Diethylstilbestrol
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | Oral, intravenous |
| ATC code | G03CB02 (WHO) G03CC05 (WHO), L02AA01 (WHO) |
| Identifiers | |
| |
| CAS Number |
56-53-1 |
| PubChem (CID) | 448537 |
| IUPHAR/BPS | 2801 |
| DrugBank |
DB00255 |
| ChemSpider |
395306 |
| UNII |
731DCA35BT |
| KEGG |
D00577 |
| ChEBI |
CHEBI:41922 |
| ChEMBL |
CHEMBL411 |
| ECHA InfoCard | 100.000.253 |
| Chemical and physical data | |
| Formula | C18H20O2 |
| Molar mass | 268.35 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Diethylstilbestrol (DES) (INN, USAN, BAN), also known formerly (and inappropriately) as stilboestrol (BAN), is a synthetic, non-steroidal estrogen of the stilbestrol group that was first synthesized in 1938.[1] It is also classified as an endocrine disruptor. Human exposure to DES occurred through diverse sources, such as dietary ingestion from supplemented cattle feed and medical treatment for certain conditions, including breast and prostate cancers. From about 1940 to 1971, DES was given to pregnant women in the mistaken belief it would reduce the risk of pregnancy complications and losses.
In 1971, DES was shown to cause clear cell carcinoma, a rare vaginal tumor in girls and women who had been exposed to this drug in utero. The United States Food and Drug Administration subsequently withdrew DES from use in pregnant women. Follow-up studies have indicated that DES also has the potential to cause a variety of significant adverse medical complications during the lifetimes of those exposed.[2] The United States National Cancer Institute recommends[3] women born to mothers who took DES undergo special medical exams on a regular basis to screen for complications as a result of the drug. Individuals who were exposed to DES during their mothers' pregnancies are commonly referred to as "DES daughters" and "DES sons".
Medical uses
DES has been used in the past for the following indications:
- Recurrent miscarriage in pregnancy
- Hormone replacement therapy for menopausal symptoms
- Hormone replacement therapy for hypoestrogenism (e.g., gonadal dysgenesis, premature ovarian failure, and after oophorectomy)
- Postpartum lactation suppression to prevent or reverse breast engorgement
- Atrophic vaginitis and gonorrheal vaginitis (the latter discontinued following the introduction of the antibiotic penicillin)
- Prostate cancer and breast cancer
- Prevention of tall stature in tall adolescent girls
- As an emergency postcoital contraceptive
Adverse effects
First generation
An estimated 3 million pregnant women in the USA were prescribed DES from 1941 through 1971.[4][5] DES was also widely prescribed to women in Canada, the UK, Europe, Australia, and New Zealand during a similar period. Women who were prescribed DES during pregnancy have been shown to have a modestly increased risk of breast cancer and breast cancer mortality.[6]
Second generation
DES daughters
DES gained notoriety when it was shown to cause a rare vaginal tumor in girls and young women who had been exposed to this drug in utero. In 1971, the New England Journal of Medicine published a report showing that seven of eight girls and young women (ages 14 to 22) who had been diagnosed with vaginal clear cell adenocarcinoma had been exposed prenatally to DES.[7] Subsequent studies have shown an approximate 40-fold increased risk of vaginal/cervical clear cell adenocarcinoma in women exposed in utero to DES. As a consequence of this evidence, DES is considered an established human carcinogen. DES was one of the first transplacental carcinogens discovered in humans, meaning a toxin could cross the placenta and harm the fetus. It had originally been believed that the placenta protected the developing fetus but it is now known that is not true. Daughters exposed to DES in utero may also have an increased risk of moderate to severe cervical squamous cell dysplasia and an increased risk of breast cancer.[8]
In addition to its carcinogenic properties, DES is a known teratogen, an agent capable of causing malformations in daughters and sons who were exposed in utero. DES-exposed daughters are at an increased risk of abnormalities of the reproductive tract, including vaginal epithelial changes such as vaginal adenosis (which means a type of cell normally found in the uterus, columnar cells, are also present in the vagina), an increased cervical transformation zone, and uterine abnormalities, such as T-shaped uterus. These anomalies contribute to an increased risk of infertility and adverse pregnancy outcomes in prenatally DES-exposed daughters. The most recent published research on DES daughters' adverse health outcomes documented by the U.S. National Cancer Institute (NCI) appears in the October 6, 2011 issue of the New England Journal of Medicine under the authorship of RN Hoover et al., and lists these adverse effects and risk factors: Cumulative risks in women exposed to DES, as compared with those not exposed, were as follows: for infertility, 33.3% vs. 15.5%; spontaneous abortion, 50.3% vs. 38.6%; preterm delivery, 53.3% vs. 17.8%; loss of second-trimester pregnancy, 16.4% vs. 1.7%; ectopic pregnancy, 14.6% vs. 2.9%; preeclampsia, 26.4% vs. 13.7%; stillbirth, 8.9% vs. 2.6%; early menopause, 5.1% vs. 1.7%; grade 2 or higher cervical intraepithelial neoplasia, 6.9% vs. 3.4%; and breast cancer at 40 years of age or older, 3.9% vs. 2.2%.[9] Daughters with prenatal exposure to DES may also have an increased risk of uterine fibroids, and incompetent cervix in adulthood.[10]
At least one published study by researchers specializing in psycho-sexual development has determined there is a positive association between in-utero DES exposure among DES daughters and increased potential for a girl being homosexual or bisexual.[11] However, later studies have concluded that "no clear-cut differences can be demonstrated to date between unexposed and DES-exposed women in gender-related behavior,"[12] and another found that "DES Daughters were slightly more likely than unexposed women to have ever been married and were less likely to report having had a same-sex sexual partner."[13] These studies contradict earlier studies indicating an inclination towards female attraction in DES daughters, as well as no indication for increased prevalence of gender-atypical behavior.
Studies of DES daughters have not found a link between in utero exposure to DES and autoimmune diseases.[14]
In an animal model designed to study environmental estrogens, DES turned out to be an obesogen capable of causing adult weight gain in female mice which had been exposed to DES during neonatal development. The excess weight gain was not apparent at birth or in infancy, but occurred in adulthood.[15][16]
DES sons
Initially, fewer studies documented risks of prenatal exposure to DES on males (referred to as "DES sons"). In the 1970s and early 1980s, studies published on prenatally DES-exposed males investigated increased risk of testicular cancer, infertility and urogenital abnormalities in development, such as cryptorchidism and hypospadias.[17][18] Research published in the U.S. by Palmer et al. in 2009 further confirmed evidence of these findings.[19] Additional research published in Finland in 2012 has further confirmed an increased risk of cryptorchidism among males exposed prenatally to DES.[20]
The U.S. Centers for Disease Control (CDC) has acknowledged the link between DES exposure and noncancerous epididymal cysts.[21]
The American Association of Clinical Endocrinologists (AACE) has documented that prenatal DES exposure in males is positively linked to a condition known as hypogonadism (low testosterone levels) that may require treatment with testosterone replacement therapy.[22]
One published study indicates males may have a greater likelihood of being left-handed than unexposed males, though this has not been subsequently confirmed.[13]
Research investigating the possible behavioral and psychosexual effects of prenatal DES exposure in human males occurred as early as 1973.[23] This research has centered on a long-standing question of whether prenatal exposure to DES in offspring of mothers who were prescribed DES may have included sexual orientation and gender-related behavioral effects and also physical intersex conditions.[24] Kaplan published the first-known medical study (1959) of intersex condition in a male prenatally-exposed to DES.[25] Several sources from medical literature in the 1970s and 1980s indicate that DES was used for treatment of male-to-female and female to male transsexual patients.[26][27][28]
The reference source Dictionary of Organic Compounds, 6th edition (1996) lists diethylstilbestrol (pp. 2175–76) as a non-steroidal estrogen with carcinogenic properties that "causes male impotence and transsexual changes, especially in offspring exposed in utero".[29]
There is some evidence linking prenatal hormonal influences on sexual orientation, gender identity and transsexual development, but this is an area of behavioral research that remains controversial.[30][31][32][33] Several published studies in the medical literature on psychoneuroendocrinology have examined the hypothesis that prenatal exposure to estrogens (including DES) may cause significant developmental impact on sexual differentiation of the brain, and on subsequent behavioral and gender identity development in exposed males and females. One of the leading investigators of this area of research is June Reinisch, former director of the Kinsey Institute for Research in Sex, Gender, and Reproduction.[34][35] Reinisch cited several cases of "male feminization" among prenatally DES-exposed males.
Dr. Scott Kerlin, a major DES research scientist and founder of the DES Sons International Research Network in 1996, has documented for the past 20 years a high prevalence of individuals with confirmed prenatal DES exposure who self-identify as male-to-female transsexual, transgender, or have intersex conditions, and many individuals who report a history of experiencing difficulties with gender dysphoria.[36][37][38][39]
A large US study, in which recruitment was not dependent on health concerns, and in which DES exposure (or lack of exposure) was confirmed for all participants, found The OR (odds ratio) for exposed men having had a same-sex sexual partner was 1.3[13] for DES-exposed men compared to unexposed men. However, no research into gender identity issues was explored in this study.[13]
Various neurological changes occur after prenatal exposure of embryonic males to DES and other estrogenic endocrine disrupters. Animals that exhibited these structural neurological changes were also shown to demonstrate various gender-related behavioral changes (so-called "feminization of males").
Psychological anomalies
Most of the initial research documenting the psychological effects of prenatal DES exposure was poorly conducted, often by mail card. Despite that, some more carefully conducted studies show a clear link to depression.,[40][41] and a more recent French study asserts that there was an 83% increase in psychological disorders for offspring that were prenatally exposed to DES.[42]
Third generation
Current research also looks at DES in the third generation. These are the children of men and women who were exposed to DES in utero; thus, they are also the grandchildren of women who were given DES during pregnancy. Studies of the third generation are important because DES might be associated with epigenetic changes, which involve changes to the way genes behave (not involving the DNA itself) that may be heritable from one generation to another. If epigenetic changes occur and are heritable, studies of the DES-exposed third generation have implications for the influence of environmental endocrine disruptors on human health and evolution.
Recent studies from the US National Cancer Institute (NCI) show that the daughters of women who were exposed in utero to DES may be less likely than the unexposed to have regular menstrual periods.[43] A possible increased risk of infertility in the older, third generation daughters was also noted. The NCI study provides limited evidence of an increased risk of birth defects in the sons or daughters of women who were exposed prenatally to DES. An increased risk of ovarian cancer in the daughters of women exposed in utero was observed, but it was based on three cases of almost 800, so the finding is considered preliminary and requires further study.
Some evidence suggests the sons of prenatally DES-exposed women might have an increased risk of hypospadias,[44][45] but other studies suggest the increase in risk might not be as great as once thought.[46]
Pharmacology
Pharmacodynamics
Estrogenic activity
DES is a very potent full agonist of the estrogen receptors (ERs).[47][48] It has approximately 468% and 295% of the affinity of estradiol at the ERα and ERβ, respectively.[49] However, EC50 values of 0.18 nM and 0.06 nM of DES for the ERα and ERβ, respectively, have been reported, suggesting, in spite of its binding affinity for the two receptors, several-fold preference for activation of the ERβ over the ERα.[50]
| Estrogen | Hot flashes | FSH | HDL cholesterol | SHBG | CBG | Angiotensinogen | |||
|---|---|---|---|---|---|---|---|---|---|
| Estradiol | 100 | 100 | 100 | 100 | 100 | 100 | |||
| Estriol | 30 | 30 | 20 | ? | ? | ? | |||
| Estrone sulfate | ? | 90 | 50 | 90 | 70 | 150 | |||
| CEEs | 120 | 110 | 150 | 300 | 150 | 500 | |||
| Equilin sulfate | ? | ? | 600 | 750 | 600 | 750 | |||
| Ethinyl estradiol | 12,000 | 12,000 | 40,000 | 50,000 | 60,000 | 35,000 | |||
| Diethylstilbestrol | ? | 340 | ? | 2,560 | 2,450 | 1,950 | |||
| Hot flashes = clinical relief of hot flashes; FSH = suppression of FSH levels; HDL cholesterol, SHBG, CBG, and angiotensinogen = increase in the serum levels of these hepatic proteins. | |||||||||
As can be seen in the table above, similarly to ethinyl estradiol, DES shows a marked and disproportionately strong effect on hepatic protein production.[51]
Other activities
DES has been identified as an antagonist of all three isotypes of the estrogen-related receptors (ERRs), the ERRα, ERRβ, and ERRγ.[52]
In addition to the ERs, an in vitro study found that DES also possesses activity, albeit relatively weak, at a variety of other steroid hormone receptors.[50] Whereas the study found EC50 values of 0.18 nM and 0.06 nM of DES for the ERα and ERβ, respectively, the drug showed significant glucocorticoid activity at a concentration of 1 μm that surpassed that of 0.1 nM dexamethasone as well as significant antagonism of the androgen, progesterone, and mineralocorticoid receptors (75%, 85%, and 50% inhibition of positive control stimulation, respectively, at a concentration of 1 μm).[50] It also showed approximately 25% inhibition of the activation of PPARγ and LXRα at a concentration of 10 μm.[50] The researchers stated that, to the best of their knowledge, they were the first to report such actions of DES, and hypothesized that these actions could be involved in the clinical effects of DES, for instance, in prostate cancer (notably in which particularly high dosages of DES are employed).[50] However, they also noted that the importance of the activities requires further study in animal models at pharmacologically relevant doses.[50]
Pharmacokinetics
DES is known to produce paroxypropione as a metabolite.[53]
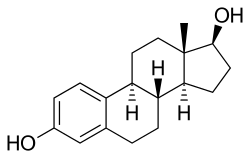
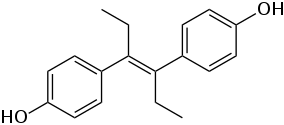
Chemistry
DES belongs to the stilbestrol (4,4'-dihydroxystilbene) group of compounds.[54] It is a non-steroidal open-ring analogue of the steroidal estrogen estradiol.[55] DES was derived from the naturally occurring compound anethole, a weakly estrogenic constituent of anise and fennel.[54][56][57][58] Anethole was demethylated to form anol and anol then spontaneously dimerized into dianol and hexestrol, with DES subsequently being synthesized via structural modification of hexestrol.[54][56][57][58] It has been determined via X-ray crystallography that the molecular dimensions of DES are almost identical to those of estradiol, particularly in regards to the distance between the hydroxyl groups at either end of the molecules.[58]
History
Synthesis
DES was first synthesized in early 1938 by Leon Golberg, then a graduate student of Sir Robert Robinson at the Dyson Perrins Laboratory at the University of Oxford. Golberg's research was based on work by Wilfrid Lawson at the Courtauld Institute of Biochemistry, (led by Sir Edward Charles Dodds at Middlesex Hospital Medical School now part of University College London). A report of its synthesis was published in Nature on 5 February 1938.[59][60][61]
DES research was funded by the UK Medical Research Council (MRC), which had a policy against patenting drugs discovered using public funds. Because it was not patented, DES was produced by more than 200 pharmaceutical and chemical companies worldwide.
Clinical use
DES (in tablets up to 5 mg) was approved by the United States Food and Drug Administration (FDA) on September 19, 1941 for four indications: gonorrheal vaginitis, atrophic vaginitis, menopausal symptoms, and postpartum lactation suppression to prevent breast engorgement.[61] The gonorrheal vaginitis indication was dropped when the antibiotic penicillin became available. From its very inception, the drug was highly controversial.[62][63]
In 1941, Charles Huggins and Clarence Hodges at the University of Chicago found DES to be the first effective drug for the treatment of metastatic prostate cancer.[64][65]
Orchiectomy or DES or both were the standard initial treatment for symptomatic advanced prostate cancer for over 40 years, until the GnRH agonist leuprolide was found to have efficacy similar to DES without estrogenic effects and was approved in 1985.[66]
From the 1940s until the late 1980s, DES was FDA-approved as estrogen-replacement therapy for estrogen deficiency states such as ovarian dysgenesis, premature ovarian failure, and after oophorectomy.
In the 1940s, DES was used off-label to prevent adverse pregnancy outcomes in women with a history of miscarriage. On July 1, 1947, the FDA approved the use of DES for this indication. The first such approval was granted to Bristol-Myers Squibb, allowing use of 25 mg (and later 100 mg) tablets of DES during pregnancy. Approvals were granted to other pharmaceutical companies later in the same year.[67] The recommended regimen started at 5 mg per day in the seventh and eighth weeks of pregnancy (from first day of last menstrual period), increased every other week by 5 mg per day through the 14th week, and then increased every week by 5 mg per day from 25 mg per day in the 15th week to 125 mg per day in the 35th week of pregnancy.[68] DES was originally considered effective and safe for both the pregnant woman and the developing baby. It was aggressively marketed and routinely prescribed. Sales peaked in 1953.
In the early 1950s, a double-blind clinical trial at the University of Chicago assessed pregnancy outcomes in women who were assigned to either receive or not receive DES.[69] The study showed no benefit of taking DES during pregnancy; adverse pregnancy outcomes were not reduced in the women who were given DES. By the late 1960s, six of seven leading textbooks of obstetrics said DES was ineffective at preventing miscarriage.[67][70]
Despite an absence of evidence supporting the use of DES to prevent adverse pregnancy outcomes, DES continued to be given to pregnant women through the 1960s. In 1971, a report published in the New England Journal of Medicine showed a probable link between DES and vaginal clear cell adenocarcinoma in girls and young women who had been exposed to this drug in utero. Later in the same year, the FDA sent an FDA Drug Bulletin to all U.S. physicians advising against the use of DES in pregnant women. The FDA also removed prevention of miscarriage as an indication for DES use and added pregnancy as a contraindication for DES use.[71] On February 5, 1975, the FDA ordered 25 mg and 100 mg tablets of DES withdrawn, effective February 18, 1975.[72] The number of persons exposed to DES during pregnancy or in utero during 1940–1971 is unknown, but may be as high as 2 million in the United States. DES was also used in other countries, most notably France, the Netherlands, and Great Britain.
From the 1950s through the beginning of the 1970s, DES was prescribed to prepubescent girls to begin puberty and thus stop growth by closing growth plates in the bones. Despite its clear link to cancer, doctors continued to recommend the hormone for "excess height".[73]
In 1960, DES was found to be more effective than androgens in the treatment of advanced breast cancer in postmenopausal women.[74] DES was the hormonal treatment of choice for advanced breast cancer in postmenopausal women until 1977, when the FDA approved tamoxifen, a selective estrogen receptor modulator with efficacy similar to DES but fewer side effects.[75]
In 1973, in an attempt to restrict off-label use of DES as a postcoital contraceptive (which had become prevalent at many university health services following publication of an influential study in 1971 in JAMA) to emergency situations such as rape, an FDA Drug Bulletin was sent to all U.S. physicians and pharmacists that said the FDA had approved, under restricted conditions, postcoital contraceptive use of DES.[76]
In 1975, the FDA said it had not actually given (and never did give) approval to any manufacturer to market DES as a postcoital contraceptive, but would approve that indication for emergency situations such as rape or incest if a manufacturer provided patient labeling and special packaging as set out in a FDA final rule published in 1975.[77] To discourage off-label use of DES as a postcoital contraceptive, the FDA in 1975 removed DES 25 mg tablets from the market and ordered the labeling of lower doses (5 mg and lower) of DES still approved for other indications changed to state: "This drug product should not be used as a postcoital contraceptive" in block capital letters on the first line of the physician prescribing information package insert and in a prominent and conspicuous location of the container and carton label.[72][78] In the 1980s, off-label use of the Yuzpe regimen of certain regular combined oral contraceptive pills superseded off-label use of DES as a postcoital contraceptive.[79]
In 1978, the FDA removed postpartum lactation suppression to prevent breast engorgement from their approved indications for DES and other estrogens.[80] In the 1990s, the only approved indications for DES were treatment of advanced prostate cancer and treatment of advanced breast cancer in postmenopausal women. The last remaining U.S. manufacturer of DES, Eli Lilly, stopped making and marketing it in 1997.
Lawsuits
In the 1970s, the negative publicity surrounding the discovery of DES's long-term effects resulted in a huge wave of lawsuits in the United States against its manufacturers. These culminated in a landmark 1980 decision of the Supreme Court of California, Sindell v. Abbott Laboratories, in which the court imposed a rebuttable presumption of market share liability upon all DES manufacturers, proportional to their share of the market at the time the drug was consumed by the mother of a particular plaintiff.
A lawsuit was filed in Boston Federal Court by 53 DES daughters who say their breast cancers were the result of DES being prescribed to their mothers while pregnant with them. Their cases survived a Daubert hearing. In 2013, the Fecho sisters who initiated the breast cancer/DES link litigation agreed to an undisclosed settlement amount on the second day of trial. The remaining litigants have received various settlements.[81]
Society and culture
Alan Turing, the ground breaking cryptographer, was placed on the medication to induce chemical castration as a treatment for his homosexuality shortly before he committed suicide.[82]
Veterinary use
Female canine incontinence
DES has been very successful in treating female canine incontinence stemming from poor sphincter control. It is still available from compounding pharmacies, and at the low (1 mg) dose, does not have the carcinogenic properties that were so problematic in humans.[83] It is generally administered once a day for seven to ten days and then once every week as needed.
Growth promotion in livestock
The greatest usage of DES was in the livestock industry, used to improve feed conversion in beef and poultry. During the 1960s, DES was used as a growth hormone in the beef and poultry industries. It was later found to cause cancer by 1971, but was not phased out until 1979.[84][85] When DES was discovered to be harmful to humans, it was moved to veterinary use.
References
- ↑ Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 396–. ISBN 978-1-4757-2085-3.
- ↑ "DES Update: For Consumers". United States Department of Health and Human Services: Centers for Disease Control and Prevention. Retrieved 2011-06-30.
- ↑ "DES: Questions and Answers". FactSheet. National Cancer Institute. Retrieved 2011-06-30.
- ↑ "Problems in Research: Regulations—The Diethylstilbestrol Tragedy". The Medical Bag. 12 April 2013. Retrieved 29 April 2014.
- ↑ Hammes B, Laitman CJ (Jan–Feb 2003). "Diethylstilbestrol (DES) update: recommendations for the identification and management of DES-exposed individuals". Journal of Midwifery & Women's Health. 48 (1): 19–29. doi:10.1016/s1526-9523(02)00370-7. PMID 12589302.
- ↑ Palmer JR, Wise LA, Hatch EE, Troisi R, Titus-Ernstoff L, Strohsnitter W, Kaufman R, Herbst AL, Noller KL, Hyer M, Hoover RN (August 2006). "Prenatal diethylstilbestrol exposure and risk of breast cancer" (PDF). Cancer Epidemiology, Biomarkers & Prevention. 15 (8): 1509–14. doi:10.1158/1055-9965.EPI-06-0109. PMID 16896041.
- ↑ Herbst AL, Ulfelder H, Poskanzer DC (April 1971). "Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women". The New England Journal of Medicine. 284 (15): 878–81. doi:10.1056/NEJM197104222841604. PMID 5549830.
- ↑ Troisi R, Hatch EE, Titus-Ernstoff L, Hyer M, Palmer JR, Robboy SJ, Strohsnitter WC, Kaufman R, Herbst AL, Hoover RN (July 2007). "Cancer risk in women prenatally exposed to diethylstilbestrol". International Journal of Cancer. 121 (2): 356–60. doi:10.1002/ijc.22631. PMID 17390375.
- ↑ Hoover RN, Hyer M, Pfeiffer RM, Adam E, Bond B, Cheville AL, Colton T, Hartge P, Hatch EE, Herbst AL, Karlan BY, Kaufman R, Noller KL, Palmer JR, Robboy SJ, Saal RC, Strohsnitter W, Titus-Ernstoff L, Troisi R (October 2011). "Adverse health outcomes in women exposed in utero to diethylstilbestrol". The New England Journal of Medicine. 365 (14): 1304–14. doi:10.1056/NEJMoa1013961. PMID 21991952.
- ↑ Office of Research on Women’s Health, NIH, DHHS (March 2006). "Status of Research on Uterine Fibroids (leiomyomata uteri) at the National Institutes of Health" (PDF). United States National Institutes of Health.
- ↑ Ehrhardt AA, Meyer-Bahlburg HF, Rosen LR, Feldman JF, Veridiano NP, Zimmerman I, McEwen BS (February 1985). "Sexual orientation after prenatal exposure to exogenous estrogen". Archives of Sexual Behavior. 14 (1): 57–77. doi:10.1007/BF0154135 (inactive 2015-01-01). PMID 3977584.
- ↑ Newbold RR (August 1993). "Gender-related behavior in women exposed prenatally to diethylstilbestrol". Environmental Health Perspectives. 101 (3): 208–13. doi:10.1289/ehp.93101208. PMC 1519765
 . PMID 8404755.
. PMID 8404755. - 1 2 3 4 Titus-Ernstoff L, Perez K, Hatch EE, Troisi R, Palmer JR, Hartge P, Hyer M, Kaufman R, Adam E, Strohsnitter W, Noller K, Pickett KE, Hoover R (March 2003). "Psychosexual characteristics of men and women exposed prenatally to diethylstilbestrol". Epidemiology. 14 (2): 155–60. doi:10.1097/01.EDE.0000039059.38824.B2. PMID 12606880.
- ↑ Strohsnitter WC, Noller KL, Troisi R, Robboy SJ, Hatch EE, Titus-Ernstoff L, Kaufman RH, Palmer JR, Anderson D, Hoover RN (October 2010). "Autoimmune disease incidence among women prenatally exposed to diethylstilbestrol". The Journal of Rheumatology. 37 (10): 2167–73. doi:10.3899/jrheum.091092. PMC 2988471
 . PMID 20634240.
. PMID 20634240. - ↑ Newbold RR, Padilla-Banks E, Snyder RJ, Jefferson WN (July 2007). "Perinatal exposure to environmental estrogens and the development of obesity". Molecular Nutrition & Food Research. 51 (7): 912–7. doi:10.1002/mnfr.200600259. PMID 17604389.
- ↑ Newbold RR, Padilla-Banks E, Snyder RJ, Phillips TM, Jefferson WN (2007). "Developmental exposure to endocrine disruptors and the obesity epidemic". Reproductive Toxicology. 23 (3): 290–6. doi:10.1016/j.reprotox.2006.12.010. PMC 1931509
 . PMID 17321108.
. PMID 17321108. - ↑ Henderson BE, Benton B, Cosgrove M, Baptista J, Aldrich J, Townsend D, Hart W, Mack TM (October 1976). "Urogenital tract abnormalities in sons of women treated with diethylstilbestrol". Pediatrics. 58 (4): 505–7. PMID 972792.
- ↑ Gill WB, Schumacher GF, Bibbo M, Straus FH, Schoenberg HW (July 1979). "Association of diethylstilbestrol exposure in utero with cryptorchidism, testicular hypoplasia and semen abnormalities". The Journal of Urology. 122 (1): 36–9. PMID 37351.
- ↑ Palmer JR, Herbst AL, Noller KL, Boggs DA, Troisi R, Titus-Ernstoff L, Hatch EE, Wise LA, Strohsnitter WC, Hoover RN (August 2009). "Urogenital abnormalities in men exposed to diethylstilbestrol in utero: a cohort study". Environmental Health. 8: 37. doi:10.1186/1476-069X-8-37. PMC 2739506
 . PMID 19689815.
. PMID 19689815. - ↑ Virtanen HE, Adamsson A (May 2012). "Cryptorchidism and endocrine disrupting chemicals". Molecular and Cellular Endocrinology. 355 (2): 208–20. doi:10.1016/j.mce.2011.11.015. PMID 22127307.
- ↑ "Known Health Effects for DES Sons". United States Department of Health and Human Services: Centers for Disease Control and Prevention. Retrieved 2011-06-30.
- ↑ "American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Evaluation and Treatment of Hypogonadism in Adult-Male Patients--2002 Update" (PDF). American Association of Clinical Endocrinologists.
- ↑ Yalom ID, Green R, Fisk N (April 1973). "Prenatal exposure to female hormones. Effect on psychosexual development in boys". Archives of General Psychiatry. 28 (4): 554–61. PMID 4734959.
- ↑ Hines M (April 2011). "Prenatal endocrine influences on sexual orientation and on sexually differentiated childhood behavior". Frontiers in Neuroendocrinology. 32 (2): 170–82. doi:10.1016/j.yfrne.2011.02.006. PMC 3296090
 . PMID 21333673.
. PMID 21333673. - ↑ Kaplan NM (September 1959). "Male pseudohermaphrodism: report of a case, with observations on pathogenesis". The New England Journal of Medicine. 261: 641–4. doi:10.1056/NEJM195909242611303. PMID 14404413.
- ↑ Goodwin WE, Cummings RH (March 1984). "Squamous metaplasia of the verumontanum with obstruction due to hypertrophy: long-term effects of estrogen on the prostate in an aging male-to-female transsexual". The Journal of Urology. 131 (3): 553–4. PMID 6199525.
- ↑ Lehrman KL (February 1976). "Pulmonary embolism in a transsexual man taking diethylstilbestrol". Jama. 235 (5): 532–3. PMID 946104.
- ↑ Seyler LE, Canalis E, Spare S, Reichlin S (July 1978). "Abnormal gonadotropin secretory responses to LRH in transsexual women after diethylstilbestrol priming". The Journal of Clinical Endocrinology and Metabolism. 47 (1): 176–83. doi:10.1210/jcem-47-1-176. PMID 122396.
- ↑ Buckingham J, and MacDonald F (1995). Dictionary of Organic Compounds, 6th edition. Chapman and Hall/CRC. pp. 2175–76. ISBN 9780849300073.
- ↑ Michel A, Mormont C, Legros JJ (October 2001). "A psycho-endocrinological overview of transsexualism". European Journal of Endocrinology. 145 (4): 365–76. doi:10.1530/eje.0.1450365. PMID 11580991.
- ↑ Selvaggi G, Ceulemans P, De Cuypere G, VanLanduyt K, Blondeel P, Hamdi M, Bowman C, Monstrey S (November 2005). "Gender identity disorder: general overview and surgical treatment for vaginoplasty in male-to-female transsexuals" (PDF). Plastic and Reconstructive Surgery. 116 (6): 135e–145e. doi:10.1097/01.prs.0000185999.71439.06. PMID 16267416.
- ↑ Dingfelder S (2004). "Gender Bender: New Research Suggests Genes and Prenatal Hormones Could Have More Sway in Gender Identity than Previously Thought". APA Monitor on Psychology. 35 (4): 48.
- ↑ Hood E (October 2005). "Are EDCs blurring issues of gender?". Environmental Health Perspectives. 113 (10): A670–7. PMC 1281309
 . PMID 16203228.
. PMID 16203228. - ↑ Reinisch JM, Ziemba-Davis M, Sanders SA (1991). "Hormonal contributions to sexually dimorphic behavioral development in humans". Psychoneuroendocrinology. 16 (1-3): 213–78. doi:10.1016/0306-4530(91)90080-D. PMID 1961841.
- ↑ Yalom ID, Green R, Fisk N (April 1973). "Prenatal exposure to female hormones. Effect on psychosexual development in boys". Archives of General Psychiatry. 28 (4): 554–61. doi:10.1001/archpsyc.1973.01750340080013. PMID 4734959.
- ↑ Hood E (October 2005). "Are EDCs blurring issues of gender?". Environmental Health Perspectives. 113 (10): A670–7. doi:10.1289/ehp.113-a670. PMC 1281309
 . PMID 16203228.
. PMID 16203228. - ↑ Blackless M, Besser M, Carr S, Cohen-Kettenis PT, Connolly P, De Sutter P, Diamond M, Di Ceglie D, Higashi Y, Jones L, Kruijver FP, Martin J, Playdon ZJ, Ralph D, Reed T, Reid R, Reiner WG, Swaab D, Terry T, Wilson P, Wylie K (2006). "Atypical Gender Development – A Review". International Journal of Transgenderism. 9 (1): 29–44. doi:10.1300/J485v09n01_04.
- ↑ Rudacille D (2005). The Riddle of Gender (Chapter, "Fear of a Pink Planet"). Pantheon Books. pp. 240–276. ISBN 0-375-42162-9.
- ↑ Bao AM, Swaab DF (April 2011). "Sexual differentiation of the human brain: relation to gender identity, sexual orientation and neuropsychiatric disorders". Frontiers in Neuroendocrinology. 32 (2): 214–26. doi:10.1016/j.yfrne.2011.02.007. PMID 21334362.
- ↑ Pillard RC, Rosen LR, Meyer-Bahlburg H, Weinrich JD, Feldman JF, Gruen R, Ehrhardt AA (1993). "Psychopathology and social functioning in men prenatally exposed to diethylstilbestrol (DES)". Psychosomatic Medicine. 55 (6): 485–91. doi:10.1097/00006842-199311000-00003. PMID 8310108.
- ↑ O'Reilly EJ, Mirzaei F, Forman MR, Ascherio A (April 2010). "Diethylstilbestrol exposure in utero and depression in women". American Journal of Epidemiology. 171 (8): 876–82. doi:10.1093/aje/kwq023. PMC 2877444
 . PMID 20332145.
. PMID 20332145. - ↑ Soyer-Gobillard MO, Paris F, Gaspari L, Courtet P, Sultan C (2016). "Association between fetal DES-exposure and psychiatric disorders in adolescence/adulthood: evidence from a French cohort of 1002 prenatally exposed children". Gynecological Endocrinology. 32 (1): 25–9. doi:10.3109/09513590.2015.1063604. PMID 26172930.
- ↑ Titus-Ernstoff L, Troisi R, Hatch EE, Wise LA, Palmer J, Hyer M, Kaufman R, Adam E, Strohsnitter W, Noller K, Herbst AL, Gibson-Chambers J, Hartge P, Hoover RN (August 2006). "Menstrual and reproductive characteristics of women whose mothers were exposed in utero to diethylstilbestrol (DES)" (PDF). International Journal of Epidemiology. 35 (4): 862–8. doi:10.1093/ije/dyl106. PMID 16723367.
- ↑ Klip H, Verloop J, van Gool JD, Koster ME, Burger CW, van Leeuwen FE (March 2002). "Hypospadias in sons of women exposed to diethylstilbestrol in utero: a cohort study". Lancet. 359 (9312): 1102–7. doi:10.1016/S0140-6736(02)08152-7. PMID 11943257.
- ↑ Kalfa N, Paris F, Soyer-Gobillard MO, Daures JP, Sultan C (June 2011). "Prevalence of hypospadias in grandsons of women exposed to diethylstilbestrol during pregnancy: a multigenerational national cohort study". Fertility and Sterility. 95 (8): 2574–7. doi:10.1016/j.fertnstert.2011.02.047. PMID 21458804.
- ↑ Brouwers MM, Feitz WF, Roelofs LA, Kiemeney LA, de Gier RP, Roeleveld N (March 2006). "Hypospadias: a transgenerational effect of diethylstilbestrol?". Human Reproduction. 21 (3): 666–9. doi:10.1093/humrep/dei398. PMID 16293648.
- ↑ Jordan VC (2013). Estrogen Action, Selective Estrogen Receptor Modulators, and Women's Health: Progress and Promise. World Scientific. pp. 143–. ISBN 978-1-84816-958-6.
- ↑ Seiler JP, Autrup JL, Autrup H (6 December 2012). Diversification in Toxicology — Man and Environment: Proceedings of the 1997 EUROTOX Congress Meeting Held in Århus, Denmark, June 25–28, 1997. Springer Science & Business Media. pp. 23–. ISBN 978-3-642-46856-8.
- ↑ Kuiper GG, Carlsson B, Grandien K, Enmark E, Häggblad J, Nilsson S, Gustafsson JA (March 1997). "Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta". Endocrinology. 138 (3): 863–70. doi:10.1210/endo.138.3.4979. PMID 9048584.
- 1 2 3 4 5 6 Coss CC, Jones A, Parke DN, Narayanan R, Barrett CM, Kearbey JD, Veverka KA, Miller DD, Morton RA, Steiner MS, Dalton JT (March 2012). "Preclinical characterization of a novel diphenyl benzamide selective ERα agonist for hormone therapy in prostate cancer". Endocrinology. 153 (3): 1070–81. doi:10.1210/en.2011-1608. PMID 22294742.
- 1 2 Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947.
- ↑ Greschik H, Flaig R, Renaud JP, Moras D (August 2004). "Structural basis for the deactivation of the estrogen-related receptor gamma by diethylstilbestrol or 4-hydroxytamoxifen and determinants of selectivity". The Journal of Biological Chemistry. 279 (32): 33639–46. doi:10.1074/jbc.M402195200. PMID 15161930.
- ↑ Chambers P, Günzel P (12 March 2013). Mechanism of Toxic Action on Some Target Organs: Drugs and Other Substances. Springer Science & Business Media. pp. 276–. ISBN 978-3-642-67265-1.
- 1 2 3 Vitamins and Hormones. Academic Press. 1945. pp. 233–. ISBN 978-0-08-086600-0.
- ↑ Wermuth CG, Aldous D, Raboisson P, Rognan D, eds. (1 July 2015). The Practice of Medicinal Chemistry. Elsevier Science. pp. 244–245. ISBN 978-0-12-417213-5.
- 1 2 Maximov PY, McDaniel RE, Jordan VC (23 July 2013). Tamoxifen: Pioneering Medicine in Breast Cancer. Springer Science & Business Media. pp. 3–. ISBN 978-3-0348-0664-0.
- 1 2 Ravina E (11 January 2011). T he Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. pp. 177–. ISBN 978-3-527-32669-3.
- 1 2 3 Sneader W (31 October 2005). Drug Discovery: A History. John Wiley & Sons. pp. 196–197. ISBN 978-0-470-01552-0.
- ↑ Dodds EC, Goldberg L, Lawson W, Robinson R (1938). "Estrogenic activity of certain synthetic compounds". Nature. 141 (3562): 247–8. doi:10.1038/141247b0.
- ↑ Dodds EC (1957). Biochemical contributions to endocrinology; experiments in hormonal research. Stanford: Stanford University Press. OCLC 1483899.
- 1 2 Meyers R (1983). D.E.S., the bitter pill. New York: Seaview/Putnam. ISBN 0-399-31008-8.
- ↑ Langston N (2010). Toxic bodies: Hormone disruptors and the legacy of DES. New Haven, CT: Yale University Press. ISBN 978-0-300-13607-4.
- ↑ Seaman B (2003). The greatest experiment ever performed on women: Exploding the estrogen myth. New York: Hyperion. ISBN 978-0-7868-6853-7.
- ↑ Huggins C, Hodges CV (1972). "Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate". CA. 22 (4): 232–40. doi:10.3322/canjclin.22.4.232. PMID 4625049.
- ↑ "Prostate cancer yields to a drug". The New York Times: 29. 1943.
- ↑ The Leuprolide Study Group (November 1984). "Leuprolide versus diethylstilbestrol for metastatic prostate cancer.". The New England Journal of Medicine. 311 (20): 1281–6. doi:10.1056/NEJM198411153112004. PMID 6436700.
- 1 2 Dutton DB (1988). Worse than the disease: pitfalls of medical progress. Cambridge: Cambridge University Press. ISBN 0-521-34023-3.
- ↑ Physicians' desk reference to pharmaceutical specialties and biologicals (15th ed.). Oradell NJ: Medical Economics. 1961. p. 625. ISBN 0-00-093447-X.
- ↑ Dieckmann WJ, Davis ME, Rynkiewicz LM, Pottinger RE (November 1953). "Does the administration of diethylstilbestrol during pregnancy have therapeutic value?". American Journal of Obstetrics and Gynecology. 66 (5): 1062–81. PMID 13104505.
- ↑ Apfel RJ, Fisher SM (1984). To do no harm: DES and the dilemmas of modern medicine. New Haven: Yale University Press. ISBN 0-300-03192-0.
- ↑ United States Food and Drug Administration (1971). "Certain estrogens for oral or parenteral use. Drugs for human use; drug efficacy study implementation". Fed Regist. 36 (217): 21537–8.; 36 FR 21537
- 1 2 FDA (1975). "Certain estrogens for oral use. Notice of withdrawal of approval of new drug applications". Fed Regist. 40 (25): 5384.; 25 FR 5384
- ↑ Zuger A (2009-07-27). "At What Height, Happiness? A Medical Tale". The New York Times. NY Times.
- ↑ Council on Drugs (1960). "Androgens and estrogens in the treatment of disseminated mammary carcinoma: retrospective study of nine hundred forty-four patients". JAMA. 172 (12): 1271–83. doi:10.1001/jama.1960.03020120049010.
- ↑ Ingle JN, Ahmann DL, Green SJ, Edmonson JH, Bisel HF, Kvols LK, Nichols WC, Creagan ET, Hahn RG, Rubin J, Frytak S (January 1981). "Randomized clinical trial of diethylstilbestrol versus tamoxifen in postmenopausal women with advanced breast cancer". The New England Journal of Medicine. 304 (1): 16–21. doi:10.1056/NEJM198101013040104. PMID 7001242.
- ↑ Kuchera LK (October 1971). "Postcoital contraception with diethylstilbestrol". Jama. 218 (4): 562–3. doi:10.1001/jama.218.4.562. PMID 5171004.
- ↑ FDA (1975). "Diethylstilbestrol as posticoital oral contraceptive; patient labeling". Fed Regist. 40 (25): 5451–5.; 40 FR 5451
- ↑ FDA (1975). "Estrogens for oral or parenteral use. Drugs for human use; drug efficacy study; amended notice". Fed Regist. 40 (39): 8242.; 39 FR 8242
- ↑ Hatcher RA, Stewart GK, Stewart F, Guest F, Josephs N, Dale J (1982). Contraceptive Technology 1982–1983. New York: Irvington Publishers. pp. 152–7. ISBN 0-8290-0705-9.
- ↑ FDA (1978). "Estrogens for postpartum breast engorgement". Fed Regist. 43 (206): 49564–7.; 43 FR 49564
- ↑ LAVOIE, DENISE (9 January 2013). "DES Pregnancy Drug Lawsuit: Settlement Reached Between Melnick Sisters And Eli Lilly And Co.". Huffington Post. Retrieved 19 March 2014.
- ↑ West-Taylor Z. "The Alan Turing Law – a Formal Pardon for Unpardonable Homophobia". Affinity magazine. Retrieved 3 December 2016.
- ↑ "Urinary Incontinence". Merck Veterinary Manual. Merck Veterinary Manual. Retrieved 30 November 2012.
- ↑ Harris RM, Waring RH (June 2012). "Diethylstilboestrol--a long-term legacy". Maturitas. 72 (2): 108–12. doi:10.1016/j.maturitas.2012.03.002. PMID 22464649.
- ↑ Gandhi R, Snedeker S (2000-06-01). "Consumer Concerns About Hormones in Food". Fact Sheet #37, June 2000. Program on Breast Cancer and Environmental Risk Factors, Cornell University. Retrieved 2011-07-20.
External links
- National Cancer Institute DES information
- DES Update from the U.S. Centers for Disease Control and Prevention
- DES Action USA national consumer organization providing comprehensive information for DES-exposed individuals
- DES Booklets from the U.S. National Institutes of Health (circa 1980)
- DES Follow-up Study National Cancer Institute's longterm study of DES-exposed persons (including the DES-AD Project)
- University of Chicago DES Registry of patients with CCA (clear cell adenocarcinoma) of the vagina and/or cervix.
- DES Diethylstilbestrol Provides resources and social media links for general DES awareness