Follicular lymphoma
| Follicular lymphoma | |
|---|---|
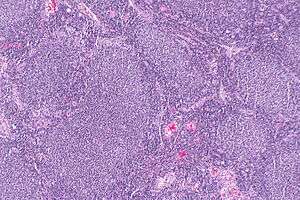 | |
| Micrograph of a follicular lymphoma, showing the characteristically abnormal lymphoid follicles that gave the condition its name. H&E stain. | |
| Classification and external resources | |
| Specialty | Hematology and oncology |
| ICD-10 | C82 |
| ICD-9-CM | 202.0 |
| ICD-O | M9690/3 |
| OMIM | 151430 |
| eMedicine | med/1362 |
| MeSH | D008224 |
Follicular lymphoma is a type of blood cancer. It is the most common of the indolent (slow-growing) non-Hodgkin's lymphomas, and the second-most-common form of non-Hodgkin's lymphomas overall. It is defined as a lymphoma of follicle center B-cells (centrocytes and centroblasts), which has at least a partially follicular pattern. It is positive for the B-cell markers CD10, CD19, CD22, and usually CD20,[1] but almost always negative for CD5.[2]
There are several synonymous and obsolete terms for this disease, such as CB/CC lymphoma (Centroblastic and Centrocytic lymphoma), nodular lymphoma[3] and Brill-Symmers Disease.
Morphology

The tumor is composed of follicles containing a mixture of centrocytes (Kiel nomenclature adopted by WHO experts) or cleaved follicle center cells (older American nomenclature), "small cells", and centroblasts (Kiel nomenclature adopted by WHO experts) or large noncleaved follicle center cells (older American nomenclature), "large cells". These follicles are surrounded by non-malignant cells, mostly T-cells. In the follicles, centrocytes typically predominate; centroblasts are usually in minority. Peripheral smear will also reveal buttock cells.[4]
Grading

According to the WHO criteria, the disease is morphologically graded into:[5]
- grade 1 (<5 centroblasts per high-power field (hpf))
- grade 2 (6–15 centroblasts/hpf)
- grade 3 (>15 centroblasts/hpf).
Grade 3 is further subdivided into:
- grade 3A (centrocytes still present)
- grade 3B (the follicles consist almost entirely of centroblasts)
The WHO 2008 update classifies grades 1 and 2 now as low grade follicular lymphoma, grade 3A as high grade follicular lymphoma, and grade 3B as Diffuse Large B Cell Lymphoma (DLBCL).
Causes
A translocation between chromosome 14 and 18 results in the overexpression of the bcl-2 gene.[6] As the bcl-2 protein is normally involved in preventing apoptosis, cells with an overexpression of this protein are basically immortal. The bcl-2 gene is normally found on chromosome 18, and the translocation moves the gene near to the site of the immunoglobulin heavy chain enhancer element on chromosome 14.
Translocations of BCL6 at 3q27 can also be involved.[7]
Treatment
There is no consensus regarding the best treatment protocol. Several considerations should be taken into account including age, stage, and prognostic scores (see International Prognostic Index). Patients with advanced disease who are asymptomatic might benefit from a watch and wait approach, as early treatment does not provide survival benefit.[8][9] When patients are symptomatic, specific treatment is required, which might include various combinations of alkylators, nucleoside analogues, anthracycline-containing chemotherapy regimens (e.g., CHOP), monoclonal antibodies (e.g. rituximab), radioimmunotherapy, autologous (self) and allogeneic (donor) hematopoietic stem cell transplantation. Follicular lymphoma is regarded as incurable, unless the disease is localized, in which case it can be cured by local irradiation. Although allogeneic stem cell transplantation may be curative, the mortality from the procedure is too high to be a first line option.
In 2010 rituximab was approved by the European Commission for first-line maintenance treatment of follicular lymphoma.[10] Pre-clinical evidence suggests that rituximab could be also used in combination with integrin inhibitors to overcome the resistance to rituximab mediated by stromal cells .[11] However, follicular lymphoma which is CD20 negative will not benefit from Rituximab, which targets CD20.
Trial results released in June 2012 show that bendamustine, a drug first developed in East Germany in the 1960s, more than doubled disease progression-free survival when given along with rituximab. This combination therapy also left patients with fewer side effects than the older treatment (a combination of five drugs—rituximab, cyclophosphamide (Cytoxan), doxorubicin (Adriamycin), vincristine and prednisone, collectively called R-CHOP).[12]
There are many recent and current clinical trials for follicular lymphoma.[13] For example, personalised idiotype vaccines have shown promise, particularly as upfront therapy,[14] but have still to prove their efficacy in randomized clinical trials.[15]
Prognosis
Median survival is around 10 years, but the range is wide, from less than one year, to more than 20 years. Some patients may never need treatment. The overall survival rate at five years is 72-77%.[16] Recent advances and addition of Rituximab, improved median survival. Recent reports for the period 1986 and 2012 estimates median survival of over 20 years
[17]
microRNA expression
In 2014, it was described that short non-coding RNAs named microRNAs (miRNAs) have important functions in lymphoma biology, including follicular lymphoma. In malignant B cells, miRNAs participate in pathways fundamental to the cells' development, such as receptor signalling, migration/adhesion, cell-cell interactions in immune niches, and the production and class-switching of immunoglobulins.[18] MiRNAs influence B cell maturation, generation of pre-, marginal zone, follicular, B1, plasma and memory B cells.[18]
Epidemiology
Of all cancers involving the same class of blood cell (lymphoproliferative disorders), 22% of cases are follicular lymphomas.[19]
See also
References
- ↑ Overview at UMDNJ
- ↑ Barekman CL, Aguilera NS, Abbondanzo SL (July 2001). "Low-grade B-cell lymphoma with coexpression of both CD5 and CD10. A report of 3 cases". Arch. Pathol. Lab. Med. 125 (7): 951–3. doi:10.1043/0003-9985(2001)125<0951:LGBCLW>2.0.CO;2. PMID 11419985.
- ↑ "follicular lymphoma" at Dorland's Medical Dictionary
- ↑ Spitalnik, Steven L.; Arinsburg, Suzanne; Jhang, Jeffrey (22 September 2014). Clinical Pathology Board Review. Elsevier Health Sciences. p. 310. ISBN 9780323186551.
It is important to be able to recognize buttock cells and to know that they represent cleaved centrocytic cells of follicular lymphoma.
- ↑ "Follicular Lymphomas". Retrieved 2008-07-26.
- ↑ Bosga-Bouwer AG, van Imhoff GW, Boonstra R, et al. (February 2003). "Follicular lymphoma grade 3B includes 3 cytogenetically defined subgroups with primary t(14;18), 3q27, or other translocations: t(14;18) and 3q27 are mutually exclusive". Blood. 101 (3): 1149–54. doi:10.1182/blood.V101.3.1149. PMID 12529293.
- ↑ Bosga-Bouwer AG, Haralambieva E, Booman M, et al. (November 2005). "BCL6 alternative translocation breakpoint cluster region associated with follicular lymphoma grade 3B". Genes Chromosomes Cancer. 44 (3): 301–4. doi:10.1002/gcc.20246. PMID 16075463.
- ↑ Follicular Lymphoma: Perspective, Treatment Options, and Strategy by T. Andrew Lister, MD, FRCP, http://www.medscape.org/viewarticle/709528_transcript
- ↑ Watchful Waiting in Low–Tumor Burden Follicular Lymphoma in the Rituximab Era: Results of an F2-Study Database http://jco.ascopubs.org/content/30/31/3848.abstract?sid=40023c4f-fb96-484b-a302-1ade09cc741e
- ↑ "Roche Gets EC Nod for Follicular Lymphoma Maintenance Therapy". October 29, 2010.
- ↑ Mraz, M.; Zent, C. S.; Church, A. K.; Jelinek, D. F.; Wu, X.; Pospisilova, S.; Ansell, S. M.; Novak, A. J.; Kay, N. E.; Witzig, T. E.; Nowakowski, G. S. (2011). "Bone marrow stromal cells protect lymphoma B-cells from rituximab-induced apoptosis and targeting integrin α-4-β-1 (VLA-4) with natalizumab can overcome this resistance". British Journal of Haematology. 155 (1): 53–64. doi:10.1111/j.1365-2141.2011.08794.x. PMID 21749361.
- ↑ "'Rediscovered' Lymphoma Drug Helps Double Survival: Study". June 3, 2012.
- ↑ http://clinicaltrials.gov/ct2/results?term=follicular+lymphoma
- ↑ Navarrete, MA; Heining-Mikesch, K; Schüler, F; Bertinetti-Lapatki, C; Ihorst, G; Keppler-Hafkemeyer, A; Dölken, G; Veelken, H (3 February 2011). "Upfront immunization with autologous recombinant idiotype Fab fragment without prior cytoreduction in indolent B-cell lymphoma.". Blood. 117 (5): 1483–91. doi:10.1182/blood-2010-06-292342. PMID 21045197.
- ↑ Inoges S, de Cerio AL, Soria E, Villanueva H, Pastor F, Bendandi M (January 2010). "Idiotype vaccines for human B-cell malignancies". Curr. Pharm. Des. 16 (3): 300–7. doi:10.2174/138161210790170111. PMID 20109139.
- ↑ Lymphoma, Follicular at eMedicine
- ↑ http://www.ejcancer.com/article/S0959-8049%2816%2931778-6/abstract
- 1 2 Musilova, K; Mraz, M (2014). "MicroRNAs in B cell lymphomas: How a complex biology gets more complex". Leukemia. doi:10.1038/leu.2014.351. PMID 25541152.
- ↑ Turgeon, Mary Louise (2005). Clinical hematology: theory and procedures. Hagerstown, MD: Lippincott Williams & Wilkins. p. 283. ISBN 0-7817-5007-5.
Frequency of lymphoid neoplasms. (Source: Modified from WHO Blue Book on Tumour of Hematopoietic and Lymphoid Tissues. 2001, p. 2001.)
External links
- Online Resource Community for Follicular Lymphoma.
- Resource page for follicular lymphoma