Fallopian tube cancer
| Fallopian tube cancer | |
|---|---|
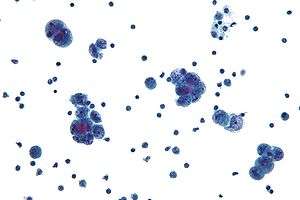 | |
| Micrograph of serous carcinoma, a type of cancer that arises in the uterine tube. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | C57.0, D28.2 |
| ICD-9-CM | 183.2, 221.0 |
| MeSH | D005185 |
Primary fallopian tube cancer (PFTC), often just tubal cancer, is a malignant neoplasm that originates from the fallopian tube.
Frequency
Tubal cancer is thought to be a relatively rare primary cancer among women accounting for 1 to 2 percent of all gynecologic cancers,[1] In the USA tubal cancer had an incidence of 0.41 per 100,000 women from 1998 to 2003.[2] Demographic distribution is similar to ovarian cancer, and the highest incidence was found in white, non-Hispanic women and women aged 60–79.[2] However, recent evidence suggests tubal cancer to be much more frequent .[3]
Evidence is accumulating that individuals with mutations of BRCA1 and BRCA2 are at higher risks for the development of PFTC.[4][5]
Pathology
The most common cancer type is the adenocarcinoma; in the largest series of 3,051 cases as reported by Stewart et al. 88% of cases fell into this category.[2] According to them half of the cases were poorly differentiated, 89% unilateral, and the distribution showed a third each with local, regional, and distant extensions. Rarer forms of tubal neoplasm include the leiomyosarcoma, and the transitional cell carcinoma.
As the tumor is often enmeshed with the adjacent ovary it may be the pathologist and not the surgeon who will determine that the lesion is indeed tubal in origin.
Secondary tubal cancer usually originates from cancer of the ovaries, the endometrium, the GI tract, the peritoneum, and the breast.
Symptoms
The internal location of the fallopian tubes makes it difficult to reach an early diagnosis. Symptoms are nonspecific and may consist of pain and vaginal discharge or bleeding. A pelvic mass may be detected on a routine gynecologic examination.
Vaginal discharge in fallopian tube carcinoma result from intermittent hydrosalphinx that is called as hydrops tubae profluens.[6]
Diagnosis
A pelvic examination may detect an adnexal mass. A CA-125 blood test is a nonspecific test that tends to be elevated in patients with tubal cancer. More specific tests are a gynecologic ultrasound examination, a CT scan, or an MRI of the pelvis. Occasionally, an early fallopian tube cancer may be detected serendipitously during pelvic surgery.
Treatment
The initial approach to tubal cancer is generally surgical and similar to that of ovarian cancer. As the lesion will spread first to the adjacent uterus and ovary, a total abdominal hysterectomy is an essential part of this approach and removes the ovaries, the tubes, and the uterus with the cervix. Also, peritoneal washings are taken, the omentum is removed, and pelvic and paraaortic lymph nodes are sampled. Staging at the time of surgery and pathological findings will determine further steps. In advanced cases when the cancer has spread to other organs and cannot be completely removed cytoreductive surgery is used to lessen the tumor burden for subsequent treatments. Surgical treatments are typically followed by adjuvant usually platinum-based chemotherapy.[7][8] Also radiation therapy has been applied with some success to patients with tubal cancer for palliative or curative indications[9]
Staging
International Federation of Gynecology and Obstetrics (FIGO) staging is done at the time of surgery:
- Stage 0 :Carcinoma in situ
- Stage I :Growth limited to fallopian tubes
- Stage II :Growth involving one or both fallopian tubes with extension to pelvis
- Stage III:Tumor involving one or both fallopian tubes with spread outside pelvis
- Stage IV :Growth involving one or more fallopian tubes with distant metastases
Prognosis
Prognosis depends to a large degree on the stage of the condition. In 1991 it was reported that about half of the patients with advanced stage disease survived 5 years with a surgical approach followed by cisplatinum-based chemotherapy.[10]
References
- ↑ UCSF. "Gynecologic Cancer: Fallopian Tube Cancer". accessed 08-14-2008
- 1 2 3 Stewart SL, Wike JM, Foster SL, Michaud F (2007). "The incidence of primary fallopian tube cancer in the United States.". Gynecol Oncol. 107 (3): 392–7. doi:10.1016/j.ygyno.2007.09.018. PMID 17961642.
- ↑ Piek JM, van Diest PJ, Verheijen RH (2008). "Ovarian carcinogenesis: an alternative hypothesis". Adv. Exp. Med. Biol. 622: 79–87. doi:10.1007/978-0-387-68969-2_7. PMID 18546620.
- ↑ BRCA mutations link to tubal cancer, accessed 08-14-2008
- ↑ http://dare.ubvu.vu.nl/handle/1871/9013
- ↑ GOLDMAN JA, GANS B, ECKERLING B (November 1961). "Hydrops tubae profluens--symptom in tubal carcinoma". Obstet Gynecol. 18: 631–4. PMID 13899814.
- ↑ Liapis A, Bakalianou K, Mpotsa E, Salakos N, Fotiou S, Kondi-Paffiti A (2008). "Fallopian tube malignancies: A retrospective clinical pathological study of 17 cases.". J Obstet Gynaecol. 28 (1): 93–5. doi:10.1080/01443610701811894. PMID 18259909.
- ↑ Takeshima N, Hasumi K (2000). "Treatment of fallopian tube cancer. Review of the literature.". Arch Gynecol Obstet. 264 (1): 13–9. doi:10.1007/pl00007475. PMID 10985612.
- ↑ Schray MF, Podratz KC, Malkasian GD (1987). "Fallopian tube cancer: the role of radiation therapy.". Radiother Oncol. 10 (4): 267–75. doi:10.1016/s0167-8140(87)80032-4. PMID 3444903.
- ↑ Barakat RR, Rubin SC, Saigo PE, et al. "Cisplatin-based combination chemotherapy in carcinoma of the fallopian tube.". Gynecol Oncol.