Gastritis
| Gastritis | |
|---|---|
 | |
| Micrograph showing gastritis. H&E stain. | |
| Classification and external resources | |
| Specialty | Gastroenterology |
| ICD-10 | K29.0-K29.7 |
| ICD-9-CM | 535.0-535.5 |
| DiseasesDB | 34500 |
| MedlinePlus | 001150 |
| eMedicine | emerg/820 med/852 |
| MeSH | D005756 |
Gastritis is inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain.[1] Other possible symptoms include nausea and vomiting, bloating, loss of appetite and heartburn.[1][2] Complications may include bleeding, stomach ulcers, and stomach tumors.[1] When due to autoimmune problems, low red blood cells due to not enough vitamin B12 may occur, a condition known as pernicious anemia.[3]
Common causes include infection with Helicobacter pylori and use of NSAIDs. Less common causes include alcohol, smoking, cocaine, severe illness, autoimmune problems, radiation therapy and Crohn's disease, among others.[1][4] Endoscopy, a type of X-ray known as an upper gastrointestinal series, blood tests, and stool tests may help with diagnosis.[1] The symptoms of gastritis may be a presentation of a myocardial infarction. Other conditions with similar symptoms include inflammation of the pancreas, gallbladder problems, and peptic ulcer disease.[2]
Prevention is by avoiding things that cause the disease.[5] Treatment includes medications such as antacids, H2 blockers, or proton pump inhibitors.[1] During an acute attack drinking viscous lidocaine may help.[6] If gastritis is due to NSAIDs these may be stopped. If H. pylori is present it may be treated with a combination of antibiotics such as amoxicillin and clarithromycin.[1] For those with pernicious anemia, vitamin B12 supplements are recommended either by mouth or by injection.[3] People are usually advised to avoid foods that bother them.[7]
Gastritis is believed to affect about half of people worldwide.[5] In 2013 there were approximately 90 million new cases of the condition.[8] As people get older the disease becomes more common.[5] It, along with a similar condition in the first part of the intestines known as duodenitis, resulted in 60,000 deaths in 2013.[9] H. pylori was first discovered in 1981 by Barry Marshall and Robin Warren.[10]
Signs and symptoms
Many people with gastritis experience no symptoms at all. However, upper central abdominal pain is the most common symptom; the pain may be dull, vague, burning, aching, gnawing, sore, or sharp.[11] Pain is usually located in the upper central portion of the abdomen,[12] but it may occur anywhere from the upper left portion of the abdomen around to the back.
Other signs and symptoms may include the following:
- Nausea
- Vomiting (if present, may be clear, green or yellow, blood-streaked, or completely bloody, depending on the severity of the stomach inflammation)
- Belching (if present, usually does not relieve the pain much)
- Bloating
- Early satiety[11]
- Loss of appetite
- Unexplained weight loss
Cause
Common causes include Helicobacter pylori and NSAIDs. Less common causes include alcohol, cocaine, severe illness and Crohn disease, among others.[1]
Helicobacter pylori
Helicobacter pylori colonizes the stomachs of more than half of the world's population, and the infection continues to play a key role in the pathogenesis of a number of gastroduodenal diseases. Colonization of the gastric mucosa with Helicobacter pylori results in the development of chronic gastritis in infected individuals, and in a subset of patients chronic gastritis progresses to complications (e.g., ulcer disease, gastric neoplasias, some distinct extragastric disorders).[13] However, over 80 percent of individuals infected with the bacterium are asymptomatic and it has been postulated that it may play an important role in the natural stomach ecology.[14]
Critical illness
Gastritis may also develop after major surgery or traumatic injury ("Cushing ulcer"), burns ("Curling ulcer"), or severe infections. Gastritis may also occur in those who have had weight loss surgery resulting in the banding or reconstruction of the digestive tract.
Diet
Evidence does not support a role for specific foods including spicy foods and coffee in the development of peptic ulcers.[15] People are usually advised to avoid foods that bother them.[7]
Pathophysiology
Acute
Acute erosive gastritis typically involves discrete foci of surface necrosis due to damage to mucosal defenses.[16] NSAIDs inhibit cyclooxygenase-1, or COX-1, an enzyme responsible for the biosynthesis of eicosanoids in the stomach, which increases the possibility of peptic ulcers forming.[17] Also, NSAIDs, such as aspirin, reduce a substance that protects the stomach called prostaglandin. These drugs used in a short period are not typically dangerous. However, regular use can lead to gastritis.[18] Additionally, severe physiologic stress ("stress ulcers") from sepsis, hypoxia, trauma, or surgery, is also a common etiology for acute erosive gastritis. This form of gastritis can occur in more than 5% of hospitalized patients.
Also, note that alcohol consumption does not cause chronic gastritis. It does, however, erode the mucosal lining of the stomach; low doses of alcohol stimulate hydrochloric acid secretion. High doses of alcohol do not stimulate secretion of acid.[19]
Chronic
Chronic gastritis refers to a wide range of problems of the gastric tissues.[16] The immune system makes proteins and antibodies that fight infections in the body to maintain a homeostatic condition. In some disorders the body targets the stomach as if it were a foreign protein or pathogen; it makes antibodies against, severely damages, and may even destroy the stomach or its lining.[18] In some cases bile, normally used to aid digestion in the small intestine, will enter through the pyloric valve of the stomach if it has been removed during surgery or does not work properly, also leading to gastritis. Gastritis may also be caused by other medical conditions, including HIV/AIDS, Crohn's disease, certain connective tissue disorders, and liver or kidney failure. Since 1992, chronic gastritis lesions are classified according to the Sydney system.[20]
Metaplasia
Mucous gland metaplasia, the reversible replacement of differentiated cells, occurs in the setting of severe damage of the gastric glands, which then waste away (atrophic gastritis) and are progressively replaced by mucous glands. Gastric ulcers may develop; it is unclear if they are the causes or the consequences. Intestinal metaplasia typically begins in response to chronic mucosal injury in the antrum, and may extend to the body. Gastric mucosa cells change to resemble intestinal mucosa and may even assume absorptive characteristics. Intestinal metaplasia is classified histologically as complete or incomplete. With complete metaplasia, gastric mucosa is completely transformed into small-bowel mucosa, both histologically and functionally, with the ability to absorb nutrients and secrete peptides. In incomplete metaplasia, the epithelium assumes a histologic appearance closer to that of the large intestine and frequently exhibits dysplasia.[16]
Diagnosis
Often, a diagnosis can be made based on the patient's description of their symptoms, but other methods which may be used to verify gastritis include:
- Blood tests:
- Blood cell count
- Presence of H. pylori
- Liver, kidney, gallbladder, or pancreas functions
- Urinalysis
- Stool sample, to look for blood in the stool
- X-rays
- ECGs
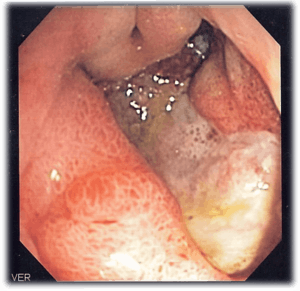
- Endoscopy, to check for stomach lining inflammation and mucous erosion
- Stomach biopsy, to test for gastritis and other conditions[21]
Treatment
Antacids are a common treatment for mild gastritis.[22] When antacids do not provide enough relief, medications such as H2 blockers and proton-pump inhibitors that help reduce the amount of acid are often prescribed.[22][23]
Cytoprotective agents are designed to help protect the tissues that line the stomach and small intestine. They include the medications sucralfate and misoprostol. If NSAIDs are being taken regularly, one of these medications to protect the stomach may also be taken. Another cytoprotective agent is bismuth subsalicylate.
Several regimens are used to treat H. pylori infection. Most use a combination of two antibiotics and a proton pump inhibitor. Sometimes bismuth is also added to the regimen.
See also
References
- 1 2 3 4 5 6 7 8 "Gastritis". The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). November 27, 2013. Retrieved 1 March 2015.
- 1 2 Rosen & Barkin's 5-Minute Emergency Medicine Consult (4 ed.). Lippincott Williams & Wilkins. 2012. p. 447. ISBN 9781451160970.
- 1 2 Varbanova, M.; Frauenschläger, K.; Malfertheiner, P. (Dec 2014). "Chronic gastritis - an update.". Best Pract Res Clin Gastroenterol. 28 (6): 1031–42. doi:10.1016/j.bpg.2014.10.005. PMID 25439069.
- ↑ Stephen Hauser (2014). Mayo Clinic Gastroenterology and Hepatology Board Review. Oxford University Press. p. 49. ISBN 9780199373338.
- 1 2 3 Fred F. Ferri (2012). Ferri's Clinical Advisor 2013,5 Books in 1, Expert Consult - Online and Print,1: Ferri's Clinical Advisor 2013. Elsevier Health Sciences. p. 417. ISBN 9780323083737.
- ↑ James G. Adams (2012). "32". Emergency Medicine: Clinical Essentials. Elsevier Health Sciences. ISBN 9781455733941.
- 1 2 Holdsworth, [edited by] Joan Gandy, Angela Madden, Michelle (2012). Oxford handbook of nutrition and dietetics (2nd ed.). Oxford: Oxford University Press, USA. p. 571. ISBN 9780199585823.
- ↑ Global Burden of Disease Study 2013, Collaborators (22 August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet (London, England). 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMID 26063472.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet. 385: 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604
 . PMID 25530442.
. PMID 25530442. - ↑ Wang, AY; Peura, DA (October 2011). "The prevalence and incidence of Helicobacter pylori-associated peptic ulcer disease and upper gastrointestinal bleeding throughout the world.". Gastrointestinal endoscopy clinics of North America. 21 (4): 613–35. doi:10.1016/j.giec.2011.07.011. PMID 21944414.
- 1 2 "Gastritis Symptoms". eMedicineHealth. 2008. Retrieved 2008-11-18.
- ↑ "Gastritis". National Digestive Diseases Information Clearinghouse. National Institute of Diabetes and Digestive and Kidney Diseases. December 2004. Retrieved 2008-10-06.
- ↑ Kandulski A, Selgrad M, Malfertheiner P (August 2008). "Helicobacter pylori infection: a clinical overview". Digestive and Liver Disease. 40 (8): 619–26. doi:10.1016/j.dld.2008.02.026. PMID 18396114.
- ↑ Blaser, M. J. (2006). "Who are we? Indigenous microbes and the ecology of human diseases" (PDF). EMBO Reports. 7 (10): 956–60. doi:10.1038/sj.embor.7400812. PMC 1618379
 . PMID 17016449.
. PMID 17016449. - ↑ Pennsylvania, editors, Raphael Rubin, M.D., Professor of Pathology, David S. Strayer, M.D., Ph. D., Professor of Pathology, Department of Pathology and Cell Biology, Jefferson Medical College of Thomas Jefferson University Philadelphia, Pennsylvania ; Founder and Consulting Editor, Emanuel Rubin, M.D., Gonzalo Aponte Distinguished Professor of Pathology, Chairman Emeritus of the Department of Pathology and Cell Biology, Jefferson Medical College of Thomas Jefferson University, Philadelphia, (2012). Rubin's pathology : clinicopathologic foundations of medicine (Sixth ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 623. ISBN 9781605479682.
- 1 2 3 "Gastritis". Merck. January 2007. Retrieved 2009-01-11.
- ↑ Dajani EZ, Islam K (August 2008). "Cardiovascular and gastrointestinal toxicity of selective cyclo-oxygenase-2 inhibitors in man" (PDF). J Physiol Pharmacol. 59 Suppl 2: 117–33. PMID 18812633.
- 1 2 Siegelbaum, Jackson (2006). "Gastritis". Jackson Siegelbaum Gastroenterology. Retrieved 2008-11-18.
- ↑ Wolff G (1989). "[Effect of alcohol on the stomach]" [Effect of alcohol on the stomach]. Gastroenterol J (in German). 49 (2): 45–9. PMID 2679657.
- ↑ Mayo Clinic Staff (April 13, 2007). "Gastritis". MayoClinic. Retrieved 2008-11-18.
- ↑ "Exams and Tests". eMedicinHealth. 2008. Retrieved 2008-11-18.
- 1 2 Zajac, P; Holbrook, A; Super, ME; Vogt, M (March–April 2013). "An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia". Osteopathic Family Physician. 5 (2): 79–85. doi:10.1016/j.osfp.2012.10.005.
- ↑ Boparai V, Rajagopalan J, Triadafilopoulos G (2008). "Guide to the use of proton pump inhibitors in adult patients". Drugs. 68 (7): 925–47. doi:10.2165/00003495-200868070-00004. PMID 18457460.