Delta wave

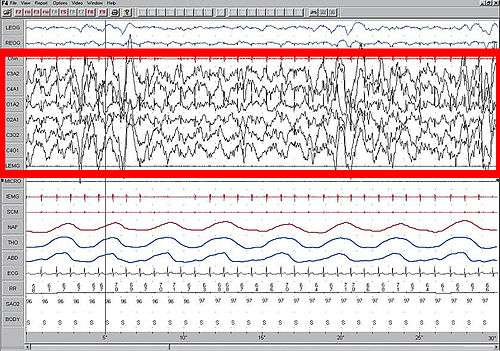
A delta wave is a high amplitude brain wave with a frequency of oscillation between 0.5–4 hertz. Delta waves, like other brain waves, are recorded with an electroencephalogram[1] (EEG) and are usually associated with the deep stage 3 of NREM sleep, also known as slow-wave sleep (SWS), and aid in characterizing the depth of sleep.
Background and history
"Delta waves" were first described in the 1930s by W. Grey Walter, who improved upon Dr. Hans Berger's electroencephalograph machine (EEG) to detect alpha and delta waves. Delta waves can be quantified using Quantitative electroencephalography (qEEG) using freely available toolboxes, such as, EEGLAB or the Neurophysiological Biomarker Toolbox (NBT).
Classification and features
Delta waves, like all brain waves, can be detected by electroencephalography (EEG). Delta waves were originally defined as having a frequency between 1-4 Hz, although more recent classifications put the boundaries at between 0.5 and 2 Hz. They are the slowest and highest amplitude classically described brainwaves, although recent studies have described slower (<0.1 Hz) oscillations[2] Delta waves begin to appear in stage 3 sleep, but by stage 4 nearly all spectral activity is dominated by delta waves. Stage 3 sleep is defined as having less than 50% delta wave activity, while stage 4 sleep has more than 50% delta wave activity. These stages have recently been combined and are now collectively referred to as stage N3 slow-wave sleep.[3] During N3 SWS, delta waves account for 20% or more of the EEG record during this stage.[4] Delta waves occur in all mammals, and potentially all animals as well.
Delta waves are often associated with another EEG phenomenon, the K-complex. K-Complexes have been shown to immediately precede delta waves in slow wave sleep.[5]
Delta waves have also been classified according to the location of the activity into frontal (FIRDA), temporal (TIRDA), and occipital (OIRDA) intermittent delta activity.[6]
Neurophysiology
Sex differences
Women have been shown to have more delta wave activity, and this is true across most mammal species. This discrepancy does not become apparent until early adulthood (in the 30's or 40's, in humans), with men showing greater age-related reductions in delta wave activity than women.[7] It has been suggested that this discrepancy may be due to larger skull size in males, but this theory has been refuted by intracranial data from female cats, which still show more delta activity.
Brain localization and biochemistry
Delta waves can arise either in the thalamus or in the cortex. When associated with the thalamus, they are thought to arise in coordination with the reticular formation.[8][9] In the cortex, the suprachiasmatic nuclei have been shown to regulate delta waves, as lesions to this area have been shown to cause disruptions in delta wave activity. In addition, delta waves show a lateralization, with right hemisphere dominance during sleep.[10] Delta waves have been shown to be mediated in part by T-type calcium channels.[11] During delta wave sleep, neurons are globally inhibited by gamma-aminobutyric acid (GABA).[12]
Delta activity stimulates the release of several hormones, including growth hormone releasing hormone GHRH and prolactin (PRL). GHRH is released from the hypothalamus, which in turn stimulates release of growth hormone (GH) from the pituitary. The secretion of (PRL), which is closely related to (GH), is also regulated by the pituitary. The release of thyroid stimulating hormone (TSH), is decreased in response to delta-wave signaling.[13]
Development
Infants have been shown to spend a great deal of time in slow-wave sleep, and thus have more delta wave activity. In fact, delta-waves are the predominant wave forms of infants. Analysis of the waking EEG of a newborn infant indicates that delta wave activity is predominant in that age, and still appears in a waking EEG of five-year-olds.[14] Delta wave activity during slow-wave sleep declines during adolescence, with a drop of around 25% reported between the ages of 11 and 14 years.[15] Delta waves have been shown to decrease across the lifespan, with most of the decline seen in the mid-forties. By the age of about 75, stage four sleep and delta waves may be entirely absent.[16] In addition to a decrease in the incidence of delta waves during slow-wave sleep in the elderly, the incidence of temporal delta wave activity is commonly seen in older adults, and incidences also increase with age.[17]
Disruptions and disorders
Regional delta wave activity not associated with NREM sleep was first described by W. Grey Walter, who studied cerebral hemisphere tumors. Disruptions in delta wave activity and slow wave sleep are seen in a wide array of disorders. In some cases there may be increases or decreases in delta wave activity, while others may manifest as disruptions in delta wave activity, such as alpha waves presenting in the EEG spectrum. Delta wave disruptions may present as a result of physiological damage, changes in nutrient metabolism, chemical alteration, or may also be idiopathic. Disruptions in delta activity is seen in adults during states of intoxication or delirium and in those diagnosed with various neurological disorders such as dementia or schizophrenia.[18]
Temporal Low-voltage Irregular Delta Wave
Temporal low-voltage irregular delta wave activity has been commonly detected in patients with ischemic brain diseases, particularly in association with small ischemic lesions and is seen to be indicative of early-stage cerebrovascular damage.[19]
Parasomnias
Parasomnias, a category of sleep disorders, are often associated with disruptions in slow wave sleep. Sleep walking and sleep talking most often occur during periods of high delta wave activity. Sleep walkers have also been shown to have more hypersynchronous delta activity (HSD) compared to total time spent in stages 2, 3, and 4 sleep relative to healthy controls. HSD refers to the presence of continuous, high-voltage (> 150 uV) delta waves seen in sleep EEGs.[20] Parasomnias which occur deep in NREM sleep also include sleep terrors and confusional arousals.
Sleep deprivation
Total sleep deprivation has been shown to increase delta wave activity during sleep recovery,[21] and has also been shown to increase hypersynchronous delta activity.[20]
Parkinson's disease
Sleep disturbances, as well as dementia, are common features of Parkinson's disease, and patients with this disease show disrupted brain wave activity. The drug Rotigotine, developed for the treatment of Parkinson's disease, has been shown to increase delta power and slow-wave sleep. Delta-wave inducing peptide injected into the substantia nigra of the rat model has been shown to increase Parkinsonian symptoms.[22]
Schizophrenia
People suffering schizophrenia have shown disrupted EEG patterns, and there is a close association of reduced delta waves during deep sleep and negative symptoms associated with schizophrenia. During slow wave sleep (stages 3 and 4), schizophrenics have been shown to have reduced delta wave activity, although delta waves have also been shown to be increased during waking hours in more severe forms of schizophrenia.[23] A recent study has shown that the right frontal and central delta wave dominance, seen in healthy individuals, is absent in patients with schizophrenia. In addition, the negative correlation between delta wave activity and age is also not observed in those with schizophrenia.[24]
Diabetes and insulin resistance
Disruptions in slow wave (delta) sleep have been shown to increase risk for development of Type II diabetes, potentially due to disruptions in the growth hormone secreted by the pituitary. In addition, hypoglycemia occurring during sleep may also disrupt delta-wave activity.[25] Low-voltage irregular delta waves, have also been found in the left temporal lobe of diabetic patients, at a rate of 56% (compared to 14% in healthy controls).[26][27]
Fibromyalgia
Patients suffering from fibromyalgia often report unrefreshing sleep. A study conducted in 1975 by Moldovsky et al. showed that the delta wave activity of these patients in stages 3 and 4 sleep were often interrupted by alpha waves. They later showed that depriving the body of delta wave sleep activity also induced musculoskeletal pain and fatigue.[28]
Alcoholism
Alcohol has been shown to decrease slow wave sleep and delta power, while increasing stage 1 and REM incidence in both men and women. In long-term alcohol abuse, the influences of alcohol on sleep architecture and reductions in delta activity have been shown to persist even after long periods of abstinence.[29]
Temporal lobe epilepsy
Slow waves, including delta waves, are associated with seizure-like activity within the brain. W. Grey Walter was the first person to use delta waves from an EEG to locate brain tumors and lesions causing temporal lobe epilepsy.[30] Neurofeedback has been suggested as a treatment for temporal lobe epilepsy, and theoretically acts to reduce inappropriate delta wave intrusion, although there has been limited clinical research in this area.[31]
Other disorders
Other disorders frequently associated with disrupted delta-wave activity include:
- Narcolepsy
- Depression
- Anxiety
- Obsessive–compulsive disorder
- Attention deficit hyperactivity disorder (ADHD) and its three subtypes.[32]
- Juvenile chronic arthritis[33]
Consciousness and dreaming
Initially, dreaming was thought to only occur in rapid eye movement sleep, though it is now known that dreaming may also occur during slow-wave sleep. Delta waves and delta wave activity are marked, in most people, by an apparently unconscious state, and the loss of physical awareness as well as the "iteration of information". Nevertheless, some people who practice a type of deep meditation called Yoga Nidra (Sleep yoga) can remain conscious while in delta-sleep.[34]
Delta wave activity has also been purported to aid in the formation of declarative and explicit memory formation. [12]
Cultural and religious role
In Advaita Vedanta, deep dreamless sleep is considered the highest state of consciousness. If one can stay aware or conscious while in deepest dreamless sleep, a deep meditative state (known as "jagrat sushupti") is said to be achievable. This notion of paradoxical consciousness may be linked to high cortical activity which happens during the delta-sleep. [35]
Pharmacology
While most drugs that affect sleep do so by stimulating sleep onset, or disrupting REM sleep, a number of chemicals and drugs have been shown to alter delta wave activity.
- Delta sleep-inducing peptide, as the name suggests, induces delta wave EEG activity.
- Alcohol reduces SWS delta wave activity, thereby restricting the release of growth hormone (GH) by the pituitary.[36]
- The muramyl peptide, muramyl dipeptide (MDP, N-acetylmuramyl-L-alanyl-D-isoglutamine) has been shown to increase delta wave activity during slow wave sleep.[37]
- The drug Gabapentin, a drug used to control epileptic seizures, increases delta-wave activity and slow wave sleep in adults.[38]
- While hypnotic drugs increase slow wave sleep, they do not increase delta wave activity, and instead increase spindle activity during slow wave sleep.[39]
- Gamma-hydroxy butyrate (GHB) increases delta slow-wave sleep as well as sleep-related growth hormone (GH).[39]
Effects of diet
Diets very low in carbohydrates, such as a ketogenic diet, have been shown to increase the amount of delta activity and slow wave sleep in healthy individuals.[40]
See also
- Delta sleep-inducing peptide
- Electroencephalography
- K-complex
- Sensorimotor rhythm
- slow-wave sleep
- Wolff-Parkinson-White syndrome
Brain waves
- Delta wave – (0.1 – 4 Hz)
- Theta wave – (4 – 7 Hz)
- Alpha wave – (8 – 15 Hz)
- Mu wave – (7.5 – 12.5 Hz)
- SMR wave – (12.5 – 15.5 Hz)
- Beta wave – (16 – 31 Hz)
- Gamma wave – (32 – 100 Hz)
References
- ↑ Walker, Peter (1999). Chambers dictionary of science and technology. Edinburgh: Chambers. p. 312. ISBN 0-550-14110-3.
- ↑ Hiltunen T1, Kantola J, Abou Elseoud A, Lepola P, Suominen K, Starck T, Nikkinen J, Remes J, Tervonen O, Palva S, Kiviniemi V, Palva JM. (2014). Infra-slow EEG fluctuations are correlated with resting-state network dynamics in fMRI. [Article]. The Journal of Neuroscience, 34(2): 356-362.
- ↑ "Glossary. A resource from the Division of Sleep Medicine at Harvard Medical School, Produced in partnership with WGBH Educational Foundation". Harvard University. 2008. Retrieved 2009-03-11. "The 1968 categorization of the combined Sleep Stages 3 – 4 was reclassified in 2007 as Stage N3."
- ↑ Iber C, Ancoli-Israel S, Chesson A, and Quan SF for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, 1st ed.: Westchester, Illinois: American Academy of Sleep Medicine, 2007.
- ↑ De Gennaro, L., Ferrara, M., & Bertini, M. (2000). The spontaneous K-complex during stage 2 sleep: is it the 'forerunner' of delta waves? [Article]. Neuroscience Letters, 291(1), 41–43.
- ↑ Brigo F (2011). "Intermittent rhythmic delta activity patterns". Epilepsy & Behavior : E&B (Review). 20 (2): 254–6. doi:10.1016/j.yebeh.2010.11.009. PMID 21276757.
- ↑ Ehlers, C. L., and D. J. Kupfer. "Slow-wave Sleep: Do Young Adult Men and Women Age Differently?" J Sleep Res. 6.3 (1997): 211-15. Print.
- ↑ Gross, Richard E. (1992). Psychology: the science of mind and behaviour. London: Hodder & Stoughton. pp. 112–113. ISBN 0-340-56136-X.
- ↑ Maquet, P., Degueldre, C., Delfiore, G., Aerts, J., Peters, J. M., Luxen, A., et al. (1997). Functional neuroanatomy of human slow wave sleep. Journal of Neuroscience, 17(8), 2807-2812.
- ↑ Mistlberger, R. E., Bergmann, B. M., & Rechtschaffen, A. (1987). RELATIONSHIPS AMONG WAKE EPISODE LENGTHS, CONTIGUOUS SLEEP EPISODE LENGTHS, AND ELECTROENCEPHALOGRAPHIC DELTA WAVES IN RATS WITH SUPRACHIASMATIC NUCLEI LESIONS. [Article]. Sleep, 10(1), 12-24.
- ↑ Lee, J., Kim, D., Shin, H. Lack of delta waves and sleep disturbances during non-rapid eye movement sleep in mice lacking a1g-subunit of T-type calcium channels. PNAS;101(52): 18195-18199.
- 1 2 Hobson, J. , & Pace-Schott, E. (2002). The Cognitive Neuroscience of Sleep: Neuronal Systems, Consciousness and Learning. Nature Reviews Neuroscience, 3(9), 679-693.
- ↑ Brandenberger, G. (2003). The Ulradien Rhythm of Sleep: Diverse Relations with Pituitary and Adrenal Hormones. Revue Neurologique, 159(11), S5-S10.
- ↑ Taylor, Eric; Rutter, Michael (2002). Child and adolescent psychiatry. Oxford: Blackwell Science. p. 162. ISBN 0-632-05361-5.
- ↑ "Brain Wave Changes In Adolescence Signal Reorganization Of The Brain". ScienceDaily. 2006-12-08. Retrieved 2008-03-24.
- ↑ Colrain, I. M., Crowley, K. E., Nicholas, C. L., Afifi, L., Baker, F. C., Padilla, M., et al. (2010). Sleep evoked delta frequency responses show a linear decline in amplitude across the adult lifespan. [Article]. Neurobiology of Aging, 31(5), 874-883.
- ↑ Inui, Koji, Eishi Motomura, Hiroyuki Kaige, and Sen Nomura. "Temporal Slow Waves and Cerebrovascular Diseases - Inui - 2008 - Psychiatry and Clinical Neurosciences." Psychiatry and Clinical Neurosciences 55.5 (2001): 525-31. Wiley Online Library. Web. 29 Nov. 2010.
- ↑ Hales, Robert E.; Yudofsky, Stuart C. (2007). The American Psychiatric Publishing Textbook of Neuropsychiatry and Behavioral Neurosciences, Fifth Edition (American Psychiatric Press Textbook of Neuropsychiatry). American Psychiatric Publishing, Inc. ISBN 1-58562-239-7.
- ↑ Inui, Koji, Hozumi Kawamoto, Masahiko Kawakita, Kazuhisa Wako, Hiromichi Nakashima, Masanori Kamihara, and Junichi Nomura. "Temporal Delta Wave and Ischemic Lesions on MRI." Psychiatry and Clinical Neurosciences 48.4 (1994): 891-98. Print.
- 1 2 Pilon M; Zadra A; Joncas S et al. Hypersynchronous delta waves and somnambulism: brain topography and effect of sleep deprivation. SLEEP 2006;29(1): 77-84.
- ↑ Feinberg, I., T. Baker, R. Leder, and J. D. March. "Response of Delta (0-3 Hz) EEG and Eye Movement Density to a Night with 100 Minutes of Sleep." Sleep 11.5 (1988): 473-87. Print.
- ↑ Kryzhanovskii, G. N., A. A. Shandra, L. S. Godlevskii, and I. I. Mikhaleva. "Appearance of Parkinsonian Syndrome after Administration of Delta Sleep-inducing Peptide into the Rat Substantia Nigra." Biull Eksp Biol Med. 109.2 (1990): 119-21. Print.
- ↑ Alfimova, M. V., & Uvarova, L. G. (2007). Changes in the EEG spectral power during perception of neutral and emotionally salient words in schizophrenic patients, their relatives and healthy individuals from general population. [Article]. Zhurnal Vysshei Nervnoi Deyatelnosti Imeni I P Pavlova, 57(4), 426-436.
- ↑ Sekimoto, M., et al., Cortical regional differences of delta waves during all-night sleep in schizophrenia, Schizophr. Res. (2010), doi:10.1016/j.schres.2010.11.003
- ↑ Abdelkarim, T. H., Westin, T., Romaker, A., & Girish, M. (2002). Presence of delta waves in REM sleep during polysomnography as a sign of acute hypoglycemic encephalopathy. [Meeting Abstract]. Sleep, 25, 531.
- ↑ Appearance of Parkinsonian Syndrome after Administration of Delta Sleep-inducing Peptide into the Rat Substantia Nigra." Biull Eksp Biol Med. 109.2 (1990): 119-21. Print.
- ↑ Inui, K., H. Sannan, H. Ota, Y. Uji, S. Nomura, H. Kaige, I. Kitayama, and J. Nomura. "EEG Findings in Diabetic Patients with and without Retinopathy." Acta Neurologica Scandinavica 97.2 (1998): 107-09. Print.
- ↑ Nezu, Arthur M. ., Christine Maguth. Nezu, Pamela A. . Geller, and Irving B. . Weiner. Handbook of Psychology. New York: Wiley, 2003. Print.
- ↑ Colrain, I. M., S. Turlington, and F. C. Baker. "Impact of Alcoholism on Sleep Architecture and EEG Power Spectra in Men and Women." Sleep. 32.10 (2009): 1341-352. Print.
- ↑ Walter WG. The location of cerebral tumors by electroencephalography. Lancet 1936;2: 305–8.
- ↑ "Biofeedback for Epileptic Seizures; EEG Neurofeedback for Epilepsy". Epilepsyhealth.com. Retrieved 2011-02-14.
- ↑ EEG-defined subtypes of children with attention-deficit/hyperactivity disorder. Adam R Clarke, Robert J Barry, Rory McCarthy, Mark Selikowitz. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 1 November 2001 (volume 112 issue 11 Pages 2098-2105)
- ↑ Lopes, M.C., Guilleminault, C., Rosa, A., Passarelli, C., Roizenblatt, S., Tufik, S. Delta sleep instability in children with chronic arthritis. Brazilian Journal of Medical and Biological Research. 2008;41(10): 938-43.
- ↑ Miller, Richard (February 10, 2010). Yoga Nidra (Pap/Com ed.). Boulder, CO: Sounds True, Incorporated. p. 104. ISBN 1591797586.
- ↑ Sharma Arvind: Sleep as a State of Consciousness in Advaita Vedanta; State University of New York Press, 2004
- ↑ Lands, William. "Alcohol, Slow Wave Sleep, and the Somatotropic Axis." Alcohol 18.2 (1999): 109-22.
- ↑ Davenne, D. M. "Enhancement of Quiet Sleep in Rabbit Neonates by Muramyl Dipeptide." Am J Physiol. 253.4 (1987): 646-54. Print.
- ↑ Foldvary-Schaefer, N., I. De Leon Sanchez, M. Karafa, D. Dinner, and H. H. Morris. "Gabapentin Increases Slow-wave Sleep in Normal Adults." Epilepsia 43.12 (2002): 1493-497. Print.
- 1 2 D'haenen, H. A. H., Johan A. Den Boer, and Paul Willner. Biological Psychiatry. Chichester: Wiley, 2002. Print.
- ↑ Afaghi, A. , O'Connor, H. , & Chow, C. (2008). Acute Effects of the Very Low Carbohydrate Diet on Sleep Indices. Nutritional Neuroscience, 11(4), 146-154.