Gingival recession
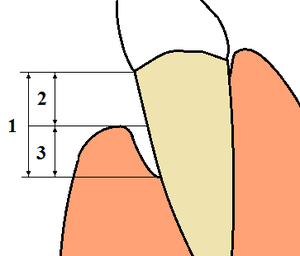
Gingival recession, also known as receding gums, is the exposure in the roots of the teeth caused by a loss of gum tissue and/or retraction of the gingival margin from the crown of the teeth.[1] Gum recession is a common problem in adults over the age of 40, but it may also occur starting from the age of a teenager, or around the age of 10. It may exist with or without concomitant decrease in crown-to-root ratio (recession of alveolar bone).
Classification
Various classifications have been proposed to classify gingival recession, Miller’s classification system[2] being the one that is most widely followed. Many cases which are encountered in daily clinical practice cannot be classified according to the criteria of the present classification systems. Kumar & Masamatti's classification system gives a comprehensive depiction of recession defect that can be used to include cases that cannot be classified according to present classifications. A separate classification system for palatal recessions (PR) has been given. A new comprehensive classification system classifies recession on the basis of the position of interdental papilla and buccal/lingual/palatal recessions. Kumar & Masamatti's classification system tries to overcome the limitations of Miller's classification.[3]
Causes
There are many possible causes for gingival recession:
- By far the most common cause is gum disease (periodontal disease).[1] Inadequate brushing and flossing allows bacteria to build up between the teeth and below the gumline, which leads to painless, chronic inflammation of the gums and gradual recession, with increased tooth mobility as the supporting bone is lost.
- Overaggressive brushing,[1] which causes the enamel at the gum line to be worn away over time by scrubbing the sides of the teeth in a washboard fashion
- Improper flossing (i.e., flossing too roughly or aggressively) which may cut into the gums
- Hereditary thin, fragile or insufficient gingival tissue predisposes to gingival recession.[1]
- Excessive clenching and grinding of the teeth (bruxism) can sometimes worsen pre-existing periodontal disease. By itself, bruxism may cause a reversible increase in tooth mobility, but not any gingival recession.
- stomach acid damage from self-induced vomiting, which may be associated with certain eating disorders
- Dipping tobacco, which affects the mucous membrane lining in the mouth and will cause receding gums over time
- Self-inflicted trauma, such as habits like digging a fingernail or pencil into the gum. This type of recession more commonly associated with children and persons with psychiatric disorders.
- Scurvy (lack of dietary vitamin C)
- Acute necrotizing ulcerative gingivitis
- Adult orthodontic movement of teeth.
- Abnormal tooth position, such as tooth crowding, giving inadequate cover of one or more teeth by the jaw bone.[1]
- Piercings in the lip or tongue that wear away the gum by rubbing against it.
- Intentional gingival retraction. For example, the adult tooth may not grow out of the gum, and to remedy this, a procedure called an exposure is done. It involves the gum tissue being cut open to allow the adult tooth to grow out. This is a less common cause of gum recession.
Symptoms
Gum recession is generally not an acute condition. In most cases, receding of gums is a progressive condition that occurs gradually over the years. This is one reason that it is common over the age of 40. Because the changes in the condition of the gums from one day to another are minimal, patients get used to the gums' appearance and tend not to notice the recession visually. Receding gums may remain unnoticed until the condition starts to cause symptoms.

The following signs and symptoms may indicate gum recession:
- Tooth mobility
- Dentin hypersensitivity (over-sensitive teeth) - short, sharp pain is triggered by hot, cold, sweet, sour, or spicy food and drink. If the cementum covering the root is not protected anymore by the gums, it is easily abraded exposing the dentin tubules to external stimuli.
- Teeth may also appear longer than normal (a larger part of the crown is visible if gums are receding)
- The roots of the tooth are exposed and visible
- The tooth feels notched at the gum line
- Change in the tooth’s color (due to the color difference between enamel and cementum)
- Spaces between teeth seem to grow (the space is the same, but it seems larger because the gums do not fill it any more)
- Cavities below the gum line
If the gum recession is caused by gingivitis, the following symptoms may also be present:
- Puffy, red, or swollen (inflamed) gums
- Gum bleeding while brushing or flossing
- Bad breath (halitosis)
In some cases, it is the treatment of gingivitis that reveals a gum recession problem, that was previously masked by the gums swelling.[4]
Treatment
Treatment should start with addressing the problem(s) that caused the gum recession. If overactive brushing is the cause, the patient should consider purchasing a softer toothbrush and use a more gentle brushing technique. If poor plaque control was a contributing factor, improved oral hygiene must be performed, combined with regular professional dental cleanings as prophylaxis. If severe calculus (tartar) was the cause, then a procedure called scaling and root planing may be necessary to clean the teeth and heal inflammation in the gingiva (gums). If malocclusion (incorrect bite) was a factor, an occlusal adjustment (bite adjustment) or bite splint may be recommended.
If cause-specific measures are insufficient, soft-tissue graft surgery may be used to create more gingiva.[1] The tissue used may be autologous tissue from another site in the patient's mouth, or it can be freeze-dried tissue products or synthetic membranes.[1] New research is focused on using stem cells to culture the patients' own gums to replace receded gums.
Gingival grafting
Depending on the shape of the gum recession and the levels of bone around the teeth, areas of gum recession can be regenerated with new gum tissue using a variety of gum grafting "periodontal plastic surgery" procedures performed by a specialist in periodontics (a periodontist). These procedures are typically completed under local anesthesia with or without conscious sedation, as the patient prefers. This may involve repositioning of adjacent gum tissue to cover the recession (called a pedicle graft) or use of a free graft of gingival or connective tissue from the roof of the mouth (called a free gingival graft or a Subepithelial connective tissue graft). Alternatively, a material called acellular dermal matrix (processed donated human skin allograft) may be used instead of tissue from the patient's own palate.
Growth-factor techniques
Recent advances have seen the introduction of platelet derived growth factor (PDGF) infused bone graft material. This material is usually combined with the cellular matrix to form a soft bone paste that is then covered by the allograft. The development of this type of bone and tissue cellular matrix (also known as ortho filler) results in greater osseointegration with the patient's healthy bone and soft tissue.
Healing from such procedures requires 2–4 weeks. After a few months the results can be evaluated and in some cases the new tissue needs to be reshaped in a very minor procedure to get an optimal result. In cases where recession is not accompanied by periodontal bone loss, complete or near complete coverage of the recession area is achievable.
References
- 1 2 3 4 5 6 7 Gingival Recession - Causes and treatment JADA, Vol 138. http://jada.ada.org. Oct 2007. American Dental Association
- ↑ Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent 1985;5:8-13.
- ↑ Kumar A, Masamatti SS. A new classification system for gingival and palatal recession. J Indian Soc Periodontol 2013;17:175-81.
- ↑ Receding Gums - Causes, Treatment & Prevention of Gum Recession
- AAP Periodontal Plastic Surgery Page
- American Academy of Periodontology (AAP)
- The Gum Recession Project
External links
- An academic presentation on gingival recession
- Highly informative overview article from the NYTimes.