Diphyllobothriasis
| Diphyllobothriasis | |
|---|---|
| Classification and external resources | |
| Specialty | infectious disease |
| ICD-10 | B70.0 |
| ICD-9-CM | 123.4 |
| DiseasesDB | 29539 |
| MedlinePlus | 001375 |
| eMedicine | med/571 |
| MeSH | D004169 |
Diphyllobothriasis is the infection caused by tapeworms of the Diphyllobothrium genus, commonly Diphyllobothrium latum.
Geographic distribution
Diphyllobothriasis occurs in areas where lakes and rivers coexist with human consumption of raw or undercooked freshwater fish. Such areas are found in Europe, newly independent states of the former Soviet Union, North America, Asia, Uganda, Peru (because of ceviche), and Chile. It is particularly common in Japan, because of sushi or sashimi.
Around the middle of the 20th century in Japan, before advancements in refrigeration, many sushi/sashimi connoisseurs suffered great morbidity and mortality from Diphyllobothrium after eating unrefrigerated sashimi. Through research in parasitology, scientists came to realize that the primary cause was the relatively favorable parasite-breeding conditions that raw fish offered.
The disease is rare in the United States. It was, however, once more common and was referred to as "Jewish housewife's disease" because Jewish housewives preparing the traditional "gefilte fish" frequently tasted the fish before it was cooked.
Clinical features
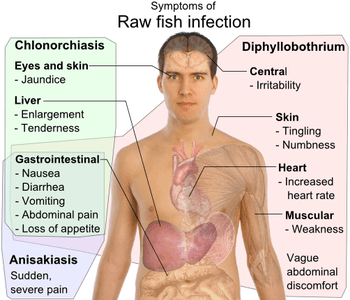
Diphyllobothriasis can last for decades if untreated. Most infections are asymptomatic. Manifestations may include abdominal discomfort, diarrhea, vomiting and weight loss. Vitamin B12 deficiency with subsequent megaloblastic anemia may occur, but has not for several decades in D. latum infections, possibly because of improved nutrition. In one test, nearly half of the ingested vitamin was absorbed by D. latum in otherwise healthy patients, while 80-100% was absorbed by the worm in patients with anemia. It is not known why anemia occurs in some cases but not others. Massive infections may result in intestinal obstruction. Migration of proglottids can cause cholecystitis or cholangitis.
Females cases are disproportionately reported, most likely due to the higher likelihood for them to be involved in meal preparation, rather than any morphological differences.
Diagnosis
Microscopic identification of eggs in the stool is the basis of specific diagnosis. Eggs are usually numerous and can be demonstrated without concentration techniques. Examination of proglottids passed in the stool is also of diagnostic value.
Diagnostic tool:
- Microscopy
- Morphologic comparison with other intestinal parasites
Though it is difficult to identify the eggs or proglottids to the species level, the distinction is of little medical importance because, like most adult tapeworms in the intestine, all members of this genus respond to the same drugs.
Treatment
Upon diagnosis, treatment is quite simple and effective. The standard treatment for diphyllobothriasis, as well as many other tapeworm infections is a single dose of praziquantel, 5–10 mg/kg orally once for both adults and children. An alternative treatment is niclosamide, 2 g orally once for adults or 50 mg/kg (max 2 g) for children.[6][7][8] One should note that praziquantel is not FDA-approved for this indication and niclosamide is not available for human use in the United States.[6] Reportedly, albendazole can also be effective.[9][10] Another interesting potential diagnostic tool and treatment is the contrast medium, Gastrografin, introduced into the duodenum, which allows both visualization of the parasite, and has also been shown to cause detachment and passing of the whole worm.[11][12]
Prevention
Avoid ingestion of raw freshwater fish. Adequate cooking or freezing of freshwater fish will kill the encysted fish tapeworm larvae. Also, because human feces is an important mechanism for spreading eggs, proper disposal of sewage can cut down on infection of fish and thus of humans.
References
- ↑ WaiSays: About Consuming Raw Fish Retrieved on April 14, 2009
- ↑ For Chlonorchiasis: Public Health Agency of Canada > Clonorchis sinensis - Material Safety Data Sheets (MSDS) Retrieved on April 14, 2009
- ↑ For Anisakiasis: WrongDiagnosis: Symptoms of Anisakiasis Retrieved on April 14, 2009
- ↑ For Diphyllobothrium: MedlinePlus > Diphyllobothriasis Updated by: Arnold L. Lentnek, MD. Retrieved on April 14, 2009
- ↑ For symptoms of diphyllobothrium due to vitamin B12-deficiency University of Maryland Medical Center > Megaloblastic (Pernicious) Anemia Retrieved on April 14, 2009
- 1 2 "Diphyllobothrium - Resources for Health Professionals". Parasites - CDC. 2012-01-10. Retrieved 2015-09-05.
- ↑ "Helminths: Cestode (tapeworm) infection: Niclosamide". WHO Model Prescribing Information: Drugs Used in Parasitic Diseases - Second Edition. WHO. 1995. Retrieved 2015-09-05.
- ↑ "Helminths: Cestode (tapeworm) infection: Praziquantel". WHO Model Prescribing Information: Drugs Used in Parasitic Diseases - Second Edition. WHO. 1995. Retrieved 2015-09-05.
- ↑ Molodozhnikova NM, Volodin AV, Bakulina NG (Nov–Dec 1991). "[The action of albendazole on the broad tapeworm]". Meditsinskaia parazitologiia i parazitarnye bolezni (in Russian). Moscow (6): 46–50. PMID 1818249.
- ↑ Jackson Y, Pastore R, Sudre P, Loutan L, Chappuis F (Dec 2007). "Diphyllobothrium latum outbreak from marinated raw perch, Lake Geneva, Switzerland". Emerging Infectious Diseases. 13 (12): 1957–1958. doi:10.3201/eid1312.071034. PMC 2876774
 . PMID 18258060. Retrieved 2015-09-05.
. PMID 18258060. Retrieved 2015-09-05. - ↑ Waki K, Oi H, Takahashi S, et al. (1986). "Successful treatment of Diphyllobothrium latum and Taenia saginata infection by intraduodenal 'Gastrografin' injection". Lancet. 2 (8516): 1124–6. doi:10.1016/S0140-6736(86)90532-5. PMID 2877274.
- ↑ Ko, S.B. “Observation of deworming process in intestinal Diphyllobothrium latum parasitism by Gastrografin injection into jejunum through double-balloon enteroscope.” (2008) from Letter to the Editor; American Journal of Gastroenterology, 103; 2149-2150.
External links
- "Diphyllobothriasis". CDC - DPDx - Laboratory Identification of Parasitic Diseases of Public Health Concern. 2013-11-29. Retrieved 2015-09-05.