Dysautonomia
| Dysautonomia | |
|---|---|
|
The autonomic nervous system | |
| Classification and external resources | |
| Specialty | Neurology |
| ICD-10 | G90 |
| ICD-9-CM | 337.9 |
| MeSH | D001342 |
Dysautonomia is a term for a group of diseases that include postural orthostatic tachycardia syndrome (POTS), multiple system atrophy, autonomic failure, and autonomic neuropathy. In these conditions the autonomic nervous system (ANS) does not work properly. Dysautonomia is most often a type of neuropathy affecting the nerves that carry information from the brain and spinal cord to the heart, bladder, intestines, sweat glands, pupils, and blood vessels; although it has many causes, not all of which classify as neuropathic.[1]
The diagnosis is achieved through functional testing of the autonomic nervous system, focusing on the organ system affected. Investigations may be performed to identify underlying disease processes that may have led to the development of symptoms or autonomic neuropathy. Symptomatic treatment is available for many symptoms associated with dysautonomia, and some disease processes can be treated directly. [2]
Signs and symptoms
The symptoms of dysautonomia are numerous and vary widely for each individual,symptoms of dysautonomia are due to inefficient or unbalanced efferent signals sent via both systems.[3] The primary symptoms present in individuals with dysautonomia include:
- Orthostatic hypotension[4]
- Weakness[5]
- Low Blood Pressure[5]
- Bradycardia[5]
- Rapid heart rate[1]
- Anxiety[5]
- Insomnia[5]
- Chronic Fatigue[5]
- Tunnel vision[5]
- Exercise Intolerance[4]
- Brain Fog[4]
- Difficulty swallowing[6]
- Bowel incontinence[4]
- Blurry or double vision[4]
- Urinary incontinence or urinary retention[4]
- Constipation[5]
- Anhydrosis[4]
- Vertigo[5]
- Dizziness[5]
- Syncope[5]
Causes

Dysautonomia may be due to inherited or degenerative neurologic diseases (primary dysautonomia)[1] or it may occur due to injury of the autonomic nervous system from an acquired disorder (secondary dysautonomia).[4][7] The most common causes of dysautonomia include:
- Toxic causes (vincristine)[5]
- Parkinson disease[6]
- Diabetes[6]
- Multiple sclerosis[6]
- Guillain Barre syndrome[6]
- HIV and AIDS[6]
- Eaton-Lambert syndrome[5]
- Autoimmune disease, such as Sjögren's syndrome or SLE
- Amyloidosis[5]
- Chronic alcohol misuse[6]
- Lyme disease or coinfections, such as ehrlichiosis or babesiosis[5]
- Spinal cord injury[6]
- Surgery or injury involving the nerves[6]
- Ehlers-Danlos Syndrome[8]
- Paraneoplastic syndrome[9]
In the sympathetic nervous system predominant dysautonomia is common along with fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis, raising the possibility that such dysautonomia could be their common clustering underlying pathogenesis.[10]
Mechanism
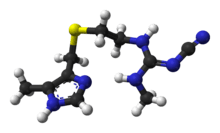
The autonomic nervous system (ANS) is a component of the peripheral nervous system and is made up of two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS controls the more active responses such as increasing heart rate and blood pressure. The PNS slows down the heart rate and aids in digestion,for example. Symptoms typically arise from abnormal responses of either the sympathetic or parasympathetic systems based on situation or environment.[1][11]
Diagnosis
The diagnosis of dysautonomia depends on the overall function of three autonomic functions - cardiovagal, adrenergic, and sudomotor. A diagnosis should, at a bare minimum, include measurements of blood pressure and heart rate while lying flat, and after at least 3 minutes of standing. The best way to achieve a diagnosis includes a range of testing, notably an autonomic reflex screen, tilt table test, and testing of the sudomotor response (QSART or thermoregulatory sweat test). [12] Additional tests and exams to determine a diagnosis of dysautonomia include the following:
- Cold presser[12]
- Testing for orthostatic intolerance[12]
- Hyperventilation test[12]
- Deep breathing[12]
- Valsalva maneuver[12]
- Tilt table test[12]
- Ambulatory blood pressure and EKG monitoring [5]
- Quantitative sudomotor axon reflex test (QSART)[12]
- Thermoregulatory sweat test[12]
- Nerve biopsy for Small fiber neuropathy[4]
Tests to elucidate the cause of dysautonomia can include:
Management
The treatment of dysautonomia can be difficult, since it is made up of many different symptoms, a combination of drug therapies is often required to manage individual symptomatic complaints. Therefore, if an autoimmune neuropathy is the case, then treatment with immunomodulatory therapies is done, or if diabetes mellitus is the cause, control of blood glucose is important.[4] In treatment there can be: proton-pump inhibitors and H2 receptor antagonists used for digestive symptoms such as acid reflux.[13]
For the treatment of genitourinary autonomic neuropathy medications may include sildenafil (a guanine monophosphate type-5 phosphodiesterase inhibitor). For the treatment of hyperhidrosis, anticholinergic agents such as trihexyphenidyl or scopolamine can be used, also intracutaneous injection of botulinum toxin type A can be used for management in some cases.[14]
Prognosis
The prognosis of dysautonomia depends on several factors, individuals with chronic, progressive, generalized dysautonomia in the setting of central nervous system degeneration such as Parkinson's disease or multiple system atrophy have a generally poorer long-term prognosis. Consequently, dysautonomia could be fatal due to pneumonia, acute respiratory failure, or sudden cardiopulmonary arrest.[1]
According to Vinik, et al., it was found that autonomic dysfunction symptoms such as orthostatic hypotension, gastroparesis, and gustatory sweating are more frequently identified in mortalities.[15]
See also
References
- 1 2 3 4 5 "Dysautonomia". NINDS. Retrieved 2012-04-03.
- ↑ Iodice, V; Sandroni, Paola; Vernino, Steven. "Efficacy of immunotherapy in seropositive and seronegative putative autoimmune autonomic ganglionopathy.". PubMed. NIH. Retrieved 13 September 2016.
- ↑ Lonsdale, Derrick (2009-03-01). "Dysautonomia, A Heuristic Approach to a Revised Model for Etiology of Disease". Evidence-Based Complementary and Alternative Medicine. 6 (1): 3–10. doi:10.1093/ecam/nem064. ISSN 1741-427X. PMC 2644268
 . PMID 18955227.
. PMID 18955227. - 1 2 3 4 5 6 7 8 9 10 11 12 "Autonomic Neuropathy Clinical Presentation: History, Physical, Causes". emedicine.medscape.com. Retrieved 2016-02-21.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Autonomic Neuropathy. Information about AN. Patient | Patient". Patient. Retrieved 2016-02-21.
- 1 2 3 4 5 6 7 8 9 "Autonomic neuropathy: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2016-02-20.
- ↑ KIRK, KATHERINE A; SHOYKHET, MICHAEL; JEONG, JONG H; TYLER-KABARA, ELIZABETH C; HENDERSON, MARYANNE J; BELL, MICHAEL J; FINK, ERICKA L (2012-08-01). "Dysautonomia after pediatric brain injury". Developmental Medicine and Child Neurology. 54 (8): 759–764. doi:10.1111/j.1469-8749.2012.04322.x. ISSN 0012-1622. PMC 3393822
 . PMID 22712762.
. PMID 22712762. - ↑ De Wandele I, Rombaut L, Leybaert L, Van , de Borne P, De Backer T, Malfait F, De Paepe A, Calders P (2014). "Dysautonomia and its underlying mechanisms in the hypermobility type of Ehlers-Danlos syndrome". Semin. Arthritis Rheum. 44: 93–100. doi:10.1016/j.semarthrit.2013.12.006. PMID 24507822.
- ↑ "Paraneoplastic syndromes of the nervous system". Mayo Clinic. Mayo Clinic. Retrieved 13 September 2016.
- ↑ Martínez-Martínez LA, Mora T, Vargas A, Fuentes-Iniestra M, Martínez-Lavín M (Apr 2014). "Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: a review of case-control studies.". J Clin Rheumatol. 20: 146–50. doi:10.1097/RHU.0000000000000089. PMID 24662556.
- ↑ Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894. "Autonomic Nervous System - National Library of Medicine". PubMed Health. Retrieved 2016-02-21.
- 1 2 3 4 5 6 7 8 9 Mustafa, Hossam I.; Fessel, Joshua P.; Barwise, John; Shannon, John R.; Raj, Satish R; Diedrich, André; Biaggioni, Italo; Robertson, David (2012-01-01). "Dysautonomia: Perioperative Implications". Anesthesiology. 116 (1): 205–215. doi:10.1097/ALN.0b013e31823db712. ISSN 0003-3022. PMC 3296831
 . PMID 22143168.
. PMID 22143168. - ↑ "H2 Blockers. Reducing stomach acid with H2 Blockers. | Patient". Patient. Retrieved 2016-02-21.
- ↑ http://www.medscape.com/viewarticle/473205_9
- ↑ Vinik, Aaron I.; Maser, Raelene E.; Mitchell, Braxton D.; Freeman, Roy (2003-05-01). "Diabetic Autonomic Neuropathy". Diabetes Care. 26 (5): 1553–1579. doi:10.2337/diacare.26.5.1553. ISSN 0149-5992. PMID 12716821.
Further reading
- Lara, Aline; Damasceno, Denis D.; Pires, Rita; Gros, Robert; Gomes, Enéas R.; Gavioli, Mariana; Lima, Ricardo F.; Guimarães, Diogo; Lima, Patricia (2010-04-01). "Dysautonomia Due to Reduced Cholinergic Neurotransmission Causes Cardiac Remodeling and Heart Failure". Molecular and Cellular Biology. 30 (7): 1746–1756. doi:10.1128/MCB.00996-09. ISSN 0270-7306. PMC 2838086
 . PMID 20123977.
. PMID 20123977. - Schiffer, Randolph B.; Rao, Stephen M.; Fogel, Barry S. (2003-01-01). Neuropsychiatry. Lippincott Williams & Wilkins. ISBN 9780781726559.
