Glipizide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Glucotrol |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a684060 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | A10BB07 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability |
100% (regular formulation) 90% (extended release) |
| Protein binding | 98 to 99% |
| Metabolism | Hepatic hydroxylation |
| Biological half-life | 2 to 5 hours |
| Excretion | Renal and fecal |
| Identifiers | |
| |
| CAS Number |
29094-61-9 |
| PubChem (CID) | 3478 |
| IUPHAR/BPS | 6821 |
| DrugBank |
DB01067 |
| ChemSpider |
3359 |
| UNII |
X7WDT95N5C |
| KEGG |
D00335 |
| ChEBI |
CHEBI:5384 |
| ChEMBL |
CHEMBL1073 |
| ECHA InfoCard | 100.044.919 |
| Chemical and physical data | |
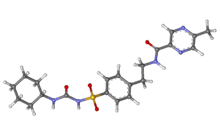
| Formula | C21H27N5O4S |
| Molar mass | 445.536 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Glipizide is an oral rapid- and short-acting anti-diabetic medication from the sulfonylurea class. It is classified as a second-generation sulfonylurea, which means that it undergoes enterohepatic circulation. Second-generation sulfonylureas are both more potent and have shorter half-lives than the first-generation sulfonylureas.
Originally available in 1984, it is marketed by Pfizer under the brand name Glucotrol in the USA, where Pfizer sells Glucotrol in doses of 5 and 10 milligrams and Glucotrol XL (an extended release form of glipizide) in doses of 2.5, 5, and 10 milligrams. Other companies also market glipizide, most commonly extended release tablets of 5 and 10 milligrams.
Mechanism of action
Glipizide acts by partially blocking potassium channels among beta cells of pancreatic islets of Langerhans. By blocking potassium channels, the cell depolarizes which results in the opening of voltage-gated calcium channels. The resulting calcium influx encourages insulin release from beta cells.
Sulfonylureas may also cause the decrease of serum glucagon and potentiate the action of insulin at the extrapancreatic tissues. The mouse model of MODY diabetes suggested that the reduced glipizide clearance stands behind their therapeutic success in human MODY patients, but Urbanova et al. found that human MODY patients respond differently to the mouse model and that there was no consistent decrease in glipizide clearance in randomly selected HNF1A-MODY and HNF4A-MODY patients.[1]
See also
References
- ↑ Urbanova, J.; et al. (2015). "Half-Life of Sulfonylureas in HNF1A and HNF4A Human MODY Patients is not Prolonged as Suggested by the Mouse Hnf1a-/- Model". Current Pharmaceutical Design. 21: 5736–5748. doi:10.2174/1381612821666151008124036.
External links
- Glucotrol XL Full U.S. Prescribing Information. Accessed on July 26, 2005.