not in itself mean that there is necessarily a disorder. Visual hallucinations are associated with organic disorders of the brain and with drug- and alcohol-related illness,[49] and not typically considered the result of a psychiatric disorder.[50]
Schizoc hallucination
Hallucinations may be caused by schizophrenia. Schizophrenia is a mental disorder in which there is an inability to tell the difference between real and unreal experiences, to think logically, to have contextually appropriate emotions, and to function in social situations.[51]
Neuroanatomical correlates
Normal everyday procedures like getting an MRI (Magnetic Resonance Imaging) have been used to find out more about auditory and verbal hallucinations. "Functional magnetic resonance imaging (fMRI) and repetitive transcranial magnetic stimulation (rTMS) were used to explore the pathophysiology of auditory/verbal hallucinations (AVHs)"[52] Throughout the exploring through MRI's of patients,there were "lower levels of hallucination-related activation in Broca’s area strongly predicted greater rate of response to left temporoparietal rTMS."[52]
Also through fMRIs, it is found that there can be better understandings on why hallucinations happen in the brain, by understanding emotions and cognition and how they can prompt physical reactions that can help result in a hallucination. It suggests the theory that "motivations in the body and mind can drive us to certain behaviors that we act in, such as survival instinct and intuition" and that they can work in a hand-in-hand-like fashion. It can also be viewed as a symbolic "homeostasis" that can have adverse effects by having these hallucinations and/or mental illnesses. The amygdala has also been seen to relate to this finding by contributing a "declarative judgement of emotional salience" as well as affecting both "efferent and afferent representational levels of affective autonomic responses in the brain".[53] Hallucinations in schizophrenia have been found to associate with differences in morphology of the paracingulate sulcus.[54]
Pathophysiological mechanisms
There are symptoms that are mechanism-based that are associated with hallucinations. These include superficial pressure and stabbing pain. Others include a burning-like sensation or electric shock feeling. Human studies of these symptoms remain mostly unclear unlike similar studies in animals.[55]
Treatments
There are few treatments for many types of hallucinations. However, for those hallucinations caused by mental disease, a psychologist or psychiatrist should be alerted, and treatment will be based on the observations of those doctors. Antipsychotic and atypical antipsychotic medication may also be utilized to treat the illness if the symptoms are severe and cause significant distress. For other causes of hallucinations there is no factual evidence to support any one treatment is scientifically tested and proven. However, abstaining from hallucinogenic drugs, managing stress levels, living healthily, and getting plenty of sleep can help reduce the prevalence of hallucinations. In all cases of hallucinations, medical attention should be sought out and informed of one's specific symptoms.
Epidemiology
One study from as early as 1895[56] reported that approximately 10% of the population experiences hallucinations. A 1996-1999 survey of over 13,000 people[57] reported a much higher figure, with almost 39% of people reporting hallucinatory experiences, 27% of which daytime hallucinations, mostly outside the context of illness or drug use. From this survey, olfactory (smell) and gustatory (taste) hallucinations seem the most common in the general population.
See also
- Phantosmia
- Closed-eye hallucination
- Dimethyltryptamine
- Folie à deux
- Ganzfeld effect
- Hallucinogenic fish
- Hallucinations in the sane
- Hypnagogia
- Microwave auditory effect
- Phantom eye syndrome
- Prisoner's cinema
- Psychedelic experience
- Psychotic depression
- Simulated reality
- Vision (spirituality)
- Lourdes apparitions
- Schizophrenia
- Bicameralism (psychology)
References
- ↑ Leo P. W. Chiu (1989). "Differential diagnosis and management of hallucinations" (PDF). Journal of the Hong Kong Medical Association. t 41 (3): 292–7.
- ↑ Chen E, Berrios GE (1996). "Recognition of hallucinations: a multidimensional model and methodology". Psychopathology. 29 (1): 54–63. doi:10.1159/000284972. PMID 8711076.
- ↑ Pelak, Victoria. "Approach to the patient with visual hallucinations". www.uptodate.com. Retrieved 2014-08-25.
- ↑ "Paracusia". thefreedictionary.com.
- ↑ Nolen-Hoeksema, Susan (2014). Abnormal Psychology (6e ed.). McGraw-Hill. p. 283.
- ↑ "Rescuers heard a voice" Ben Brumfield, CNN March 9, 2015
- ↑ "'Mysterious voice' led Utah Officers to child who survived for 14 hours in submerged car" Joel Landau , New York Daily News,March 9, 2015
- ↑ "Lily Groesbeck Rescue" NBC news
- ↑ "Rescuers recall 'distinct voice' that spurred them to rescue trapped toddler" Pat Reavy , KSL newsradio , March 8, 2015
- ↑ Shibayama M (2011). "Differential diagnosis between dissociative disorders and schizophrenia". Seishin shinkeigaku zasshi=Psychiatria et neurologia Japonica. 113 (9): 906–911. PMID 22117396.
- ↑ Thompson, Andrea (September 15, 2006). "Hearing Voices: Some People Like It". LiveScience.com. Retrieved 2006-11-25.
- ↑ Engmann, Birk; Reuter, Mike: "Spontaneous perception of melodies – hallucination or epilepsy?" Nervenheilkunde 2009 Apr 28: 217-221. ISSN 0722-1541
- ↑ Ozsarac M, Aksay E, Kiyan S, Unek O, Gulec FF (2012). "De novo cerebral arteriovenous malformation: Pink Floyd's song "Brick in the Wall" as a warning sign". J Emerg Med. 43 (1): e17–20. doi:10.1016/j.jemermed.2009.05.035. PMID 19682829.
- ↑ "Rare Hallucinations Make Music In The Mind". ScienceDaily.com. August 9, 2000. Retrieved 2006-12-31.
- ↑ Medical News Today: "Too Much Coffee Can Make You Hear Things That Are Not There"
- 1 2 Beck-Sander A, Birchwood M, Chadwick P (1997). "Acting on command hallucinations: A cognitive approach". The British journal of clinical psychology / the British Psychological Society. 36 (1): 139–48. doi:10.1111/j.2044-8260.1997.tb01237.x. PMID 9051285.
- ↑ Lee TM, Chong SA, Chan YH, Sathyadevan G (2004). "Command hallucinations among Asian patients with schizophrenia". Canadian Journal of Psychiatry. 49 (12): 838–42. PMID 15679207.
- ↑ Knoll, James L., Resnick, Phillip J. (2008). "Insanity Defense Evaluations: Toward a Model for Evidence-Based Practice". Brief Treatment and Crisis Intervention. 8 (1): 92–110. doi:10.1093/brief-treatment/mhm024.
- 1 2 Shea, Sean Christopher. "M.D".
- 1 2 3 4 5 HealthUnlocked (2014), "Phantosmia (Smelling Odours That Aren't There)", NHS Choices, retrieved 6 August 2016
- ↑ Hong, Seok-Chan; Holbrook, Eric H.; Leopold, Donald A.; Hummel, Thomas (2012), "Distorted Olfactory Perception: A Systematic Review", Acta Oto-Laryngologica (Supplement), 132 (S1): S27
- 1 2 Leopold, D. A. (2002), "Distortion of Olfactory Perception: Diagnosis and Treatment", Chemical Senses, 27 (7): 611–615
- 1 2 Berrios GE (April 1982). "Tactile hallucinations: conceptual and historical aspects". J. Neurol. Neurosurg. Psychiatr. 45 (4): 285–93. doi:10.1136/jnnp.45.4.285. PMC 491362
 . PMID 7042917.
. PMID 7042917. - 1 2 3 Panayiotopoulos CP (2007). A clinical guide to epileptic syndromes and their treatment (2nd ed.). London: Springer. ISBN 978-1846286438.
based on the ILAE classification and practice parameter guidelines
- 1 2 Barker P (1997). Assessment in psychiatric and mental health nursing: in search of the whole person. Cheltenham, UK: Stanley Thornes Publishers. p. 245. ISBN 978-0748731749.
- ↑ Ohayon MM, Priest RG, Caulet M, Guilleminault C (1996). "Hypnagogic and Hypnopompic Hallucinations: Pathological Phenomena?". The British Journal of Psychiatry. 169 (4): 459–67. doi:10.1192/bjp.169.4.459. PMID 8894197.
- 1 2 3 4 Manford M, Andermann F (Oct 1998). "Complex visual hallucinations. Clinical and neurobiological insights". Brain. 121 (Pt 10): 1819–40. doi:10.1093/brain/121.10.1819. PMID 9798740.
- ↑ Mark Derr (2006) "Marilyn and Me," The New York Times, February 14, 2006
- ↑ Engmann, Birk (2008). "Phosphenes and photopsias - ischaemic origin or sensorial deprivation? - Case history". Z Neuropsychol. (in German). 19 (1): 7–13. doi:10.1024/1016-264X.19.1.7.
- 1 2 3 Teeple RC, Caplan JP, Stern TA (2009). "Visual Hallucinations: Differential Diagnosis and Treatment". Primary Care Companion to the Journal of Clinical Psychiatry. 11 (1): 26–32. doi:10.4088/PCC.08r00673. PMC 2660156
 . PMID 19333408.
. PMID 19333408. - ↑ Bien CG, Benninger FO, Urbach H, Schramm J, Kurthen M, Elger CE (2000). "Localizing value of epileptic visual auras". Brain. 123 (2): 244–253. doi:10.1093/brain/123.2.244. PMID 10648433.
- ↑ Frood, Arran. "Drug Hallucinations Look Real in the Brain". New Scientist. Retrieved October 25, 2011.
- ↑ Gurney, E., Myers, F.W.H. and Podmore, F. (1886). Phantasms of the Living, Vols. I and II. London: Trubner and Co..
- ↑ Sidgwick, Eleanor; Johnson, Alice; and others (1894). Report on the Census of Hallucinations, London: Proceedings of the Society for Psychical Research, Vol. X.
- ↑ See Slade, P.D. and Bentall, R.P. (1988). Sensory Deception: a scientific analysis of hallucination. London: Croom Helm, for a review.
- ↑ Horowitz, M. (1975). Hallucinations: An information-processing approach. New York: Wiley. pp. 163–194.
- 1 2 Blom, Jan (2010). A Dictionary of Hallucinations. Springer. p. 459. ISBN 978-1-4419-1222-0. Retrieved July 11, 2012.
- ↑ Casey, Patricia; Brendan Kelly (2007). Fish's Clinical Psychopathology: Signs and Symptoms in Psychiatry. RCPsych Publications. p. 23. ISBN 1-904671-32-2. Retrieved July 11, 2012.
- ↑ Joseph M. Tonkonogy, Iosif Moiseevich Tonkonogiĭ, Antonio E. Puente (2009). Localization of Clinical Syndromes in Neuropsychology and Neuroscience. Springer. p. 200. ISBN 0826119670. Retrieved July 11, 2012.
- ↑ Erick Messias, ed. "Schizophrenia". Medopedia. Retrieved July 14, 2012.
- ↑ Smith Ely Jelliffi, ed. (1915). Journal of nervous and mental disease, Volume 42. New York. pp. 30–31. Retrieved July 11, 2012.
- ↑ Chakrabarty A, Reddy MS (2011). "Visual hallucinations in mania". Indian Journal of Psychological Medicine. 33 (1): 71–73. doi:10.4103/0253-7176.85399. PMC 3195159
 . PMID 22021957.
. PMID 22021957. - ↑ Urbán, Péter (2011). Brainstem Disorders. Springer. p. 173. ISBN 3642042023. Retrieved July 11, 2012.
- ↑ Kapur S (Jan 2003). "Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia". Am J Psychiatry. 160 (1): 13–23. doi:10.1176/appi.ajp.160.1.13. PMID 12505794.
- ↑ Bentall RP (Jan 1990). "The illusion of reality: a review and integration of psychological research on hallucinations". Psychol Bull. 107 (1): 82–95. doi:10.1037/0033-2909.107.1.82. PMID 2404293.
- ↑ Grossberg S (Jul 2000). "How hallucinations may arise from brain mechanisms of learning, attention, and volition". J Int Neuropsychol Soc. 6 (5): 583–92. doi:10.1017/S135561770065508X. PMID 10932478.
- 1 2 3 4 5 Horowitz MJ (1975). "Hallucinations: An Information Processing Approach". In West LJ, Siegel RK. Hallucinations; behavior, experience, and theory. New York: Wiley. ISBN 0-471-79096-6.
- ↑ Nolen-Hoeksema, Susan. Abnormal Psychology (6th ed.). Boston: McGraw-Hill. p. 223.
- ↑ Semple, David. Oxford Hand Book of Psychiatry. Oxford press. 2005.
- ↑ Teeple RC, Caplan JP, Stern TA (2009). "Visual hallucinations: differential diagnosis and treatment". Prim Care Companion J Clin Psychiatry. 11 (1): 26–32. doi:10.4088/PCC.08r00673. PMC 2660156
 . PMID 19333408.
. PMID 19333408. - ↑ Stannard, Lia. "Schizophrenia Types of Hallucinations." LiveStrong. Demand Media, Inc., 11 May 2011. Web. 14 Dec 2011.
- 1 2 Hoffman RE, Hampson M, Wu K, Anderson AW, Gore JC, Buchanan RJ, Constable RT, Hawkins KA, Sahay N, Krystal JH (2007). "Probing the pathophysiology of auditory/verbal hallucinations by combining functional magnetic resonance imaging and transcranial magnetic stimulation". Cereb. Cortex. 17 (11): 2733–43. doi:10.1093/cercor/bhl183. PMC 2634833
 . PMID 17298962.
. PMID 17298962. - ↑ Critchley HD (2009). "Psychophysiology of neural, cognitive and affective integration: fMRI and autonomic indicants". International Journal of Psychophysiology. 73 (2): 88–94. doi:10.1016/j.ijpsycho.2009.01.012. PMC 2722714
 . PMID 19414044.
. PMID 19414044. - ↑ Garrison, JR; Al., et. (2015). "Paracingulate sulcus morphology is associated with hallucinations in the human brain.". Nature Communications. 6: 8956. doi:10.1038/ncomms9956. PMC 4660352
 . PMID 26573408. Lay summary.
. PMID 26573408. Lay summary. hallucinations were associated with specific brain morphology differences in the paracingulate sulcus, a fold in the medial prefrontal cortex, with a 1 cm reduction in sulcal length increasing the likelihood of hallucinations by 19.9%, regardless of the sensory modality in which they were experienced. The findings suggest a specific morphological basis for a pervasive feature of typical and atypical human experience.
- ↑ Leone, Caterina; Biasiotta, Antonella. "Pathophysiological Mechanisms of Neuropathic Pain". Medscape. Retrieved 7 August 2014.
- ↑ Francis Nagaraya; Myers FWH; et al. (1894). "Report on the census of hallucinations". Proceedings of the Society for Psychical Research. 34: 25–394.
- ↑ Ohayon MM (Dec 2000). "Prevalence of hallucinations and their pathological associations in the general population". Psychiatry Res. 97 (2–3): 153–64. doi:10.1016/S0165-1781(00)00227-4. PMID 11166087.
Further reading
- Johnson FH (1978). The Anatomy of Hallucinations. Chicago: Nelson-Hall Co. ISBN 0-88229-155-6.
- Bentall RP, Slade PD (1988). Sensory Deception: A Scientific Analysis of Hallucination. London: Croom Helm. ISBN 0-7099-3961-2.
- Aleman A, Larøi F (2008). Hallucinations: The Science of Idiosyncratic Perception. American Psychological Association (APA). ISBN 1-4338-0311-9.
- Sacks O (2012). Hallucinations. New York: Alfred A. Knopf. ISBN 978-0307957245
External links
- Hearing Voices Network
- "Anthropology and Hallucinations; chapter from The Making of Religion". psychanalyse-paris.com. November 4, 2006. Retrieved October 4, 2016.
- "The voice inside: A practical guide to coping with hearing voices"
- Psychology Terms
- Hallucination: A Normal Phenomenon?
- Fasting-induced hallucination