Immune tolerance in pregnancy
Immune tolerance in pregnancy or gestational/maternal immune tolerance is the absence of a maternal immune response against (in other words, immune tolerance towards) the fetus and placenta during pregnancy,[1] which thus may be viewed as unusually successful allografts, since they genetically differ from the mother.[2] In the same way, many cases of spontaneous abortion may be described in the same way as maternal transplant rejection.[2] It is studied within the field of reproductive immunology.
Mechanisms
Placental mechanisms
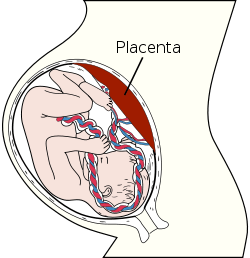
The placenta functions as an immunological barrier between the mother and the fetus, creating an immunologically privileged site. For this purpose, it uses several mechanisms:
- It secretes Neurokinin B containing phosphocholine molecules. This is the same mechanism used by parasitic nematodes to avoid detection by the immune system of their host.[3]
- Also, there is presence of small lymphocytic suppressor cells in the fetus that inhibit maternal cytotoxic T cells by inhibiting the response to interleukin 2.[2]
- The placental trophoblast cells do not express the classical MHC class I isotypes HLA-A and HLA-B, unlike most other cells in the body, and this absence is assumed to prevent destruction by maternal cytotoxic T cells, which otherwise would recognize the fetal HLA-A and HLA-B molecules as foreign. On the other hand, they do express the atypical MHC class I isotypes HLA-E and HLA-G, which is assumed to prevent destruction by maternal NK cells, which otherwise destroy cells that do not express any MHC class I.[4] However, trophoblast cells do express the rather typical HLA-C.[4]
- It forms a syncytium without any extracellular spaces between cells in order to limit the exchange of migratory immune cells between the developing embryo and the body of the mother (something an epithelium will not do sufficiently, as certain blood cells are specialized to be able to insert themselves between adjacent epithelial cells). The fusion of the cells is apparently caused by viral fusion proteins from endosymbiotic endogenous retrovirus (ERV).[5] An immunoevasive action was the initial normal behavior of the viral protein, in order to avail for the virus to spread to other cells by simply merging them with the infected one. It is believed that the ancestors of modern viviparous mammals evolved after an infection by this virus, enabling the fetus to better resist the immune system of the mother.[6]
Still, the placenta does allow maternal IgG antibodies to pass to the fetus to protect it against infections. However, these antibodies do not target fetal cells, unless any fetal material has escaped across the placenta where it can come in contact with maternal B cells and make those B cells start to produce antibodies against fetal targets. The mother does produce antibodies against foreign ABO blood types, where the fetal blood cells are possible targets, but these preformed antibodies are usually of the IgM type,[7] and therefore usually do not cross the placenta. Still, rarely, ABO incompatibility can give rise to IgG antibodies that cross the placenta, and are caused by sensitization of mothers (usually of blood type 0) to antigens in foods or bacteria.[8]
Other mechanisms
Still, the placental barrier is not the sole means to evade the immune system, as foreign fetal cells also persist in the maternal circulation, on the other side of the placental barrier.[9]
The placenta does not block maternal IgG antibodies, which thereby may pass through the human placenta, providing immune protection to the fetus against infectious diseases.
One model for the induction of tolerance during the very early stages of pregnancy is the Eutherian Fetoembryonic Defense System (eu-FEDS) hypothesis.[10] The basic premise of the eu-FEDS hypothesis is that both soluble and cell surface associated glycoproteins, present in the reproductive system and expressed on gametes, suppress any potential immune responses, and inhibit rejection of the fetus.[10] The eu-FEDS model further suggests that specific carbohydrate sequences (oligosaccharides) are covalently linked to these immunosuppressive glycoproteins and act as “functional groups” that suppress the immune response. The major uterine and fetal glycoproteins that are associated with the eu-FEDS model in the human include alpha-fetoprotein, CA125, and glycodelin-A (also known as placental protein 14 (PP14)).
Regulatory T cells also likely play a role.[11]
Also, a shift from cell-mediated immunity toward humoral immunity is believed to occur.[12]
Insufficient tolerance
Many cases of spontaneous abortion may be described in the same way as maternal transplant rejection,[2] and a chronic insufficient tolerance may cause infertility. Other examples of insufficient immune tolerance in pregnancy are Rh disease and pre-eclampsia:
- Rh disease is caused by the mother producing antibodies (including IgG antibodies) against the Rhesus D antigen on her baby's red blood cells. It occurs if the mother is Rh negative and the baby is Rh positive, and a small amount of Rh positive blood from any previous pregnancy has entered the mother's circulation to make her produce IgG antibodies against the D antigen (Anti-D). Maternal IgG is able to pass through the placenta into the fetus and if the level of it is sufficient, it will cause destruction of D positive fetal red blood cells leading to development of the anti-Rh type of hemolytic disease of the fetus and newborn (HDFN). Generally HDFN becomes worse with each additional Rh incompatible pregnancy.
- One cause of pre-eclampsia is an abnormal immune response towards the placenta. There is substantial evidence for exposure to partner's semen as prevention for pre-eclampsia, largely due to the absorption of several immune modulating factors present in seminal fluid.[13][14]
Pregnancies resulting from egg donation, where the carrier is less genetically similar to the fetus than a biological mother, are associated with a higher incidence of pregnancy-induced hypertension and placental pathology.[15] The local and systemic immunologic changes are also more pronounced than in normal pregnancies, so it has been suggested that the higher frequency of some conditions in egg donation may be caused by reduced immune tolerance from the mother.[15]
Infertility and miscarriage
Immunological responses could be the cause in many cases of infertility and miscarriage. Some immunological reasons that contribute to infertility are reproductive autoimmune failure syndrome, the presence of anti-phospholipid antibodies, and antinuclear antibodies.
Anti-phospholipid antibodies are targeted toward the phospholipids of the cell membrane. Studies have shown that antibodies against phosphatidylserine, phoshphatidylcholine, phosphatidylglycerol, phosphatidylinositol and phosphatidylethanolamine target the pre-embryo. Antibodies against phosphatidylserine and phosphatidylethanolamine are against the trophoblast.[16] These phospholipids are essential in the aiding the cells of the fetus to remain attached to the cells of the uterus with implantation. If a female has antibodies against these phospholipids, they will be destroyed through the immune response and ultimately the fetus will not be able to remain bound to the uterus. These antibodies also jeopardize the health of the uterus by altering the blood flow to the uterus.[16]
Antinuclear antibodies cause an inflammation in the uterus that does not allow it to be a suitable host for implantation of the embryo. Natural killer cells misinterpret the fetal cells as cancer cells and attack them. An individual that presents with reproductive autoimmune failure syndrome has unexplained infertility, endometriosis, and repetitive miscarriages due to elevated levels of antinuclear antibodies circulating.[16] Both the presence of anti-phospholipids antibodies and antinuclear antibodies have toxic effects on the implantation of embryos. This does not apply to anti-thyroid antibodies. Elevated levels do not have a toxic effect, but they are indicative of a risk of miscarriage. Elevated anti-thyroid antibodies act as a marker for females who have T-lymphocyte dysfunction because these levels indicate T cells that are secreting high levels of cytokines that induce inflammation in the uterine wall.[16]
Still, there is currently no drug that has evidence of preventing miscarriage by inhibition of maternal immune responses; aspirin has no effect in this case.[17]
Increased infectious susceptibility
The increased immune tolerance is believed to be a major contributing factor to an increased susceptibility and severity of infections in pregnancy.[18] Pregnant women are more severely affected by, for example, influenza, hepatitis E, herpes simplex and malaria.[18] The evidence is more limited for coccidioidomycosis, measles, smallpox, and varicella.[18] However, pregnancy does not seem to alter the protective effects vaccination.[18]
Interspecific pregnancy
If the mechanisms of rejection-immunity of the fetus could be elucidated, it could avail for interspecific pregnancy, having, for example pigs carry human fetuses to term as an alternative to a human surrogate mother.[19]
References
- ↑ Williams, Zev (Sep 20, 2012). "Inducing Tolerance to Pregnancy". New England Journal of Medicine. 367: 1159–1161. doi:10.1056/NEJMcibr1207279. PMC 3644969
 . PMID 22992082.
. PMID 22992082. - 1 2 3 4 Clark DA, Chaput A, Tutton D (March 1986). "Active suppression of host-vs-graft reaction in pregnant mice. VII. Spontaneous abortion of allogeneic CBA/J x DBA/2 fetuses in the uterus of CBA/J mice correlates with deficient non-T suppressor cell activity". J. Immunol. 136 (5): 1668–75. PMID 2936806.
- ↑ "Placenta 'fools body's defences'". BBC News. 2007-11-10.
- 1 2 Page 31 to 32 in: Maternal-Fetal Medicine : Principles and Practice. Editor: Robert K. Creasy, Robert Resnik, Jay D. Iams. ISBN 978-0-7216-0004-8 Published: September 2003
- ↑ Mi S, Lee X, Li X, et al. (Feb 2000). "Syncytin is a captive retroviral envelope protein involved in human placental morphogenesis". Nature. 403 (6771): 785–9. doi:10.1038/35001608. PMID 10693809.
- ↑ Luis P. Villarreal (Sep 2004). "Can Viruses Make Us Human?" (PDF). Proceedings of the American Philosophical Society. 148 (3): 314.
- ↑ Magnetic immunodiagnostic method for the demonstration of antibody/antigen complexes especially of blood groups Yves Barbreau, Olivier Boulet, Arnaud Boulet, Alexis Delanoe, Laurence Fauconnier, Fabien Herbert, Jean-Marc Pelosin, Laurent Soufflet. October 2009
- ↑ Merck manuals > Perinatal Anemia Last full review/revision January 2010 by David A. Paul
- ↑ Williams Z, Zepf D, Longtine J, et al. (March 2008). "Foreign fetal cells persist in the maternal circulation". Fertil. Steril. 91 (6): 2593–5. doi:10.1016/j.fertnstert.2008.02.008. PMID 18384774.
- 1 2 Clark GF, Dell A, Morris HR, Patankar MS, Easton RL (2001). "The species recognition system: a new corollary for the human fetoembryonic defense system hypothesis". Cells Tissues Organs (Print). 168 (1-2): 113–21. doi:10.1159/000016812. PMID 11114593.
- ↑ Trowsdale J, Betz AG (March 2006). "Mother's little helpers: mechanisms of maternal-fetal tolerance". Nat. Immunol. 7 (3): 241–6. doi:10.1038/ni1317. PMID 16482172.
- ↑ Jamieson DJ, Theiler RN, Rasmussen SA. Emerging infections and pregnancy. Emerg Infect Dis. 2006 Nov. Available from http://www.cdc.gov/ncidod/EID/vol12no11/06-0152.htm
- ↑ Sarah Robertson. "Research Goals --> Role of seminal fluid signalling in the female reproductive tract".
- ↑ Sarah A. Robertson; John J. Bromfield; Kelton P. Tremellen (2003). "Seminal 'priming' for protection from pre-eclampsia—a unifying hypothesis". Journal of Reproductive Immunology. 59 (2): 253–265. doi:10.1016/S0165-0378(03)00052-4. PMID 12896827.
- 1 2 Van Der Hoorn, M. L. P.; Lashley, E. E. L. O.; Bianchi, D. W.; Claas, F. H. J.; Schonkeren, C. M. C.; Scherjon, S. A. (2010). "Clinical and immunologic aspects of egg donation pregnancies: a systematic review". Human Reproduction Update. 16 (6): 704–12. doi:10.1093/humupd/dmq017. PMID 20543201.
- 1 2 3 4 Gronowski, Ann M (2004), Handbook of Clinical Laboratory Testing During Pregnancy, Humana Press, ISBN 1-58829-270-3
- ↑ Kaandorp, S. P.; Goddijn, M. T.; Van Der Post, J. A. M.; Hutten, B. A.; Verhoeve, H. R.; Hamulyák, K.; Mol, B. W.; Folkeringa, N.; Nahuis, M.; Papatsonis, D. N. M.; Büller, H. R.; Van Der Veen, F.; Middeldorp, S. (2010). "Aspirin plus Heparin or Aspirin Alone in Women with Recurrent Miscarriage". New England Journal of Medicine. 362 (17): 1586–1596. doi:10.1056/NEJMoa1000641. PMID 20335572.
- 1 2 3 4 Kourtis, Athena P.; Read, Jennifer S.; Jamieson, Denise J. (2014). "Pregnancy and Infection". New England Journal of Medicine. 370 (23): 2211–2218. doi:10.1056/NEJMra1213566. ISSN 0028-4793.
- ↑ Darwin's children LeVay, Simon. (1997, October 14). from The Free Library. (1997). Retrieved March 06, 2009