Dexamethasone suppression test
| Dexamethasone suppression test | |
|---|---|
| Diagnostics | |
 |
| proopiomelanocortin derivatives | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| POMC | |||||||||
| γ-MSH | ACTH | β-lipotropin | |||||||
| α-MSH | CLIP | γ-lipotropin | β-endorphin | ||||||
| β-MSH | |||||||||
The dexamethasone suppression test (DST) is used to assess adrenal gland function by measuring how cortisol levels change in response to an injection of dexamethasone.[1] It is typically used to diagnose Cushing's syndrome.
The DST was historically used for diagnosing depression, but by 1988 it was considered to be "at best, severely limited in its clinical ability" for this purpose.[2]
Physiology
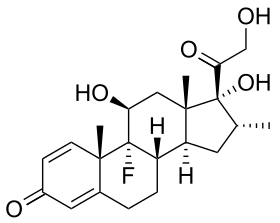
Dexamethasone is an exogenous steroid that provides negative feedback to the pituitary gland to suppress the secretion of adrenocorticotropic hormone (ACTH). Specifically, dexamethasone binds to glucocorticoid receptors in the anterior pituitary gland, which lie outside the blood–brain barrier, resulting in regulatory modulation.[3]
Interpretation
Low-dose and high-dose variations of the test exist.[4] The test is given at low (usually 1–2 mg) and high (8 mg) doses of dexamethasone, and the levels of cortisol are measured to obtain the results.[1]
A low dose of dexamethasone suppresses cortisol in individuals with no pathology in endogenous cortisol production. A high dose of dexamethasone exerts negative feedback on pituitary ACTH-producing cells, but not on ectopic ACTH-producing cells or adrenal adenoma.
Dose
A normal result is a decrease in cortisol levels upon administration of low-dose dexamethasone. Results indicative of Cushing's disease involve no change in cortisol on low-dose dexamethasone, but inhibition of cortisol on high-dose dexamethasone. If the cortisol levels are unchanged by low- and high-dose dexamethasone, then other causes of Cushing's syndrome must be considered with further work-up necessary. After the high-dose dexamethasone, it may be possible to make further interpretations.[5]
| ACTH† | Cortisol | Interpretation |
|---|---|---|
| Undetectable or low | is not suppressed by high or low doses | Primary hypercortisolism is likely; Cushing's syndrome, not disease (i.e. the hypercortisolism is not driven by ACTH hypersecretion) |
| Elevated in hundreds | is not suppressed by high or low doses | Ectopic ACTH syndrome is likely. If an adrenal tumor is not apparent, a chest CT and abdominal CT is indicated to rule out a different tumor secreting ACTH. |
| Normal to elevated but not in hundreds | is not suppressed by low doses, but is suppressed by high doses | Cushing's disease should be considered because the pituitary still retains some feedback control. A pituitary MRI would be needed to confirm. |
†ACTH as measured prior to dosing of dexamethasone[6]
Equivocal results should be followed by a corticotropin-releasing hormone stimulation test, with inferior petrosal sinus sampling.
References
- 1 2 Medline Plus "Dexamethasone suppression test"
- ↑ Nierenberg AA, Feinstein AR (1988). "How to evaluate a diagnostic marker test. Lessons from the rise and fall of dexamethasone suppression test.". JAMA. 259 (11): 1699–702. doi:10.1001/jama.1988.03720110061036. PMID 3278149.
- ↑ Cole MA, Kim PJ, Kalman BA, Spencer RL (February 2000). "Dexamethasone suppression of corticosteroid secretion: evaluation of the site of action by receptor measures and functional studies". Psychoneuroendocrinology. 25 (2): 151–67. doi:10.1016/S0306-4530(99)00045-1. PMID 10674279.
- ↑ Isidori AM, Kaltsas GA, Mohammed S, et al. (November 2003). "Discriminatory value of the low-dose dexamethasone suppression test in establishing the diagnosis and differential diagnosis of Cushing's syndrome". J. Clin. Endocrinol. Metab. 88 (11): 5299–306. doi:10.1210/jc.2003-030510. PMID 14602765.
- ↑ Kumar, Abbas, Fausto. Robbins and Cotran Pathologic Basis of Disease, 7th ed. Elsevier-Saunders; New York, 2005
- ↑ Longo, Dan L.; Fauci, Anthony S.; Kasper, Dennis L.; Hauser, Stephen L.; Jameson, J. Larry; Loscalzo, Joseph (2012), Harrison's Principles of Internal Medicine (18th ed.), McGraw Hill Medical, pp. 2897–2898, ISBN 978-0-07174889-6
- Theodore C. Friedman, M.D., Ph.D. Professor of Medicine-UCLA Chairman, Department of Internal Medicine Charles R. Drew University (2013). http://www.goodhormonehealth.com/talks/cushings-MAGIC-13.ppt