Dioxins and dioxin-like compounds
Dioxins and dioxin-like compounds (DLCs) are compounds that are highly toxic environmental persistent organic pollutants (POPs). They are mostly by-products of various industrial processes - or, in case of dioxin-like PCBs and PBBs, part of intentionally produced mixtures.[1] They include:[2][3]
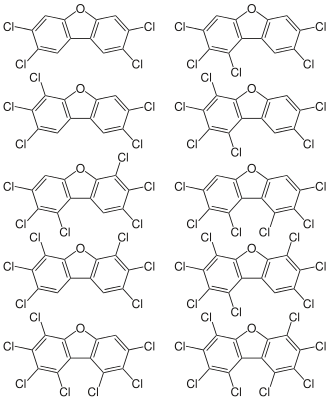
- Polychlorinated dibenzo-p-dioxins (PCDDs), or simply dioxins. PCDDs are derivatives of dibenzo-p-dioxin. There are 75 PCDD congeners, differing in the number and location of chlorine atoms, and seven of them are especially toxic, the most dangerous being 2,3,7,8-Tetrachlorodibenzodioxin (TCDD)
- Polychlorinated dibenzofurans (PCDFs), or furans. PCDFs are derivatives of dibenzofuran. There are 135 isomers, ten have dioxin-like properties.
- Polychlorinated/polybrominated biphenyls (PCBs/PBBs), derived from biphenyl, of which twelve are "dioxin-like". Under certain conditions PCBs may form dibenzofurans/dioxins through partial oxidation.
- Finally, dioxin may refer to 1,4-Dioxin proper, the basic chemical unit of the more complex dioxins. This simple compound is not persistent and has no PCDD-like toxicity.
Because dioxins refer to such a broad class of compounds that vary widely in toxicity, the concept of toxic equivalency factor (TEF) has been developed to facilitate risk assessment and regulatory control. Toxic equivalence factors (TEFs) exist for seven congeners of dioxins, ten furans and twelve PCBs. The reference congener is the most toxic dioxin 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) which per definition has a TEF of one.[4]
In reference to their importance as environmental toxicants the term dioxins is used almost exclusively to refer to the sum of compounds (as TEQ) from the above groups which demonstrate the same specific toxic mode of action associated with TCDD. These include 17 PCDD/Fs and 12 PCBs. Incidents of contamination with PCBs are also often reported as dioxin contamination incidents since it is this toxic characteristic which is of most public and regulatory concern.
Toxicity
Mechanism of toxicity
The toxic effects of dioxins are measured in fractional equivalencies of TCDD (2,3,7,8-tetrachlorodibenzo-p-dioxin), the most toxic and best studied member of its class (see TCDD for more detailed description of the mechanism). The toxicity is mediated through the interaction with a specific intracellular protein, the aryl hydrocarbon (AH) receptor, a transcriptional enhancer, affecting a number of other regulatory proteins.[5][6][7] This receptor is a transcription factor which is involved in expression of many genes. TCDD binding to the AH receptor induces the cytochrome P450 1A class of enzymes which function to break down toxic compounds, e.g., carcinogenic polycyclic hydrocarbons such as benzo(a)pyrene (but making many of them more toxic in the process).[8]
While the affinity of dioxins and related industrial toxicants to this receptor may not fully explain all their toxic effects including immunotoxicity, endocrine effects and tumor promotion, toxic responses appear to be typically dose-dependent within certain concentration ranges. A multiphasic dose-response relationship has also been reported, leading to uncertainty and debate about the true role of dioxins in cancer rates.[9]
The endocrine disrupting activity of dioxins is thought to occur as a down-stream function of AH receptor activation, with thyroid status in particular being a sensitive marker of exposure. It is important to note that TCDD, along with the other PCDDs, PCDFs and dioxin-like coplanar PCBs are not direct agonists or antagonists of hormones, and are not active in assays which directly screen for these activities such as ER-CALUX and AR-CALUX. These compounds have also not been shown to have any direct mutagenic or genotoxic activity.[10] Their main action in causing cancer is cancer promotion. A mixture of PCBs such as Aroclor may contain PCB compounds which are known estrogen agonists, but on the other hand are not classified as dioxin-like in terms of toxicity. Mutagenic effects have been established for some lower chlorinated chemicals such as 3-chlorodibenzofuran, which is neither persistent nor an AH receptor agonist.[11]
Toxicity in animals
The symptoms reported to be associated with dioxin toxicity in animal studies are incredibly wide ranging, both in the scope of the biological systems affected and in the range of dosage needed to bring these about.[2][3] Acute effects of single high dose dioxin exposure include wasting syndrome, and typically a delayed death of the animal in 1 to 6 weeks.[7] By far most toxicity studies have been performed using 2,3,7,8-tetrachlorodibenzo-p-dioxin.
The LD50 of TCDD varies wildly between species and even strains of the same species, with the most notable disparity being between the seemingly similar species of hamster and guinea pig. The oral LD50 for guinea pigs is as low as 0.5 to 2 μg/kg body weight, whereas the oral LD50 for hamsters can be as high as 1 to 5 mg/kg body weight.[3] Even between different mouse or rat strains there may be tenfold to thousandfold differences in acute toxicity.[3] Many pathological findings are seen in the liver, thymus and other organs.
Some chronic and sub-chronic exposures can be harmful at much lower levels, especially at particular developmental stages including foetal, neonatal and pubescent stages.[12] Well established developmental effects are cleft palate, hydronephrosis, disturbances in tooth development and sexual development as well as endocrine effects.[12]
Human toxicity
Dioxins have been considered highly toxic and able to cause reproductive and developmental problems, damage the immune system, interfere with hormones and also cause cancer.[13] This is based on animal studies. The best proven is chloracne.[2] Even in poisonings with huge doses of TCDD, the only persistent effects after the initial malaise have been chloracne and amenorrhea.[14][15] In occupational settings many symptoms have been seen, but exposures have always been to a multitude of chemicals including chlorophenols, chlorophenoxy acid herbicides, and solvents. Therefore, proof of dioxins as causative factors has been difficult.[16] The suspected effects in adults are liver damage, and alterations in heme metabolism, serum lipid levels, thyroid functions, as well as diabetes and immunological effects.[16]
In line with animal studies, developmental effects may be much more important than effects in adults. These include disturbances of tooth development,[17] and of sexual development.[18] An example of the variation in responses is clearly seen in a study following the Seveso disaster indicating that sperm count and motility were affected in different ways in exposed males, depending on whether they were exposed before, during or after puberty.[19]
Intrauterine exposure to dioxins and dioxin-like compounds as an environmental toxin in pregnancy has subtle effects on the child later in life that include changes in liver function, thyroid hormone levels, white blood cell levels, and decreased performance in tests of learning and intelligence.[20]
Exposure to dioxins can happen in a number of ways, most often as by-products of industrial waste. However, dioxins can result from natural processes including volcanic eruptions and forest fires, and manufacturing processes such as smelting, chlorine bleaching of paper pulp, and the creation of some herbicides and pesticides.[21] Even at levels 100X lower than those associated with its cancer causing effects, the presence of dioxin can cause immune system damage, severe reproductive and developmental problems, and interference with regulatory hormones.[22]
The Endometriosis Research Center (ERC) has testified before the California State Legislature concerning Assembly Bill 2820 [Cardoza, D-Merced] that, "feminine hygiene products (i.e. tampons) do indeed test positive for Dioxin. Dioxin, in turn, is a well-documented catalyst for Endometriosis - and the effects of Dioxin are cumulative; able to be measured as much as 20 or 30 years after exposure."[23] The ERC also references an independent study that found, in an assessment of four brands of tampons and four brands of baby diapers, dioxins "were present at detectable concentrations in all samples." The presence of this toxin in tampons may be linked to endometriosis because dioxins last a long time in the body; they are chemically stable and can be absorbed by fat tissue, where they are then stored in the body. Their half-life in the body is estimated to be 7 to 11 years.[21]
Carcinogenicity
Dioxins are well established carcinogens in animal studies, although the precise mechanistic role is not clear. Dioxins are not mutagenic or genotoxic. The United States Environmental Protection Agency has categorised dioxin, and the mixture of substances associated with sources of dioxin toxicity as a "likely human carcinogen".[24] The International Agency for Research on Cancer has classified TCDD as a human carcinogen (class 1) on the basis of clear animal carcinogenicity and limited human data, but was not able to classify other dioxins.[25] It is thought that the presence of dioxin can accelerate the formation of tumours and adversely affect the normal mechanisms for inhibiting tumour growth, without actually instigating the carcinogenic event.[10]
As with all toxic endpoints of dioxin, a clear dose-response relationship is very difficult to establish. After accidental or high occupational exposures there is evidence on human carcinogenicity.[26][27] There is much controversy especially on cancer risk at low population levels of dioxins.[9][26][28] Among fishermen with high dioxin concentrations in their bodies, cancer deaths were decreased rather than increased.[29] Some researchers have also proposed that dioxin induces cancer progression through a very different mitochondrial pathway.[30]
Risk assessment
The uncertainty and variability in the dose-response relationship of dioxins in terms of their toxicity, as well as the ability of dioxins to bioaccumulate mean that the tolerable daily intake (TDI) of dioxin has been set very low, 1-4 pg/kg body weight per day, i.e. 7x10−11 to 2.8x10−10g per 70-kg person per day, to allow for this uncertainty and ensure public safety in all instances. Specifically, the TDI has been assessed based on the safety of children born to mothers exposed all their lifetime prior to pregnancy to such a daily intake of dioxins.[31] It is likely that the TDI for other population groups could be somewhat higher. The most important cause for differences in different assessments is carcinogenicity. If the dose-response of TCDD in causing cancer is linear, it might be a true risk. If the dose-response is of a threshold-type or J-shape, there is little or no risk at the present concentrations. Understanding the mechanisms of toxicity better is hoped to increase the reliability of risk assessment.[1][32]
Controversy
Greenpeace and some other environmental groups have called for the chlorine industry to be phased out.[33][34][35] However, chlorine industry supporters say that "banning chlorine would mean that millions of people in the third world would die from want of disinfected water".[36] (Although critics point out the existence of alternative water disinfection methods.)
Sharon Beder and others have argued that the dioxin controversy has been very political and that large companies have tried to play down the seriousness of the problems of dioxin.[34][35][37] The companies involved have often said that the campaign against dioxin is based on "fear and emotion" and not on science.[38]
In 2008, Chile experienced a pork crisis caused by high dioxin concentrations in their pork exports. The contamination was found to be due to zinc oxide used in pork feed, and caused reputational and financial losses for the country, as well as leading to the introduction of new food safety regulations.[39]
Human intake and levels
Most intake of dioxin-like chemicals is from food of animal origin: meat, dairy products, or fish predominate, depending on the country.[2][40][41] The daily intake of dioxins and dioxin-like PCBs as TEQ is of the order of 100 pg/day, i.e. 1-2 pg/kg/day.[2] In many countries both the absolute and relative significance of dairy products and meat have decreased due to strict emission controls, and brought about the decrease of total intake. E.g. in the United Kingdom the total intake of PCDD/F in 1982 was 239 pg/day and in 2001 only 21 pg/day (WHO-TEQ).[2] Since the half-lives are very long (for e.g. TCDD 7–8 years), the body burden will increase almost over the whole lifetime. Therefore, the concentrations may increase five- to tenfold from age 20 to age 60.[42][43] For the same reason, short term higher intake such as after food contamination incidents, is not crucial unless it is extremely high or lasts for several months or years.[2]
The highest body burdens were found in Western Europe in the 1970s and early 1980s,[2][44][45] and the trends have been similar in the U.S.[46] The most useful measure of time trends is concentration in breast milk measured over decades.[40][44] In many countries the concentrations have decreased to about one tenth of those in the 1970s, and the total TEQ concentrations are now of the order of 10-30 pg/g fat[7][44] (please note the units, pg/g is the same as ng/kg, or the non-standard expression ppt used sometimes in America).[2] The decrease is due to strict emission controls and also to the control of concentrations in food.[47][48] In the U.S. young adult female population (age group 20-39), the concentration was 9.7 pg/g lipid in 2001-2002 (geometric mean).[43]
Certain professions such as subsistence fishermen in some areas are exposed to exceptionally high amounts of dioxins and related substances.[49] This along with high industrial exposures may be the most valuable source of information on the health risks of dioxins.
Uses
Dioxins have no common uses. They are manufactured on a small scale for chemical and toxicological research, but mostly exist as by-products of industrial processes such as bleaching paper pulp, pesticide manufacture, and combustion processes such as waste incineration. The defoliant Agent Orange contained dioxins.[50] The production and use of dioxins was banned by the Stockholm Convention in 2001.
Sources
Environmental sources
PCB-compounds, always containing low concentrations of dioxin-like PCBs and PCDFs, were synthesized for various technical purposes (see Polychlorinated biphenyls). They have entered the environment through accidents such as fires or leaks from transformers or heat exchangers, or from PCB-containing products in landfills or during incineration. Because PCBs are somewhat volatile, they have also been transported long distances by air leading to global distribution including the Arctic.
PCDD/F-compounds were never synthesized for any purpose, except for small quantities for scientific research.[7] Small amounts of PCDD/Fs are formed whenever organics, oxygen and chlorine are available at suitable temperatures.[51] This is augmented by metal catalysts such as copper. The optimal temperature range is 400 °C to 700 °C. This means that formation is highest when organic material is burned in less-than-optimal conditions such as open fires, building fires, domestic fireplaces, and poorly operated and/or designed solid waste incinerators.[2] Historically, municipal and medical waste incineration was the most important source of PCDD/Fs.
Other sources of PCDD/F include:
- Metal smelting and refining
- Chlorine bleaching of pulp and paper - historically important source of PCDD/Fs to waterways.
- Synthesis side products of several chemicals, especially PCBs, chlorophenols, chlorophenoxy acid herbicides and hexachlorophene.[25]
- Uncontrolled combustion, particularly open burning of waste ("backyard barrel burning"), accidental fires, wildfires.
- (Historical) Engines using leaded fuel, which contained the additives 1,2-Dichloroethane and 1,2-Dibromoethane.
In waste incineration
Improvements and changes have been made to nearly all industrial sources to reduce PCDD/F production. In waste incineration, large amounts of publicity and concern surrounded dioxin-like compounds during the 1980s-1990s continues to pervade the public consciousness, especially when new incineration and waste-to-energy facilities are proposed. As a result of these concerns, incineration processes have been improved with increased combustion temperatures (over 1000 °C), better furnace control, and sufficient residence time allotted to ensure complete oxidation of organic compounds. Ideally, an incineration process oxidizes all carbon to CO2 and converts all chlorine to HCl or inorganic chlorides prior to the gases passing through the temperature window of 700-400 °C where PCDD/F formation is possible. These substances cannot easily form organic compounds, and HCl is easily and safely neutralized in the scrubber while CO2 is vented to the atmosphere. Inorganic chlorides are incorporated into the ash.
Scrubber and particulate removal systems manage to capture most of the PCDD/F which forms even in sophisticated incineration plants. These PCDD/Fs are generally not destroyed but moved into the fly ash. Catalytic systems have been designed which destroy vapor-phase PCDD/Fs at relatively low temperatures. This technology is often combined with the baghouse or SCR system at the tail end of an incineration plant.
European Union limits for concentration of dioxin-like compounds in the discharged flue gas is 0.1 ng/Nm³ TEQ.[52]
Both in Europe[53] and in U.S.A.,[54] the emissions have decreased dramatically since the 1980s, by even 90%. This has also led to decreases in human body burdens, which is neatly demonstrated by the decrease of dioxin concentrations in breast milk.[44]
Open burning of waste (backyard barrel burning) has not decreased effectively, and in the U.S. it is now the most important source of dioxins. Total U.S. annual emissions decreased from 14 kg in 1987 to 1.4 kg in 2000. However, backyard barrel burning decreased only modestly from 0.6 kg to 0.5 kg, resulting in over one third of all dioxins in the year 2000 from backyard burning alone.[54]
Low concentrations of dioxins have been found in some soils without any anthropogenic contamination. A puzzling case of milk contamination was detected in Germany. The source was found to be kaolin added to animal feed. Dioxins have been repeatedly detected in clays from Europe and USA since 1996, with contamination of clay assumed to be the result of ancient forest fires or similar natural events with concentration of the PCDD/F during clay sedimentation.[55]
Environmental persistence and bioaccumulation
All groups of dioxin-like compounds are persistent in the environment.[56] Neither soil microbes nor animals are able to break down effectively the PCDD/Fs with lateral chlorines (positions 2,3,7, and 8). This causes very slow elimination. Ultraviolet light is able to slowly break down these compounds. Lipophilicity (tendency to seek for fat-like environments) and very poor water solubility make these compounds move from water environment to living organisms having lipid cell structures. This is called bioaccumulation. Increase in chlorination increases both stability and lipophilicity. The compounds with the very highest chlorine numbers (e.g. octachlorodibenzo-p-dioxin) are, however, so poorly soluble that this hinders their bioaccumulation.[56] Bioaccumulation is followed by biomagnification. Lipid-soluble compounds are first accumulated to microscopic organisms such as phytoplankton (plankton of plant character, e.g. algae). Phytoplankton is consumed by animal plankton, this by invertebrates such as insects, these by small fish, and further by large fish and seals. At every stage or trophic level, the concentration is higher, because the persistent chemicals are not "burned off" when the higher organism uses the fat of the prey organism to produce energy.
Due to bioaccumulation and biomagnification, the species at the top of the trophic pyramid are most vulnerable to dioxin-like compounds. In Europe, the white-tailed eagle and some species of seals have approached extinction due to poisoning by persistent organic pollutants.[57] Likewise, in America, the population of bald eagles declined because of POPs causing thinning of eggshells and other reproductive problems.[58] Usually, the failure has been attributed mostly to DDT, but dioxins are also a possible cause of reproductive effects. Both in America and in Europe, many waterfowl have high concentrations of dioxins, but usually not high enough to disturb their reproductive success.[57][59] Due to supplementary winter feeding and other measures also, the white-tailed eagle is recovering (see White-tailed eagle). Also, ringed seals in the Baltic Sea are recovering.
Humans are also at the top of the trophic pyramid, particularly newborns. Exclusively breastfed newborns were estimated to be exposed to a total of 800 pg TEQ/day, leading to an estimated body weight-based dose of 242 pg TEQ/kg/day.[60] Due to a multitude of food sources of adult humans exposure is much less averaging at 1 pg TEQ/kg-day,[60] and dioxin concentrations in adults are much less at 10-100 pg/g, compared with 9000 to 340,000 pg/g (TEQ in lipid) in eagles[57] or seals feeding almost exclusively on fish.
Because of different physicochemical properties, not all congeners of dioxin-like compounds find their routes to human beings equally well. Measured as TEQs, the dominant congeners in human tissues are 2,3,7,8-TCDD, 1,2,3,7,8-PeCDD, 1,2,3,6,7,8-HxCDD and 2,3,4,7,8-PeCDF.[2] This is very different from most sources where hepta- and octa-congeners may predominate. The WHO panel re-evaluating the TEF values in 2005 expressed their concern that emissions should not be uncritically measured as TEQs, because all congeners are not equally important.[4] They stated that "when a human risk assessment is to be done from abiotic matrices, factors such as fate, transport, and bioavailability from each matrix be specifically considered".[4]
All POPs are poorly water-soluble, especially dioxins. Therefore, ground water contamination has not been a problem, even in cases of severe contamination due to the main chemicals such as chlorophenols.[61] In surface waters, dioxins are bound to organic and inorganic particles.
Fate of dioxins in human body
The same features causing persistence of dioxins in the environment, also cause very slow elimination in humans and animals. Because of low water solubility, kidneys are not able to secrete them in urine as such. They should be metabolised to more water-soluble metabolites, but also metabolism especially in humans is extremely slow. This results in biological half-lives of several years for all dioxins. That of TCDD is estimated to be 7 to 8 years, and for other PCDD/Fs from 1.4 to 13 years, PCDFs on average slightly shorter than PCDDs.[2][62]
Dioxins are absorbed well from the digestive tract, if they are dissolved in fats or oils (e.g. in fish or meat).[3] On the other hand, dioxins tend to adsorb tightly to soil particles, and absorption may be quite low: 13.8% of the given dose of TEQs in contaminated soil was absorbed.[63]
In mammalian organisms, dioxins are found mostly in fat. Concentrations in fat seem to be relatively similar, be it serum fat, adipose tissue fat, or milk fat. This permits measuring dioxin burden by analysing breast milk.[44] Initially, however, at least in laboratory animals, after a single dose, high concentrations are found in the liver, but in a few days, adipose tissue will predominate. In rat liver, however, high doses cause induction of CYP1A2 enzyme, and this binds dioxins. Thus, depending on the dose, the ratio of fat and liver tissue concentrations may vary considerably in rodents.[3]
Sources of human exposure
The most important source of human exposure is fatty food of animal origin (see Human intake, above),[40] and breast milk.[60] There is much variation between different countries as to the most important items. In U.S. and Central Europe, milk, dairy products and meat have been by far the most important sources. In some countries, notably in Finland and to some extent in Sweden, fish is important due to contaminated Baltic fish and very low intake from any other sources.[2] In most countries, a significant decrease of dioxin intake has occurred due to stricter controls during the last 20 years.
Historically occupational exposure to dioxins has been a major problem.[25] Dioxins are formed as important toxic side products in the production of PCBs, chlorophenols, chlorophenoxy acid herbicides, and other chlorinated organic chemicals. This caused very high exposures to workers in poorly controlled hygienic conditions. Many workers had chloracne. In a NIOSH study in the U.S., the average concentration of TCDD in exposed persons was 233 ng/kg (in serum lipid) while it was 7 ng/kg in unexposed workers, even though the exposure had been 15–37 years earlier.[25] This indicates a huge previous exposure. In fact the exact back-calculation is debated, and the concentrations may have been even several times higher than originally estimated.[64]
Handling and spraying of chlorophenoxy acid herbicides may also cause quite high exposures, as clearly demonstrated by the users of Agent Orange in the Malayan Emergency and in the Vietnam War. The highest concentrations were detected in nonflying enlisted personnel (e.g. filling the tanks of planes), although the variation was huge, 0 to 618 ng/kg TCDD (mean 23.6 ng/kg).[25] Other occupational exposures (working at paper and pulp mills, steel mills and incinerators) have been remarkably lower.[25]
Accidental exposures have been huge in some cases. The highest concentrations in people after the Seveso accident were 56,000 ng/kg, and the highest exposure ever recorded was found in Austria in 1998, 144,000 ng/kg (see TCDD).[14] This is equivalent to a dose of 20 to 30 μg/kg TCDD, a dose that would be lethal to guinea pigs and some rat strains.
Exposure from contaminated soil is possible when dioxins are blown up in dust, or children eat dirt. Inhalation was clearly demonstrated in Missouri in the 1970s, when waste oils were used as dust suppressant in horse arenas. Many horses and other animals were killed due to poisoning.[65] Dioxins are neither volatile nor water-soluble, and therefore exposure of human beings depends on direct eating of soil or production of dust which carries the chemical. Contamination of ground water or breathing vapour of the chemical are not likely to cause a significant exposure. Currently, in the US, there are 126 Superfund sites with a completed exposure pathway contaminated with dioxins.
Further, PCBs are known to pass through treatment plants and accumulate in sludge which is used on farm fields in certain countries. In 2011 in South Carolina, SCDHEC enacted emergency sludge regulations after PCBs were found to have been discharged to a waste treatment plant.[66]
PCBs are also known to flush from industry and land (aka sludge fields) to contaminate fish,[67] as they have up and down the Catawba River in North and South Carolina. State authorities have posted fish consumption advisories due to accumulation of PCBs in fish tissue.[68]
TEF values
All dioxin-like compounds share a common mechanism of action via the aryl hydrocarbon receptor (AHR), but their potencies are very different. This means that similar effects are caused by all of them, but much larger doses of some of them are needed than of TCDD. Binding to the AHR as well as persistence in the environment and in the organism depends on the presence of so-called "lateral chlorines", in case of dioxins and furans, chlorine substitutes in positions 2,3,7, and 8.[2] Each additional non-lateral chlorine decreases the potency, but qualitatively the effects remain similar. Therefore, a simple sum of different dioxin congeners is not a meaningful measure of toxicity. To compare the toxicities of various congeners and to render it possible to make a toxicologically meaningful sum of a mixture, a toxicity equivalency (TEQ) concept was created.[4]
Each congener has been given a toxicity equivalence factor (TEF). This indicates its relative toxicity as compared with TCDD. Most TEFs have been extracted from in vivo toxicity data on animals, but if these are missing (e.g. in case of some PCBs), less reliable in vitro data have been used.[4] After multiplying the actual amount or concentration of a congener by its TEF, the product is the virtual amount or concentration of TCDD having effects of the same magnitude as the compound in question. This multiplication is done for all compounds in a mixture, and these "equivalents of TCDD" can then simply be added, resulting in TEQ, the amount or concentration of TCDD toxicologically equivalent to the mixture.
The TEQ conversion makes it possible to use all studies on the best studied TCDD to assess the toxicity of a mixture. This resembles the common measure of all alcoholic drinks: beer, wine and whiskey can be added together as absolute alcohol, and this sum gives the toxicologically meaningful measure of the total impact.
The TEQ only applies to dioxin-like effects mediated by the AHR. Some toxic effects (especially of PCBs) may be independent of the AHR, and those are not taken into account by using TEQs.
TEFs are also approximations with certain amount of scientific judgement rather than scientific facts. Therefore, they may be re-evaluated from time to time. There have been several TEF versions since the 1980s. The most recent re-assessment was by an expert group of the World Health organization in 2005.



WHO Toxic Equivalence Factors (WHO-TEF) for the dioxin-like congeners of concern [4]
| Polychlorinated dioxins | |
| 2,3,7,8-TCDD | 1 |
| 1,2,3,7,8-PeCDD | 1 |
| 1,2,3,4,7,8-HxCDD | 0.1 |
| 1,2,3,6,7,8-HxCDD | 0.1 |
| 1,2,3,7,8,9-HxCDD | 0.1 |
| 1,2,3,4,6,7,8-HpCDD | 0.01 |
| OCDD | 0.0003 |
| Polychlorinated dibenzofurans | |
| 2,3,7,8-TCDF | 0.1 |
| 1,2,3,7,8-PeCDF | 0.03 |
| 2,3,4,7,8-PeCDF | 0.3 |
| 1,2,3,4,7,8-HxCDF | 0.1 |
| 1,2,3,6,7,8-HxCDF | 0.1 |
| 1,2,3,7,8,9-HxCDF | 0.1 |
| 2,3,4,6,7,8-HxCDF | 0.1 |
| 1,2,3,4,6,7,8-HpCDF | 0.01 |
| 1,2,3,4,7,8,9-HpCDF | 0.01 |
| OCDF | 0.0003 |
| Non-ortho-substituted PCBs | |
| 3,3',4,4'-TCB (PCB77) | 0.0001 |
| 3,4,4',5-TCB (PCB81) | 0.0003 |
| 3,3',4,4',5-PeCB (PCB126) | 0.1 |
| 3,3',4,4',5,5'-HxCB (PCB169) | 0.03 |
| Mono-ortho-substituted PCBs | |
| 2,3,3',4,4'-PeCB (PCB105) | 0.00003 |
| 2,3,4,4',5-PeCB (PCB114) | 0.00003 |
| 2,3',4,4',5-PeCB (PCB118) | 0.00003 |
| 2',3,4,4',5-PeCB (PCB123) | 0.00003 |
| 2,3,3',4,4',5-HxCB (PCB156) | 0.00003 |
| 2,3,3',4,4',5'-HxCB (PCB157) | 0.00003 |
| 2,3',4,4',5,5'-HxCB (PCB167) | 0.00003 |
| 2,3,3',4,4',5,5'-HpCB (PCB189) | 0.00003 |
(T = tetra, Pe = penta, Hx = hexa, Hp = hepta, O = octa)
Dioxin screening
There are two main methods for screening of dioxins and dioxin-like compounds:
- CALUX, or Chemical Activated Luciferase gene eXpression is a novel High-throughput screening bioassay. In comparison to HRGC-MS, it's a much faster and cheaper method as it is not reliant on expensive machinery used in HRGC-MS.
- HRGC-MS, or High Resolution Gas Chromatography Mass Spectrometry was the first screening method for 29 dioxin and DLC congeners.
References
- 1 2 "Are the dioxins the most dangerous chemicals in our environment?". opasnet.org.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Synopsis on dioxins and PCBs". thl.fi.
- 1 2 3 4 5 6 Pohjanvirta R., Tuomisto J.; Tuomisto (1994). "Short-term toxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin in laboratory animals: effects, mechanisms, and animal models". Pharmacol. Rev. 46 (4): 483–549. PMID 7899475.
- 1 2 3 4 5 6 Birnbaum L.S., Denison M., Vito M. De, Farland W., Feeley M., Fiedler H., Hakansson H., -1#den Berg The, Hanberg A.; et al. (2006). "World Health Organization reevaluation of human and mammalian toxic equivalency factors for dioxins and dioxin-like compounds". Toxicol Sci. 93 (2): 223–241. doi:10.1093/toxsci/kfl055. PMC 2290740
 . PMID 16829543.
. PMID 16829543. - ↑ Dencker L (1985). "The role of receptors in 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) toxicity". Arch. Toxicol. Suppl. Archives of Toxicology. 8: 43–60. doi:10.1007/978-3-642-69928-3_5. ISBN 978-3-540-13670-5. PMID 3006634.
- ↑ L. Poellinger. Mechanistic aspects – the dioxin (aryl hydrocarbon) receptor (2000). "Mechanistic aspects—the dioxin (aryl hydrocarbon) receptor.". Food Additives and Contaminants. 17 (4): 261–266. doi:10.1080/026520300283333. PMID 10912240.
- 1 2 3 4 J. Lindén, S. Lensu, J. Tuomisto, R. Pohjanvirta.; Lensu; Tuomisto; Pohjanvirta (2010). "Dioxins, the aryl hydrocarbon receptor and the central regulation of energy balance. A review". Frontiers in Neuroendocrinology. 31 (4): 452–478. doi:10.1016/j.yfrne.2010.07.002. PMID 20624415.
- ↑ Okey, A. B. (2007). "An aryl hydrocarbon receptor odyssey to the shores of toxicology: The Deichmann lecture". International congress of toxicology-XI. Toxicological Sciences. 98 (1): 5–38. doi:10.1093/toxsci/kfm096. PMID 17569696.
- 1 2 FN ISI Export Format VR 1.0 PT J TI The J-shaped dioxin dose response curve AU Kayajanian, GM SO ECOTOXICOLOGY AND ENVIRONMENTAL SAFETY VL 51 IS 1 BP 1 EP 4 PY 2002 TC 6 AB This commentary responds to a recent statistical treatment of cancer incidence data in selected workers exposed to dioxin from an earlier NIOSH chemical plant study. Contrary to the NIOSH authors' new findings, the cancer incidence response to increasing dioxin exposure is J-shaped, just as it is in the two major data sets that they failed to reference or explain away. The NIOSH statistical treatment obscured the significant reduction in cancer incidence that occurs at low dioxin exposures. Even though cancer incidence may increase at high dioxin exposures, such increase may be preceded at lower exposures by a significant reduction. (C) 2002 Elserier Science. UT WOS:000173569400001 SN 0147-6513 DI 10.1006/eesa.2001.2115 ER EF
- 1 2 Y.P. Dragan, D. Schrenk; Schrenk (2000). "Animal studies addressing the carcinogenicity of TCDD (or related compounds) with an emphasis on tumour promotion". Food Additives and Contaminants. 17 (4): 289–302. doi:10.1080/026520300283360. PMID 10912243.
- ↑ Matsumoto M, Ando M; Ando (1991). "Mutagenicity of 3-chlorodibenzofuran and its metabolic activation". Environ Mol Mutagen. 17 (2): 104–11. doi:10.1002/em.2850170207. PMID 2009865.
- 1 2 Birnbaum L.S., Tuomisto J.; Tuomisto (2000). "Non-carcinogenic effects of TCDD in animals". Food Addit. Contam. 17 (4): 275–288. doi:10.1080/026520300283351. PMID 10912242.
- ↑ WHO: Dioxins and their effects on human health, Fact sheet N° 225, May 2010, Accessed October 2, 2011
- 1 2 Geusau A., Abraham K., Geissler K., Sator M.O., Stingl G., Tschachler E.; Abraham; Geissler; Sator; Stingl; Tschachler (2001). "Severe 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) intoxication: clinical and laboratory effects". Environ. Health Perspect. 109 (8): 865–869. doi:10.1289/ehp.01109865. PMC 1240417
 . PMID 11564625.
. PMID 11564625. - ↑ Sorg O.; Zennegg M.; Schmid P.; Fedosyuk R.; Valikhnovskyi R.; Gaide O.; Kniazevych V.; Saurat J.H. (2009). "2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) poisoning in Victor Yushchenko: identification and measurement of TCDD metabolites". Lancet. 374: 1179–1185. doi:10.1016/s0140-6736(09)60912-0.
- 1 2 Sweeney M.H., Mocarelli P.; Mocarelli (2000). "Human health effects after exposure to 2,3,7,8- TCDD". Food Addit. Contam. 17 (4): 303–316. doi:10.1080/026520300283379. PMID 10912244.
- ↑ Alaluusua S., Calderara P., Gerthoux P.M., Lukinmaa P.L., Kovero O., Needham L., Patterson Jr., Tuomisto J., Mocarelli P.; Calderara; Gerthoux; Lukinmaa; Kovero; Needham; Patterson; Tuomisto; Mocarelli (2004). "Developmental dental aberrations after the dioxin accident in Seveso". Environ. Health Perspect. 112 (13): 1313–1318. doi:10.1289/ehp.6920. PMC 1247522
 . PMID 15345345.
. PMID 15345345. - ↑ P. Mocarelli, P.M. Gerthoux, E. Ferrari, D.G. Patterson Jr., S.M. Kieszak, P. Brambilla, N. Vincoli, S. Signorini, P. Tramacere, V. Carreri, E.J. Sampson, W.E. Turner, L.L. Needham, "Paternal concentrations of dioxin and sex ratio of offspring, Lancet 355 (2000) 1858–1863.
- ↑ FN ISI Export Format VR 1.0 PT J AU Mocarelli, P Gerthoux, PM Patterson, DG Milani, S Limonta, G Bertona, M Signorini, S Tramacere, P Colombo, L Crespi, C Brambilla, P Sarto, C Carreri, V Sampson, EJ Turner, WE Needham, LL AF Mocarelli, Paolo Gerthoux, Pier Mario Patterson, Donald G., Jr. Milani, Silvano Limonta, Giuseppe Bertona, Maria Signorini, Stefano Tramacere, Pierluigi Colombo, Laura Crespi, Carla Brambilla, Paolo Sarto, Cecilia Carreri, Vittorio Sampson, Eric J. Turner, Wayman E. Needham, Larry L. TI Dioxin exposure, from infancy through puberty, produces endocrine disruption and affects human semen quality SO ENVIRONMENTAL HEALTH PERSPECTIVES SN 0091-6765 PD JAN PY 2008 VL 116 IS 1 BP 70 EP 77 DI 10.1289/ehp.10399 UT ISI:000252142100027 ER EF
- ↑ Facts about Dioxins. from Minnesota Department of Health. Updated October 2006
- 1 2 http://www.who.int/mediacentre/factsheets/fs225/en/
- ↑ "Dioxin Concentrations in Women with Endometriosis,"Hum Reprod 1997 Feb;12(2):373-5 (ISSN 0268-1161); Mayani A; Barel S; Soback S; Almagor M, Department of OBGYN, Bikur Cholim Hospital, Israel
- ↑ https://www.endocenter.org/endostudy.htm
- ↑ http://www.health.state.mn.us/divs/eh/risk/guidance/dioxinmemo1.html
- 1 2 3 4 5 6 IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Volume 69, Lyon, 1997
- 1 2 Kogevinas M (2000). "Studies of cancer in humans". Food Additives and Contaminants. 17 (4): 317–324. doi:10.1080/026520300283388. PMID 10912245.
- ↑ Pesatori A.C., Consonni D., Rubagotti M., Grillo P., Bertazzi P.A.; Consonni; Rubagotti; Grillo; Bertazzi (2009). "Cancer incidence in the population exposed to dioxin after the Seveso accident": twenty years of follow-up". Environ. Health. 8: 39. doi:10.1186/1476-069x-8-39.
- ↑ Tuomisto J.T., Pekkanen J., Kiviranta H., Tukiainen E., Vartiainen T., Tuomisto J.; Pekkanen; Kiviranta; Tukiainen; Vartiainen; Tuomisto (2004). "Soft-tissue sarcoma and dioxin: a case-control study,". Int. J. Cancer. 108 (6): 893–900. doi:10.1002/ijc.11635. PMID 14712494.
- ↑ Turunen A.W., Verkasalo P.K., Kiviranta H., Pukkala E., Jula A., Mannisto S., Rasanen R., Marniemi J., Vartiainen T.; et al. (2008). "Mortality in a cohort with high fish consumption". Int. J. Epidemiol. 37 (5): 1008–1017. doi:10.1093/ije/dyn117. PMID 18579573.
- ↑ FN ISI Export Format VR 1.0 PT J TI Cancer and TCDD: The mitochondrial connection AU Mead, MN SO ENVIRONMENTAL HEALTH PERSPECTIVES VL 116 IS 3 BP A112 EP A112 PY 2008 TC 0 UT WOS:000253670600010 SN 0091-6765 ER EF
- ↑ "Consultation on assessment of the health risk of dioxins; re-evaluation of the tolerable daily intake (TDI): executive summary". Food Addit Contam. 17 (4): 223–40. April 2000. doi:10.1080/713810655. PMID 10912238.
- ↑ Tuomisto J (2005). "Does mechanistic understanding help in risk assessment – the example of dioxins, Toxicol". Appl. Pharmacol. 207 (2): 2–10. doi:10.1016/j.taap.2005.01.053.
- ↑ "Dioxin Controversy - What are Dioxins?". uow.edu.au.
- 1 2 Sharon Beder. 'The dioxin controversy: spilling over into schools', Australian Science Teachers' Journal, November 1998, pp. 28-34.
- 1 2 Sharon Beder (2000). Global Spin: The Corporate Assault on Environmentalism, Scribe Publications, chapters 9 and 13.
- ↑ Sharon Beder (2000) Global Spin: The Corporate Assault on Environmentalism, Scribe Publications, p. 153.
- ↑ Ronald Christaldi. Book Review: Dying From Dioxin by Lois Marie Gibbs Journal of Land Use and Environmental Law, 1996.
- ↑ Sharon Beder (2000). Global Spin: The Corporate Assault on Environmentalism, Scribe Publications, p. 154.
- ↑ Kim, Meekyung; Choi, Si-Weon; Guerrero, Pedro; Norambuena, Julio; Chung, Gab-Soo; et al. (8 January 2011). "Formation of polychlorinated dibenzo- p-dioxins/dibenzofurans (PCDD/Fs) from a refinery process for zinc oxide used in feed additives: A source of dioxin contamination in Chilean pork". Chemosphere. 82 (9): 1225–1229. doi:10.1016/j.chemosphere.2010.12.040. PMID 21216436. Retrieved 17 April 2014. Missing
|last2=in Authors list (help) - 1 2 3 Liem A.K., Furst P., Rappe C.; Fürst; Rappe (2000). "Exposure of populations to dioxins and related compounds". Food Addit. Contam. 17 (4): 241–259. doi:10.1080/026520300283324. PMID 10912239.
- ↑ Dioxins And Dioxin-Like Compounds In The Food Supply: Strategies To De-crease Exposure Food and Nutrition Board (FNB), Institute of Medicine
- ↑ Kiviranta H., Tuomisto J.T., Tuomisto J., Tukiainen E., Vartiainen T.; Tuomisto; Tuomisto; Tukiainen; Vartiainen (2005). "Polychlorinated dibenzo-p-dioxins, dibenzofurans, and biphenyls in the general population in Finland". Chemosphere. 60 (7): 854–869. doi:10.1016/j.chemosphere.2005.01.064. PMID 15992592.
- 1 2 Patterson Jr, Turner W.E., Caudill S.P., Needham L.L.; Turner; Caudill; Needham (2008). "Total TEQ reference range (PCDDs, PCDFs, cPCBs, mono-PCBs) for the US population 2001-2002". Chemosphere. 73 (1 Suppl): S261–77. doi:10.1016/j.chemosphere.2007.08.074. PMID 18511103.
- 1 2 3 4 5 WHO Fact sheet on POPs
- ↑ Noren K., Meironyte D.; Meironyté (2000). "Certain organochlorine and organobromine contaminants in Swedish human milk in perspective of past 20-30 years". Chemosphere. 40 (9–11): 1111–1123. doi:10.1016/s0045-6535(99)00360-4. PMID 10739053.
- ↑ Schecter A., Papke O., Tung K.C., Joseph J., Harris T.R., Dahlgren J.; p??Pke; Tung; Joseph; Harris; Dahlgren (2005). "Polybrominated diphenyl ether flame retardants in the U.S. population: current levels, temporal trends, and comparison with dioxins, dibenzofurans, and polychlorinated biphenyls". J. Occup. Environ. Med. 47 (3): 199–211. doi:10.1097/01.jom.0000158704.27536.d2. PMID 15761315.
- ↑ Furst P (2006). "Dioxins, polychlorinated biphenyls and other organohalogen compounds in human milk. Levels, correlations, trends and exposure through breastfeeding". Mol. Nutr. Food Res. 50 (10): 922–933. doi:10.1002/mnfr.200600008. PMID 17009213.
- ↑ Lignell S., Aune M., Darnerud P.O., Cnattingius S., Glynn A.; Aune; Darnerud; Cnattingius; Glynn (2009). "Persistent organochlorine and organobromine compounds in mother's milk from Sweden 1996-2006: compound-specific temporal trends". Environ. Res. 109 (6): 760–767. Bibcode:2009ER....109..760L. doi:10.1016/j.envres.2009.04.011. PMID 19477439.
- ↑ Kiviranta H, Vartiainen T, Tuomisto J; Vartiainen; Tuomisto (2002). "Polychlorinated dibenzo-p-dioxins, dibenzofurans, and biphenyls in fishermen in Finland". Environmental Health Perspectives. 110 (4): 355–361. doi:10.1289/ehp.02110355. PMID 11940453.
- ↑ Dioxins – ToxFAQs: Chemical Agent Briefing Sheets (CABS)
- ↑ "Where do the dioxins come from?". opasnet.org.
- ↑ "EU limit value". europa.eu.
- ↑ Quass U.; et al. (2004). Chemospere. 54: 1319–1327. Missing or empty
|title=(help) - 1 2 "An Inventory of Sources and Environmental Releases of Dioxin-Like Compounds in the U.S. for the Years 1987, 1995, and 2000 (Final, Nov 2006)". epa.gov.
- ↑ Schmitz M.; et al. ", Dioxins and primary kaolin and secondary kaolinic clays". Environ. Sci. Technol. 2011 (45): 461–467.
- 1 2 Claes Bernes: Persistent organic pollutants. Swedish Environmental Protection Agency, Stockholm 1998. ISBN 91-620-1189-8.
- 1 2 3 Koistinen J.; et al. (1995). "PCDEs, PCBs, PCDDs and PCDFs in black guillemots and white-tailed eagles from the Baltic Sea". Chemosphere. 1995 (30): 1671–1684. doi:10.1016/0045-6535(95)00053-b.
- ↑ Bull J, Farrand, J Jr (1987). Audubon Society Field Guide to North American Birds: Eastern Region. New York: Alfred A. Knopf. pp. 468–9. ISBN 0-394-41405-5
- ↑ EU Dioxin exposure and health data 1999
- 1 2 3 Matthew Lorber; Linda Phillips (Jun 2002). "Infant exposure to dioxin-like compounds in breast milk.". Environ Health Perspect. 110 (6): A325–A332. doi:10.1289/ehp.021100325. Retrieved 13 September 2014.
- ↑ Vartiainen T; et al. (1995). "Polychlorodibenzo-p-dioxin and polychlorodibenzofuran concentrations in lake-sediments and fish after a ground-water pollution with chlorophenols". Chemosphere. 1995 (30): 1439–1451. doi:10.1016/0045-6535(95)00037-9.
- ↑ Milbrath, M. O.; Wenger, Y; Chang, C. W.; Emond, C; Garabrant, D; Gillespie, B. W.; Jolliet, O (Mar 2009). "Apparent half-lives of dioxins, furans, and polychlorinated biphenyls as a function of age, body fat, smoking status, and breast-feeding". Environ Health Perspect. 117 (3): 417–25. doi:10.1289/ehp.11781. PMC 2661912
 . PMID 19337517.
. PMID 19337517. - ↑ Wittsiepe J.; et al. (2007). "Bioavailability of PCDD/F from contaminated soil in young Goettingen minipigs". Chemosphere. 67 (9): S355–S364. doi:10.1016/j.chemosphere.2006.05.129. PMID 17223170.
- ↑ Aylward LL; et al. (2005). "Exposure reconstruction for the TCDD-exposed NIOSH cohort study using a concentration- and age-dependent model of elimination". Risk Analysis. 25 (4): 945–956. doi:10.1111/j.1539-6924.2005.00645.x. PMID 16268942.
- ↑ Kimbrough R.D.; et al. (1977). "Epidemiology and pathology of a tetrachlorodibenzodioxin episode". Arch. Environ. Health. 32 (2): 77–86. doi:10.1080/00039896.1977.10667259. PMID 557961.
- ↑ "PCB contamination found on Upstate waste company's equipment". thestate.
- ↑ http://www.atsdr.cdc.gov/toxprofiles/tp17-c6.pdf
- ↑ "CATAWBA RIVER FISH CONSUMPTION ADVISORIES DRASTICALLY EXPANDED". catawbariverkeeper.org.
