Fundus photography
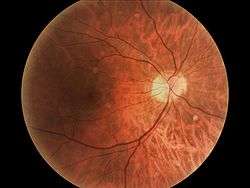
Fundus photography involves capturing a photograph of the back of the eye i.e. fundus. Specialized fundus cameras that consist of an intricate microscope attached to a flashed enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.[1]
| Fundus photography | |
|---|---|
| Intervention | |
| ICD-9-CM | 95.11 |
The models and technology of fundus photography has advanced and evolved rapidly over the last century.[2] Since the equipments are sophisticated and challenging to manufacture to clinical standards, only a few manufacturers/brands are available in the market: Volk, Topcon, Zeiss, Canon, Nidek, Kowa, CSO and CenterVue are some example of fundus camera manufacturers.[3]

History
The concept of fundus photography was first introduced in the mid-1800s, after the introduction of photography in 1839. The goal of photographing the human ocular fundus was slowly but surely becoming more achievable. In 1851, Hermann von Helmholtz introduced the Ophthalmoscope, and James Clerk Maxwell presented a colour photography method in 1861.
In the early 1860s, Henry Noyes and Abner Mulholland Rosebrugh both assembled fundus cameras and tried fundus photography on animals. Although the news was encouraging and showed promise, the vision of capturing a satisfactory photo of a human ocular fundus was still far from reach. Early fundus photos were limited by insufficient light, long exposures, eye movement, and prominent corneal reflexes that reduced the clarity detail. It would be several decades before these problems could be rectified.
There has been some controversy regarding the first ever successful human fundus photo. Most accounts state William Thomas Jackman and J.D. Webster since they published their technique along with a reproduction of a fundus image in two photography periodicals in 1886.
Three other names played a prominent role in early fundus photography. According to some historical accounts, Elmer Starr and Lucien Howe may have been first to photograph the human retina. Lucien Howe is a well-known name in Ophthalmology, and together with his assistant Elmer Starr, they collaborated on the fundus photography project in 1886-88. Howe described their results as the first "recognizable” fundus photograph, apparently a nod to Jackman & Webster being the first to "publish” a fundus photograph. Based on the written accounts, Howe and Starr's image was more "recognizable” as a fundus.[4]
For about 75 years a concerted effort was made to clearly photograph the fundus. Hundreds of specialists worked to overcome the problem, which was finally achieved in the early 20th century by Friedrich Dimmer, who published his photographs in 1921. Dimmer’s fundus camera, developed about 1904, was a complicated and sophisticated research tool and it was not until 1926 that Stockholm’s Johan Nordenson and the Zeiss Camera Company were able to market a commercial device for use by practitioners, which was the first modern Fundus camera.[5]
Since then, the features of fundus cameras have improved drastically to include nonmydriatic imaging, electronic illumination control, automated eye alignment, and high-resolution digital image capture. These improvements have helped make modern fundus photography a standard ophthalmic practice for documenting retinal disease.[6]
Following the development of fundus photography, David Alvis, and Harold Novotny, performed the first fluorescein angiography (FFA) in 1959, using the Zeiss fundus camera with electronic flash. This development was huge feat in the world of Ophthalmology.[7]
Fundus camera

Optical principles
The optical design of fundus cameras is based on the principle of monocular indirect ophthalmoscopy.[8][9] A fundus camera provides an upright, magnified view of the fundus. A typical camera views 30 to 50° of retinal area, with a magnification of 2.5x, and allows some modification of this relationship through zoom or auxiliary lenses from 15°, which provides 5x magnification, to 140° with a wide angle lens, which minifies the image by half.[9] The optics of a fundus camera are similar to those of an indirect ophthalmoscope in that the observation and illumination systems follow dissimilar paths.

The observation light is focused via a series of lenses through a doughnut shaped aperture, which then passes through a central aperture to form an annulus, before passing through the camera objective lens and through the cornea onto the retina.[10] The light reflected from the retina passes through the un-illuminated hole in the doughnut formed by the illumination system. As the light paths of the two systems are independent, there are minimal reflections of the light source captured in the formed image. The image forming rays continue towards the low powered telescopic eyepiece. When the button is pressed to take a picture, a mirror interrupts the path of the illumination system allow the light from the flash bulb to pass into the eye. Simultaneously, a mirror falls in front of the observation telescope, which redirects the light onto the capturing medium, whether it is film or a digital CCD. Because of the eye’s tendency to accommodate while looking though a telescope, it is imperative that the exiting vergence is parallel in order for an in focus image to be formed on the capturing medium.
Modes
Practical instruments for fundus photography perform the following modes of examination:
- Colour, where the retina is illuminated by white light and examined in full colour.
- Red free fundus photography utilises a filter in order to better observe superficial lesions and some vascular abnormalities within the retina and surrounding tissue. A green filter ~540-570 nm is used to block out red wavelengths of light. This allows a better contrast for viewing retinal blood vessels and associated haemorrhages, pale lesions such as drusen and exudates, and subtle characteristics such as nerve fibre layer defects and epiretinal membranes.[11] This is considered to provide a superior method of observing IRMA, NVE, and NVD than colour photography in Diabetic retinopathy progression assessment. Red free photography is also regularly used as a base line photo prior to Angiography.[12]
- Angiography is a process of photographing/recording vascular flow within the retina and surrounding tissue by injecting a fluorescent dye into the blood stream. This dye fluoresces a different colour when light from a specific wavelength (excitation colour) reaches it. Barrier filters then only allow the autoflourescent wavelengths of light to be photographed. Using this method a sequence of photographs can be produced that show the movement, and pooling of blood over time (“Phases”) as the dye passes though the retina and choroid.[13]
- Sodium Fluorescein Angiography (abbreviated FFA, FA or FAG) is used for the imaging of retinal vascular disease and utilises blue excitation light of ~490 nm and fluoresces a yellow light of ~530 nm. It is routinely used to image Cystoid Macular Oedema and Diabetic Retinopathy among others.[13]
- Indocyanine Green Angiography (abbreviated ICG) is used primarily for imaging deeper choroidal diseases and utilises near-infrared diode laser of 805 nm and barrier filters allow light of 500 and 810 nm to be photographed. ICG is useful for seeing choroidal vessel outpouching in cases of idiopathic polypoidal choroidal vasculopathy, abnormal vessels supplying ocular tumors, hyperpermeable vessels leading to central serous chorioretinopathy among other conditions.[14]
- Simultaneous stereo fundus photos have been published prior to 1909 however their use as a diagnostic tool is not widespread.[15] Recent advances in digital photography and 3D monitors has seen some manufacturers incorporating it once again into photographic equipment.[16][17] The current process involves simultaneously photographing the retina from two slightly different angles. These two images are later used together to create a 3D image. In this way the image can be analysed giving better information about surface characteristics of the retina.[18]
- Fundus photography in animals: Fundus photography is a useful tool utilised for veterinary research, veterinary ophthalmology, as well as education.[19] Numerous studies have used it as a research method for the study of ocular and systemic conditions in animals.[20]
Resolve artifact in fundus photography
Artifact errors in fundus images are captured through the improper setting up and alignment of the patient, examiner and the fundus camera. Patient cooperation and attitude are crucial to minimise artifacts. The clinician must ensure that the patient has understood the instruction. They must also correctly align, set the camera controls and make decisions concerning film choice. Each of these factors must be taken into consideration when evaluating a fundus photograph.[21] However some artifacts are not visible until the film is captured and normally this can be cause either from a mechanical problem in the camera, patient's pupil size or blink.[22]
The picture on the left represents patient that has blinked when the fundus photo was taken, resulting in a blurred and incomplete image of the fundus. It is imperative to instruct the patient not to blink when the fundus photo is taken.The patient may blink normally at any other time to prevent the excessive drying of the eye. A dry eye may also lead to a blurred fundus photo. When dry eye is suspected, ask the patient to blink several times to lubricate the eye before continuing.
The picture on the right depicts an incorrectly taken fundus photo that is out of focus and somewhat obscured. The examiner taking the fundus photo has to be extremely careful and meticulous in ensuring correct alignment, and that the picture of the fundus is in clear focus before capturing the image. Make sure the 3 white dots are in clear focus and aligned with the pupil before pressing the alignment button. If the fundus is out of focus, move the joystick backward and forward to focus the image appropriately. Once the image is in clear focus the alignment process can be completed and lastly the photo taken.
Indications
Optometrists, Ophthalmologists, Orthoptists and other trained medical professionals use fundus photography for monitoring the progression of certain eye condition/diseases. Fundus photographs are also used to document abnormalities of disease process affecting the eye, and/or to follow up on the progress of the eye condition/disease such as diabetes, age-macular degeneration(AMD), glaucoma, Neoplasm of the choroid, cranial nerves, retinal or eyeball, etc.
In patients with diabetes mellitus, regular fundus screening examinations (once every 6 months to 1 year) are important to screen for diabetic retinopathy as visual loss due to diabetes can be prevented by retinal laser treatment if retinopathy is spotted early.
Besides the prevalent ocular condition/diseases, fundus photography can also be used to monitor individuals on anti-malarial therapy, by noting the changes in the fundus during standard screening.
Fundus photography is also used in emergency cases including patients with constant headaches, diastolic pressure greater than or equal to 120mmHg and patients with sudden visual loss.
In patients with headaches, the finding of swollen optic discs, or papilloedema, on fundus photography is a key sign, as this indicates raised intracranial pressure (ICP) which could be due to hydrocephalus, benign intracranial hypertension (aka pseudotumour cerebri) or brain tumor, amongst other conditions. Cupped optic discs are seen in glaucoma.
In arterial hypertension, hypertensive changes of the retina closely mimic those in the brain, and may predict cerebrovascular accidents (strokes).
In certain cases fundus photography can also be used in research studies.[23]
Recording and interpretation
Fundus photographs are ocular documentation that record the appearance of a patient's retina. The photographs allow the clinician to study a patient's retina, detect retinal changes and review a patient's retinal findings with a coworker. Fundus photographs are routinely called upon in a wide variety of ophthalmic conditions.[1]
Fundus photography is used to inspect anomalies associated to diseases that affect the eye and to monitor the progression of the disease. It is vital for disease processes such as macular degeneration, retinal neoplasms, choroid disturbances and diabetic retinopathy. Additionally it aids in identifying glaucoma, multiple sclerosis, and other central nervous system abnormalities. It evaluates irregularities in the fundus, monitors the progression of a disease, management and therapeutic outcome. They are crucial to create a starting point to better understand a disease's progression. Fundus photographs may be useful if there is a new disease affecting the fundus and for the planning of additional management options. The medical necessity of fundus photography and other diagnostic imaging must be recorded in an orderly fashion so that the clinician is able to compare photographs of a patient from different timelines.
Documents of a patient's medical record must consist of a recent, relevant history, progress notes and fundus photographs depicting and supporting the relevant diagnosis. The photographs need to be labelled appropriately such as which eye, the date, and patient details. The patient’s records ought to contain documented outcomes of the fundus photography as well as a depiction of variations from previous photographs. They should contain an interpretation of those results and the relevant changes it could have on treatment plan. Fundus photographs without an interpretation are seen as obsolete. The records should be legible, and contain suitable patient information and clinician details.
The interpretation of fundus photographs that are glaucomatous must contain a description of the vertical and horizontal cup to disc ratio, vessel pattern, diffuse or focal pallor, asymmetry and development of the above factors. The retinal nerve fibre layer should also be studied and commented on.[24]
It is also a useful tool in objectively measuring torsion as well as in documenting and recording progression of diseases over time. Fundus photography does not replace binocular indirect ophthalmoscopy; it is a tool to supplement and complement existing findings and to maintain a record of disease progression. Fundus photography is mainly used to monitor the progression of a retinal or optic nerve head disorder. It is also good for providing photo documentation for the continuum of care and to monitor the patient's ocular condition.
Advantages and disadvantages
The retina consists of ten semi-transparent layers that serve specific functions in the process of visual perception. Fundus photography provides a bird’s-eye view of the top most layer, the inner limiting membrane, as well as the other underlying layers. As retinal abnormalities often begin in a particular layer of the retina before encroaching into the other layers (such as the formation of cotton wool spots in the nerve fiber layer), it is important to be able to appreciate depth when examining a fundus in order to provide an accurate diagnosis. However, despite recent advancements in technology and the development of stereo fundus cameras, which are able to provide three dimensional images by superimposing two images,[25] most fundus cameras in circulation are only able to provide two dimensional images of the fundus. This limitation currently prevents the technology from superseding the current gold standard which is indirect binocular ophthalmoscopy.
The following are some of the advantages and disadvantages of fundus photography:[2][26]
|
|
Future advancements
Fundus photography has been crucial in diagnosing and treating patients in Ophthalmology (especially retinal conditions such as Macular Degeneration and Diabetic Retinopathy) since the 1920s. Fluorescein angiography has been crucial to Ophthalmology since the late 1950s. While OCT imaging has helped reduce the need for fundus photography and fluorescein angiography, nothing has been implemented that can replace these very important diagnostic tests. 1. Computer-aided animation and analysis of time series retinal images have been suggested to observer retinal conditions. The manufacturer of the MatchedFlicker,[27] whose technology automatically aligns and registers two images of the same retina taken at different points in time thus generating a superimposed view which identifies any changes present between the two images. MatchedFlicker assists to improve both the speed and accuracy of image diagnostic evaluations, resulting in more effective workflow, more precise diagnosis and simplicity of recording. Studies have compared computer-aided animation and analysis of time series retinal images with photographic images in a number of retinal diseases such as glaucoma, diabetic retinopathy, age related macular degeneration and early screening of premature infant eyes for retinopathy. With results conclusively suggesting that computer aided animation provides a more accurate and earlier diagnosis including detection of glaucoma and screening of premature infant eyes for retinopathy.[24]
D-Eye
D-Eye works on the principles of direct ophthalmoscopy and exploits the smartphone camera's autofocus capability to account for a patient's refractive error. A front negative lens is imprinted in a glass plate, which serves as the top cover nearest the eye. This lens shifts the focus of the smartphone from infinity to −8 cm. This allows for a compensation of refractive error from −12 to +6 diopters. The final prototype measures approximately 47 × 18 × 10 mm and weighs 7 grams. Briefly, the light emitted by the “flash” of the camera is conveyed into the eye by a mirror and a beam splitter acts as a direct ophthalmoscope. The diaphragm, the polarizing filters, and the photo-absorbing wall remove reflections and flares. D-Eye is designed to work with Galaxy S4 and Galaxy S5 and iPhone 5, iPhone 5s, and iPhone 6.[28]
See also
- Dilated fundus examination
- Optical coherence tomography, commonly used for imaging the structure of the retina
Gallery
 A close-up of the controls of a Topcon retinal camera
A close-up of the controls of a Topcon retinal camera
External links
- Ophthalmic Photographers' Society
- "Fundus photography as a convenient tool to study microvascular response and cardiovascular risk factors"
- "An objective focusing method for fundus photography."
References
- 1 2 "Fundus Photography Overview - Ophthalmic Photographers' Society". www.opsweb.org. Retrieved 2015-09-17.
- 1 2 Abràmoff, Michael D.; Garvin, Mona K.; Sonka, Milan (2010-01-01). "Retinal Imaging and Image Analysis". IEEE transactions on medical imaging. 3: 169–208. doi:10.1109/RBME.2010.2084567. ISSN 0278-0062. PMC 3131209
 . PMID 21743764.
. PMID 21743764. - ↑ Panwar, Nishtha; Huang, Philemon; Lee, Jiaying; Keane, Pearse A.; Chuan, Tjin Swee; Richhariya, Ashutosh; Teoh, Stephen; Lim, Tock Han; Agrawal, Rupesh (2015-08-26). "Fundus Photography in the 21st Century-A Review of Recent Technological Advances and Their Implications for Worldwide Healthcare". Telemedicine Journal and e-Health: 150826121255008. doi:10.1089/tmj.2015.0068. ISSN 1556-3669. PMID 26308281.
- ↑ "Milestones, Rivalries and Controversy, Part III - Ophthalmic Photographers' Society". www.opsweb.org. Retrieved 2015-09-18.
- ↑ "Museum of Vision: Exhibitions". www.museumofvision.org. Retrieved 2015-09-18.
- ↑ Tran, Kenneth; Mendel, Thomas A.; Holbrook, Kristina L.; Yates, Paul A. (2012-11-01). "Construction of an Inexpensive, Hand-Held Fundus Camera through Modification of a Consumer "Point-and-Shoot" Camera". Investigative Ophthalmology & Visual Science. 53 (12): 7600–7607. doi:10.1167/iovs.12-10449. ISSN 0146-0404. PMC 3495602
 . PMID 23049089.
. PMID 23049089. - ↑ "Fluorescein angiography: Insight and serendipity a half century ago". Archives of Ophthalmology. 129 (7): 943–948. 2011-07-01. doi:10.1001/archophthalmol.2011.160. ISSN 0003-9950.
- ↑ Cassin, B. and Solomon, S. Dictionary of Eye Terminology. Gainesville, Florida: Triad Publishing Company, 1990.
- 1 2 Saine PJ. "Fundus Photography: What is a Fundus Camera?" Ophthalmic Photographers' Society. Accessed September 30, 2006.
- ↑ Saine PJ. "Fundus Photography: Fundus Camera Optics." Ophthalmic Photographers' Society. Accessed September 30, 2006.
- ↑ Ng, E; et al. (2014). Ophthalmological Imaging and Applications. CRC Press. ISBN 978-1-4665-5915-8.
- ↑ Venkatesh, Pradeep; Sharma, Reetika; Vashist, Nagender; Vohra, Rajpal; Garg, Satpal (2012-09-08). "Detection of retinal lesions in diabetic retinopathy: comparative evaluation of 7-field digital color photography versus red-free photography". International Ophthalmology. 35 (5): 635–640. doi:10.1007/s10792-012-9620-7. ISSN 0165-5701.
- 1 2 Ng, E (2014). Ophthalmological Imaging and Applications. CRC Press. ISBN 978-1-4665-5915-8.
- ↑ "Indocyanine Green Angiography". www.aao.org. Retrieved 2015-09-18.
- ↑ "Historical Review of Stereoscopic Imaging". www.cybersight.org. Retrieved 2015-09-18.
- ↑ "nonmyd WX - Fundus Camera | KOWA Technology for Life Science". www.kowa.co.jp. Retrieved 2015-09-18.
- ↑ "Simultaneous stereo fundus camera Patent (Patent # 5,120,122 issued June 9, 1992) - Justia Patents Database". patents.justia.com. Retrieved 2015-09-18.
- ↑ "Fundus Photography Overview - Ophthalmic Photographers' Society". www.opsweb.org. Retrieved 2015-09-18.
- ↑ Barnett, K. C.; Keeler, C. R. (1968-02-01). "Retinal photography in animals.". British Journal of Ophthalmology. 52 (2): 200–201. doi:10.1136/bjo.52.2.200. ISSN 1468-2079. PMID 5642675.
- ↑ Rosolen, S. G.; et al. (2011). "Veterinary ophthalmology; new veterinary ophthalmology findings from S.G. rosolen and co-authors described". Veterinary Research Week. Retrieved 16 August 2015.
- ↑ "Ophthalmic Photography: Retinal Photography, Angiography, an... : Optometry & Vision Science". Retrieved 2015-09-20.
- ↑ Landon S (1989). "Artifacts in fundus photographs.". J Ophthalmic Nurs Technol. 8: 229–35. PMID 2625702.
- ↑ De Boever, Patrick; Louwies, Tijs; Provost, Eline; Int Panis, Luc; Nawrot, Tim S. (2014-01-01). "Fundus photography as a convenient tool to study microvascular responses to cardiovascular disease risk factors in epidemiological studies". Journal of Visualized Experiments (92): e51904. doi:10.3791/51904. ISSN 1940-087X. PMC 4353376
 . PMID 25407823.
. PMID 25407823. - 1 2 "Fundus Photography". www.aetna.com. Retrieved 2015-09-17.
- ↑ Tyler, Marshall E. (1996). "Stereo Fundus Photography" (PDF). Journal of Ophthalmic Photography. Retrieved 18 August 2015.
- ↑ "Why non-mydriatic cameras will not replace dilated fundus exams". OptometryTimes. Retrieved 2015-09-20.
- ↑ "Accurate Eye Image Analysis with MatchedFlicker". www.eyeic.com. Retrieved 2015-09-17.
- ↑ Russo, Andrea; Morescalchi, Francesco; Costagliola, Ciro; Delcassi, Luisa; Semeraro, Francesco (2015-01-01). "A Novel Device to Exploit the Smartphone Camera for Fundus Photography". Journal of Ophthalmology. 2015: 1–5. doi:10.1155/2015/823139. ISSN 2090-004X. PMC 4468345
 . PMID 26137320.
. PMID 26137320.