Delirium
| Delirium | |
|---|---|
 | |
| Video explanation | |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | F05 |
| ICD-9-CM | 780.09 |
| DiseasesDB | 29284 |
| MedlinePlus | 000740 |
| eMedicine | med/3006 |
| Patient UK | Delirium |
| MeSH | D003693 |
Delirium, or acute confusional state, is an organically caused decline from a previously attained baseline level of cognitive function. It is typified by fluctuating course, attentional deficits and generalized severe disorganization of behavior. It typically involves other cognitive deficits, changes in arousal (hyperactive, hypoactive, or mixed), perceptual deficits, altered sleep-wake cycle, and psychotic features such as hallucinations and delusions.
Delirium itself is not a disease, but rather a clinical syndrome (a set of symptoms). It may result from an underlying disease, over-consumption of alcohol, from drugs administered during treatment of a disease, withdrawal from drugs or from any number of health factors. Delirium may be difficult to diagnose without the proper establishment of the baseline mental function of a patient.
Delirium may be caused by a disease process outside the brain that nonetheless affects the brain, such as infection (urinary tract infection, pneumonia) or drug effects, particularly anticholinergics or other CNS depressants (benzodiazepines and opioids).[1] Although hallucinations and delusions are sometimes present in delirium, these are not required for the diagnosis, and the symptoms of delirium are clinically distinct from those induced by psychosis or hallucinogens (with the exception of deliriants.) Delirium must by definition be caused by an organic process, i.e., a physically identifiable structural, functional, or chemical problem in the brain (see organic brain syndrome), and thus, fluctuations of mentation due to changes in purely psychiatric processes or diseases, such as sudden psychosis from schizophrenia or bipolar disorder, are (by definition) not termed delirium. Like its components (inability to focus attention, mental confusion and various impairments in awareness and temporal and spatial orientation), delirium is the common manifestation of new organic brain dysfunction (for any reason). Delirium requires both a sudden change in mentation, and an organic cause for this. Thus, without careful assessment and history, delirium can easily be confused with a number of psychiatric disorders or long term organic brain syndromes, because many of the signs and symptoms of delirium are conditions also present in dementia, depression, and psychosis.[2] Delirium may newly appear on a background of mental illness, baseline intellectual disability, or dementia, without being due to any of these problems.
Treatment of delirium requires treating the underlying cause, and multi-component interventions are thought to be most effective.[3] In some cases, temporary or palliative or symptomatic treatments are used to comfort the person or to allow other care (for example, a person who, without understanding, is trying to pull out a ventilation tube that is required for survival). Delirium is probably the single most common acute disorder affecting adults in general hospitals. It affects 10-20% of all hospitalized adults, and 30-40% of elderly who are hospitalized and up to 80% of those in ICU. Among those requiring critical care, delirium is a risk for death within the next year.[4] Antipsychotics are not supported for the treatment or prevention of delirium among those who are in hospital.[3][5] However, when delirium is caused by alcohol or sedative hypnotic withdrawal, benzodiazepines are typically used.[6]
Definition
In common usage, delirium is often used to refer to drowsiness, disorientation, and hallucination. In medical terminology, however, a number of different symptoms, including temporary disturbance in consciousness, with reduced ability to focus attention and solve problems, are the core features of delirium. Occasionally sleeplessness and severe agitation and irritability are part of "delirium." Hallucination, drowsiness, and disorientation are not required, but may be contribute to the diagnosis.
There are several medical definitions of delirium (including those in the DSM-IV and ICD-10). However, all include some core features.
The core features are:
- Disturbance of consciousness (that is, reduced clarity of awareness of the environment, with reduced ability to focus, sustain, or shift attention)[7]
- Change in cognition (e.g., problem-solving impairment or memory impairment) or a perceptual disturbance (hallucination)[7]
- Onset of hours to days, and tendency to fluctuate.[7]
- Behaviour may be either overactive or underactive, and sleep is often disturbed, with loss of the normal Circadian rhythm.[7]
- Thinking is slow and muddled but the content is often complex.[8]
Other clinical features include disorganized thinking, poor memory, delusions, and mood lability.[7]
Signs and symptoms
Delirium is a syndrome encompassing an array of neuropsychiatric symptoms, including a disturbance in consciousness/attention and cognition that develops acutely and tends to fluctuate.[7] The change in cognition (memory deficit, disorientation, language disturbance) or the development of a disturbance, must be one that is not better accounted for by a pre-existing, established, or evolving dementia.[9] Other symptoms can include disorientation, thought disorder, memory problems, language disorder, sleep disturbance, delusions, mood lability, psychomotor changes (changes in rate of activity/movement), and hallucinations.[7]
Delirium occurs as a stage of consciousness in the continuum between normal awakeness/alertness and coma. During the 20th century, delirium was described as a ‘clouding of consciousness’ but this rather nebulous concept has been replaced by a better understanding of the components of phenomenology that culminate in severely impaired higher order brain functions. Lipowski described delirium as a disorder of attention, wakefulness, cognition, and motor behaviour, while a disturbance in attention is often considered the cardinal symptom.[7] Disrupted sleep-wake cycles can result from a loss of normal circadian rhythm.[7]
Accumulating evidence indicates three core domains of delirium phenomenology: “Cognition”, composed of inattention and other cognitive deficits; “Higher Level Thinking Processes” including impaired executive function, semantic expression and comprehension; and “Circadian Rhythm” including altered motor activity and fragmented sleep-wake cycle.[10] Phenomenology studies suggest that “core” symptoms occur with greater frequency while other less consistent “associated” symptoms may reflect the biochemical influence of particular aetiologies or genetic, neuronal or physiological vulnerabilities.[10]
Delirium may present in hyperactive, hypoactive, or mixed forms. In its hyperactive form, it is manifested as severe confusion and disorientation, developing with relatively rapid onset and fluctuating in intensity. In its hypoactive form, it is manifested by an equally sudden withdrawal from interaction with the outside world. Delirium may occur in a mixed type where someone may fluctuate between both hyper- and hypoactive periods. Delirium as a syndrome is one which occurs more frequently in people in their later years. However, when it occurs in the course of a critical illness, delirium has been found to occur in young and old patients at relatively even rates.
Inattention and associated cognitive deficits
Inattention is the cardinal and required symptom to diagnose delirium and is noticeable on interview by distractibility and inability to shift and / or sustain attention.[11] More formal testing can include the months of the year backwards, serial sevens or digit span tests. Disorientation (another symptom of confusion, and usually a more severe one) describes the loss of awareness of the surroundings, environment and context in which the person exists. It may also appear with delirium, but it is not required, as noted. Disorientation may occur in time (not knowing what time of day, day of week, month, season or year it is), place (not knowing where one is) or person (not knowing who one is).
Memory impairment occurs[7] and is linked to inattention. Reduction in formation of new long-term memory (which by definition survives withdrawal of attention), is common in delirium, because initial formation of (new) long-term memories generally requires an even higher degree of attention than do short-term memory tasks. Since older memories are retained without need of concentration, previously formed long-term memories (i.e., those formed before the period of delirium) are usually preserved in all but the most severe cases of delirium.
Higher level thinking
Delirious patients have diminished comprehension as evidenced by reduced ‘grasp’ of their surroundings and difficulties in connecting with their immediate environment, executive dysfunction affecting abstraction, initiation/perseveration, switching mental sets, working memory, temporal sequencing and organization, insight and judgment. Though none of these cognitive deficits is specific to delirium, the array and pattern is highly suggestive.
Language disturbances in delirium include anomic aphasia, paraphasias, impaired comprehension, agraphia, and word-finding difficulties. Incoherent or illogical / rambling conversation is reported commonly. Disorganised thinking includes tangentiality, circumstantiality and a proneness to loose associations between elements of thought which results in speech that often makes limited sense with multiple apparent irrelevancies. This aspect of delirium is common but often difficult for non-experts to assess reliably.
Sleep changes
Disruption of sleep-wake cycle is almost invariably present in delirium and often predates the appearance of a full-blown episode. Minor disturbances with insomnia or excessive daytime somnolence may be hard to distinguish from other medically ill patients without delirium, but delirium typically involves more substantial alterations with sleep fragmentation or even complete sleep-wake cycle reversal that reflect disturbed circadian rhythm regulation. The relationship of circadian disturbances to the characteristic fluctuating severity of delirium symptoms over a 24-hour period or to motor disturbance is unknown.
Motor activity alterations are very common in delirium. They have been used to define clinical subtypes (hypoactive, hyperactive, mixed) though studies are inconsistent as to the prevalence of these subtypes.[12] Cognitive impairments and EEG slowing are comparable in hyperactive and hypoactive patients though other symptoms may vary. Psychotic symptoms occur in both although the prevailing stereotype suggests that they only occur in hyperactive cases. Hypoactive cases are prone to non detection or misdiagnosis as depression. A range of studies suggest that motor subtypes differ regarding underlying pathophysiology, treatment needs, and prognosis for function and mortality though inconsistent subtype definitions and poorer detection of hypoactives impacts interpretation of these findings.[13]
Psychotic symptoms occur in up to 50% of patients with delirium. While the common non-medical view of a delirious patient is one who is hallucinating, most people who are medically delirious do not have either hallucinations or delusions. Thought content abnormalities include suspiciousness, overvalued ideation and frank delusions. Delusions are typically poorly formed and less stereotyped than in schizophrenia or Alzheimer’s disease. They usually relate to persecutory themes of impending danger or threat in the immediate environment (e.g. being poisoned by nurses). Misperceptions include depersonalisation, delusional misidentifications, illusions and hallucinations. Hallucinations and illusions are frequently visual though can be tactile and auditory. Abnormalities of affect which may attend the state of delirium may include many distortions to perceived or communicated emotional states. Emotional states may also fluctuate, so that a delirious person may rapidly change between, for example, terror, sadness and jocularity.[14]
Persistent delirium
It was thought for many years that all delirium was a transient state of brain dysfunction that fluctuated on an hourly basis. Interestingly, Barrough noted in 1583 that if delirium resolves, it may be followed by a "loss of memory and reasoning power." Recent long-term studies bear this out, showing that many patients end up meeting criteria for delirium for an alarmingly long time.[15] For example, in ICU cohorts, it is common to find that 10% of patients still have delirium at the time of hospital discharge.[16]
Dementia in ICU survivors
Dementia is supposed to be an entity that continues to decline, such as Alzheimer’s disease. Another way of looking at dementia, however, is not strictly based on the decline component but on the degree of memory and executive function problems. It is now known, for example, that between 50% and 70% of ICU patients have tremendous problems with ongoing brain dysfunction that looks a lot like the degree of problems experienced by Alzheimer’s or TBI (traumatic brain injury) patients and which leaves too many ICU survivors disabled and unable to go back to work and unable to serve effectively as the matriarchs and patriarchs of their families.[17] This is a distressing personal and public health problem that is getting an increasing amount of scrutiny in ongoing investigations. The implications of such an “acquired dementia-like illness” (note: the term here is being used in a circumstance in which not all patients continue to decline as some have persistent yet stable brain dysfunction and others with newly acquired brain problems can recover fully) are profound at the private level, dismantling the person’s life in very practical ways such as inability to find a car in a parking lot or even complete shopping lists or job-related tasks done previously for years. The societal relevance is also huge when one considers work-force issues related to the inability of a young wage earner being unable to work because of either being a newly disabled ICU survivor themselves or because they now have to care for their family member who is now suffering this “dementia-like” illness following ICU care.
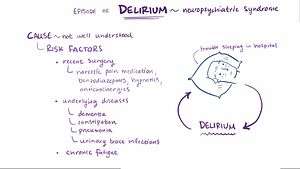
Causes
Delirium arises through the interaction of a number of predisposing and precipitating factors. A predisposing factor might be any biological, psychological or social factor that increases an individual’s susceptibility to delirium. An individual with multiple predisposing factors is said to have ‘high baseline vulnerability’, and this is closely associated with frailty (see below). A precipitating factor is any biological, psychological or social factor that can trigger delirium. The division of causes into ‘predisposing’ and ‘precipitating’ is useful in order to assess an individual’s risk of suffering from delirium, and in guiding the management of delirium – however there may be a significant degree of overlap between the two categories.
Delirium most commonly affects the frail and infirm. Frailty is usually the result of multiple physical and social causes, and is often viewed as a symptom of old age or ill health. Health can be described as a balance between fitness and frailty, in which fitness results from physical and socioeconomic assets, and frailty results from physical and socioeconomic deficits. Frail individuals (i.e. those with significant predisposing factors) demonstrate an inability to compensate for additional physical or social stressors (‘precipitating factors’). In a frail individual, a single or mild precipitating factor could be sufficient to trigger an episode of delirium. Conversely, delirium may only result in a fit individual if they suffer serious or multiple precipitating factors. It is important to note that the factors affecting the fitness or frailty of an individual can change over time, thus an individual’s risk of delirium is in a state of flux.
Predisposing factors
The most important predisposing factors are listed below:
- Older age
- Cognitive impairment / dementia
- Physical comorbidity (biventricular failure, cancer, cerebrovascular disease)
- Psychiatric comorbidity (e.g., depression)
- Sensory impairment (vision, hearing)
- Functional dependence (e.g., requiring assistance for self-care and/or mobility)
- Dehydration / malnutrition
- Drugs and drug-dependence.
- Alcohol dependence
Precipitating factors
Any acute factors that affect neurotransmitter, neuroendocrine or neuroinflammatory pathways can precipitate an episode of delirium in a vulnerable brain. Clinical environments can also precipitate delirium, and optimal nursing and medical care is a key component of delirium prevention.[18] Some of the most common precipitating factors are listed below:
- Metabolic
- Malnutrition
- Dehydration, electrolyte imbalance
- Anaemia
- Hypoxia
- Hypercapnoea
- Hypoglycaemia
- Endocrine disorders (e.g., SIADH, Addison’s disease, hyperthyroidism, hypercalcaemia)
- Infection
- Especially respiratory and urinary tract infections
- Medication
- Anticholinergics, dopaminergics, opioids, steroids, recent polypharmacy
- General Anesthetic
- Vascular
- Stroke/Transient ischaemic attack
- Myocardial infarction, arrhythmias, decompensated heart failure
- Physical/psychological stress
- Pain
- Iatrogenic event, esp. post-operative, mechanical ventilation in ICU
- Chronic/terminal illness, esp. cancer
- Post-traumatic event (e.g., fall, fracture)
- Immobilisation/restraint
- Severe constipation/fecal impaction
- Urinary retention
- Other
- Substance withdrawal (esp. alcohol, benzodiazepines)
- Substance intoxication
- Traumatic head injury
Pathophysiology
Animal models
The pathophysiology of delirium is not well understood and a lack of animal models that are relevant to the syndrome has left many key questions in delirium pathophysiology unanswered. Earliest rodent models of delirium used an antagonist of the muscarinic acetylcholine receptors, atropine, to induce cognitive and EEG changes similar to delirium. Similar anticholinergic drugs such as biperiden and scopolamine have also produced delirium-like effects. These models, along with clinical studies of drugs with ‘anticholinergic activity’ have contributed to a hypocholinergic theory of delirium.[19]
Profound systemic inflammation occurring during bacteraemia/sepsis is also known to cause delirium (often termed septic encephalopathy). Modeling this in mice also causes robust brain dysfunction and probably a delirium-like state, although these animals are typically too sick to assess cognitively and measures such as EEG and magnetic resonance imaging/spectroscopy are necessary to demonstrate dysfunction.
Animal models that interrogate interactions between prior degenerative pathology and superimposed systemic inflammation have been developed more recently and these demonstrate that even mild systemic inflammation, a frequent trigger for clinical delirium, induces acute and transient attentional/working memory deficits, but only in animals with prior pathology.[20] Prior dementia or age-associated cognitive impairment is the primary predisposing factor for clinical delirium and ‘prior pathology’ as defined by these new animal models may consist of synaptic loss, network disconnectivity, and primed microglia (brain macrophages that are ‘primed’ by the primary pathology to produce exaggerated responses to subsequent inflammatory insults).
While it is difficult to state with confidence whether delirium is occurring in a non-verbal animal, comparisons with human DSM-IV criteria remain useful. According to DSM-IV, demonstration of acute onset impairments in attention and some other cognitive domain, that cannot be better explained by existing dementia and that are triggered by physiological disturbances resulting from some general medical condition should be present in order to reach a ‘diagnosis’ of delirium. Recent animal models fulfill these criteria reasonably well.[20] Whether the deficit is one of attention or short-term memory is difficult to dissect, but it is undeniably distinct from long-term memory, consistent with observations in patients with delirium. There is an urgent need to understand more about the mechanisms of dysfunction underpinning delirium and data arising from these and other animal models must form part of the discussion on delirium pathophysiology.
Cerebrospinal fluid biomarkers
Studies of cerebrospinal fluid (CSF) in delirium are difficult to perform. Apart from the general difficulty of recruiting participants who are often unable to give consent, the inherently invasive nature of CSF sampling makes such research particularly challenging. However, a few studies have exploited the opportunity to sample CSF from persons undergoing spinal anaesthesia for elective or emergency surgery. Indeed, spinal anaesthesia may in fact be the anaesthetic modality of choice for frail older patients, so these studies are often undertaken in highly relevant populations.
A systematic review identified 8 studies involving 235 patients (142 with delirium).[21] Overall, 17 different biomarkers were considered and each article identified in the review focused on a narrow range of biomarkers with no overlap between studies. Studies were generally small, studying heterogeneous populations with different times of CSF sampling in relation to delirium, and no clear conclusions could be drawn. Broadly, delirium may be associated with: increased serotoninergic and dopamine signalling; reversible fall in somatostatin; increased cortisol; and increase in some inflammatory cytokines (IL-8, IL-1β), but possibly not others (TNF-α).
One additional study has since been published.[22] Postoperative delirium was strongly associated with pre-operative cognitive decline. However, CSF Aβ1-42, tau, and phosphorylated-tau levels were not associated with delirium status, nor did they correlate significantly with cognitive function before the onset of delirium. The two main explanations for these findings are either: (1) the study was underpowered to detect mediating pathways between premorbid cognitive impairment, Alzheimer’s pathology biomarkers and subsequent delirium; or (2) postoperative delirium arises through pathophysiological pathways that are distinct from Alzheimer's disease.
Neuroimaging
The neuroimaging correlates of delirium are very difficult to establish. Many attempts to image people with concurrent delirium will be unsuccessful. In addition, there is a more general bias selecting younger and fitter participants amenable to scanning, especially if using intensive protocols such as MRI.
Most of the literature has been summarised by a systematic review.[23] This found 12 articles for inclusion, most with small sample sizes (total number of cases 127). There was substantial heterogeneity in populations, study design, and imaging modalities such that no firm conclusions were made. Generally, structural imaging suggested that diffuse brain abnormalities such as atrophy and leukoaraiosis might be associated with delirium, though few studies could account for differences in key variables such as age, sex, education or underlying cognitive function and education.
Since publication of the systematic review, five further studies have been published. The largest-scale report was VISIONS.[24][25] This prospectively examined the neuroimaging correlates of delirium in 47 participants after critical illness. Delirium duration was related to measures of white matter tract integrity and this in turn was related to poorer cognitive outcomes at 3 and 12 months. In addition, brain volumes were also assessed and related to cognitive outcomes in the same manner. Overall, the study found that longer duration of delirium was associated with smaller brain volume and more white matter disruption, and both these correlated with worse cognitive scores 12 months later.
Two studies examined delirium risk as a post-operative complication after elective cardiac surgery. These both showed that white matter damage predicted post-operative delirium.[26][27] One functional MRI study reported a reversible reduction in activity in brain areas localising with cognition and attention function.[28]
Neurophysiology
Electroencephalography (EEG) is an attractive mode of study in delirium as it is able to capture measures of global brain function. There are also opportunities to summarise temporal fluctuations as continuous recordings, compressed into power spectra (quantitative EEG, qEEG). Since the work of Engel and Romano in the 1950s, delirium has been known to be associated with a generalised slowing of background activity.[29]
A systematic review identified 14 studies for inclusion, representing a range of different populations: 6 in older populations, 3 in ICU, sample sizes between 10 and 50).[30] For most studies, the outcome of interest was the relative power measures, in order: alpha, theta, delta frequencies. The relative power of the theta frequency was consistently different between delirium and non-delirium patients. Similar findings were reported for alpha frequencies. In two studies, the relative power of all these bands was different within patients before and after delirium.
Neuropathology
Only a handful of studies exist where there has been an attempt to correlate delirium with pathological findings at autopsy. A case series has been reported on 7 patients who died during ICU admission.[31] Each case was admitted with a range of primary pathologies, but all had acute respiratory distress syndrome and/or septic shock contributing to the delirium. 6/7 had evidence of hypoperfusion and diffuse vascular injury, with consistent involvement of the hippocampus in 5/7.
A case-control study examined 9 delirium cases with 6 age-matched controls, investigating inflammatory cytokines and their role in delirium.[32] Persons with delirum had higher scores for HLA-DR and CD68 (markers of microglial activation), IL-6 (cytokines pro-inflammatory and anti-inflammatory activities) and GFAP (marker of astrocyte activity). These results might suggest a neuroinflammatory substrate to delirium, but the conclusions are limited by biases from selection of controls.
Diagnosis
Differential points from other processes and syndromes that cause cognitive dysfunction:
- Delirium may be distinguished from psychosis, in which consciousness and cognition may not be impaired (however, there may be overlap, as some acute psychosis, especially with mania, is capable of producing delirium-like states).
- Delirium is distinguished from dementia (chronic organic brain syndrome) which describes an "acquired" (non-congenital) and usually irreversible cognitive and psychosocial decline in function. Dementia usually results from an identifiable degenerative brain disease (for example Alzheimer disease or Huntington's disease). Dementia is usually not associated with a change in level of consciousness, and a diagnosis of dementia requires a chronic impairment.
- Delirium is distinguished from depression.
- Delirium is distinguished by time-course from the confusion and lack of attention which result from long term learning disorders and varieties of congenital brain dysfunction. Delirium has also been referred to as 'acute confusional state' or 'acute brain syndrome'. The key word in both of these descriptions is "acute" (meaning: of recent onset), since delirium may share many of the clinical (i.e., symptomatic) features of dementia or developmental disabilities including attention deficit hyperactivity disorder, with the important exception of symptom duration.
Delirium represents an organically caused decline from a previously attained level of cognitive functioning. It is a corollary of these differential criteria that a diagnosis of delirium cannot be made without a previous assessment, or knowledge, of the affected person's baseline level of cognitive function. In other words, a mentally disabled or demented person who is operating at their own baseline level of mental ability might appear to be delirious without a baseline functional status against which to compare.
Mental illness
Some mental illnesses, such as a manic episode of bipolar disorder, or some types of acute psychosis, may cause a rapidly fluctuating impairment of cognitive function and ability to focus. Outwardly this appears similar to a confused state caused by inadequate brain metabolism but it actually comes from problems in functioning. However, they are not technically causes of delirium, since any fluctuating cognitive symptoms that occur as a result of these mental disorders are considered by definition to be due to the mental disorder itself, and to be a part of it. Thus, physical disorders can be said to produce delirium as a mental side-effect or symptom, although primary mental disorders which produce the symptom cannot be put into this category once identified. However, such symptoms may be impossible to distinguish clinically from delirium resulting from physical disorders, if a diagnosis of an underlying mental disorder is yet to be made.
Diagnosis in general settings
Multiple guidelines recommend that delirium should be diagnosed when it presents to healthcare services. Much evidence suggest, however, that delirium is greatly underdiagnosed.[33] Higher rates of detection of delirium in general settings (for the ICU see below) can be assisted by the use of validated delirium screening tools. Many such tools have been published. They differ in duration, complexity, need for training, and so on. Examples of tools in use in clinical practice are: Delirium Observation Screening Scale,[34] the Nursing Delirium Screening Scale (Nu-DESC),[35] the Confusion Assessment Method,[36] the Recognizing Acute Delirium As part of your Routine (RADAR) tool [37] and the 4 "A"s Test or 4AT.[38]
Diagnosis in ICU
In the ICU, international guidelines recommend that every patient gets checked for delirium every day (usually twice or more a day) using a validated clinical tool.[39] The two most widely used are the Confusion Assessment Method for the ICU (CAM-ICU)[40] and the Intensive Care Delirium Screening Checklist (ICDSC).[41] There are translations of these tools in over 20 languages and they are used globally in many thousands of ICUs, and instructional videos and myriad implementation tips are available.[42] It is not as important which tool is used as that the patient gets monitored. Without using one of these tools, 75% of ICU delirium is missed by the practicing team, which leaves the patient without any likely active interventions to help reduce the duration of his/her delirium.[43]
The most salient component of the definition of delirium that nurses and other healthcare professionals use at the bedside is whether or not the patient can pay attention and follow simple commands (see videos and literature[42]). The advent of daily monitoring for delirium, made easy by the CAM-ICU[44] and other assessment tools, as well as proper documentation, had led to important changes in the culture of ICUs and rounds in that the entire team can now discuss the brain and how it is doing in terms of being “on” (not delirious) or “off” (delirious) and then focus on the several most likely causes of delirium in any specific patient. Thus, it is not the monitoring itself that changes the patient’s clinical course, but rather it is this combination of monitoring and then relaying the information on rounds in the ICU that makes such a huge difference in awareness of this form of organ dysfunction and then enables a difference to be made in clinical outcomes.
Prevention
Episodes of delirium can be prevented by identifying hospitalized people at risk of the condition: those over 65, those with a known cognitive impairment, those with hip fracture, those with severe illness.[45] Close observation for the early signs is recommended in those people.
Systematically addressing the common contributing factors (such as constipation, dehydration and polypharmacy), as well as providing a therapeutic environment (such as adequate lighting, minimizing noise, clear communication, minimizing relocation, signage, ways to tell the time, and helping the person to walk and be mobile) may prevent delirium.[45][46][47][3] Rates with a number of interventions together decrease rates to 0.72 from baseline in the elderly.[48]
It is thought that 30–40% of all cases of delirium could be prevented, and that high rates of delirium reflect negatively on the quality of care.[46] Melatonin and other pharmacological agents have been studied for prevention of postoperative delirium, but evidence is not clear.[49][3]
It is unclear if the medication donepezil, a cholinesterase inhibitor, reduces delirium following surgery.[3] There is also no clear evidence to suggest that citicoline, Methylprednisolone, or antipsychotic medications prevent delirium.[3]
Treatment
Treatment of delirium involves two main strategies: first, treatment of the underlying presumed acute cause or causes; secondly, optimising conditions for the brain. This involves ensuring that the person with delirium has adequate oxygenation, hydration, nutrition, and normal levels of metabolites, that drug effects are minimised, constipation treated, pain treated, and so on. Detection and management of mental stress is also important. Therefore, the traditional concept that the treatment of delirium is 'treat the cause' is not adequate; people with delirium require a highly detailed and expert analysis of all the factors which might be disrupting brain function.
Non medication treatments are the first measure in delirium, unless there is severe agitation that places the person at risk of harming oneself or others. Avoiding unnecessary movement, involving family members, having recognizable faces at the bedside, having means of orientation available (such as a clock and a calendar) may be sufficient in stabilizing the situation.[45][46] If this is insufficient, verbal and non-verbal de-escalation techniques may be required to offer reassurances and calm the person experiencing delirium.[45] Only if this fails, or if de-escalation techniques are inappropriate, is pharmacological treatment indicated.[45][46]
“The T-A-DA method (tolerate, anticipate, don't agitate)”[50] can be an effective management technique for older people with delirium. All unnecessary attachments are removed (IVs, catheters, NG tubes) which allows for greater mobility.[50] Patient behavior is tolerated even if it is not considered normal as long as it does not put the patient or other people in danger.[50] This technique requires that patients are isolated in a specific area designated for patients of old age dealing with symptoms of delirium.[50] Patient behavior is anticipated so care givers can plan required care. Patients are treated to reduce agitation.[50] Reducing agitation may mean that patients are not reoriented if reorientation causes agitation.[50]
Physical restraints are occasionally used as a last resort with patients in a severe delirium. Restraint use should be avoided as it can increase agitation and risk of injury.[51] In order to avoid the use of restraints some patients may require constant supervision.
Medications
The treatment for delirium with medications depends on its cause. Antipsychotics, particularly haloperidol, are the most commonly used drugs for delirium and the most studied.[45][46] Evidence is weaker for the atypical antipsychotics, such as risperidone, olanzapine and quetiapine.[46][52] British professional guidelines by the National Institute for Health and Clinical Excellence advise haloperidol or olanzapine.[45] Antipsychotics however not supported for the treatment or prevention of delirium among those who are in hospital.[5]
Benzodiazepines themselves can cause delirium or worsen it,[46] and lack a reliable evidence base.[53] However, if delirium is due to alcohol withdrawal or benzodiazepine withdrawal or if antipsychotics are contraindicated (e.g. in Parkinson's disease or neuroleptic malignant syndrome), then benzodiazepines are recommended.[46] Similarly, people with dementia with Lewy bodies may have significant side-effects to antipsychotics, and should either be treated with a small dose or not at all.[45]
The antidepressant trazodone is occasionally used in the treatment of delirium, but it carries a risk of oversedation, and its use has not been well studied.[46]
Prognosis
There is substantial evidence that delirium results in long-term poor outcomes in older persons admitted to hospital.[54] This systematic review only included studies that looked for an independent effect of delirium (i.e., after accounting for other associations with poor outcomes, for example co-morbidity or illness severity).
In older persons admitted to hospital, individuals experiencing delirium are twice as likely to die than those who do not (meta-analysis of 12 studies).[54] In the only prospective study conducted in the general population, older persons reporting delirium also showed higher mortality (60% increase).[55]
Institutionalisation was also twice as likely after an admission with delirium (meta-analysis of 7 studies).[54] In a community-based population examining individuals after an episode of severe infection (though not specifically delirium), these persons acquired more functional limitations (i.e. required more assistance with their care needs) than those not experiencing infection.[56] After an episode of delirium in the general population, functional dependence increased threefold.[55]
The association between delirium and dementia is complex. The systematic review estimated a 13-fold increase in dementia after delirium (meta-analysis of 2 studies).[54] However, it is difficult to be certain that this is accurate because the population admitted to hospital includes persons with undiagnosed dementia (i.e. the dementia was present before the delirium, rather than caused by it). In prospective studies, people hospitalised from any cause appear to be at greater risk of dementia[57] and faster trajectories of cognitive decline,[57][58] but these studies did not specifically look at delirium. In the only population-based prospective study of delirium, older persons had an eight-fold increase in dementia and faster cognitive decline.[55] The same association is also evident in persons already diagnosed with Alzheimer’s dementia.[59]
Epidemiology
The highest rates of delirium (often 50% to 75% of people) is seen among those who are critically ill in the intensive care unit (ICU)[42] As a result this was referred to as "ICU psychosis" or "ICU syndrome", terms largely abandoned for the more widely accepted term ICU delirium. Since the advent of validated and easy-to-implement delirium instruments for ICU patients such as the Confusion Assessment Method for the ICU (CAM-ICU)[40] and the Intensive Care Delirium Screening Checkllist (IC-DSC).,[41] of the hundreds of thousands of ICU patients who develop delirium in ICUs every year, it has been recognized that most of them belong to the hypoactive variety, which is easily missed and invisible to the managing teams unless actively monitored using such instruments. The causes of delirium in such patients depend on the underlying illnesses, new problems like sepsis and low oxygen levels, and the sedative and pain medicines that are nearly universally given to all ICU patients. Outside the ICU, on hospital wards and in nursing homes, the problem of delirium is also a very important medical problem, especially for older patients.
The most recent area of the hospital in which delirium is just beginning to be monitored routinely in many centers is the Emergency Department, where the prevalence of delirium among older adults is about 10%.[60] A systematic review of delirium in general medical inpatients showed that estimates of delirium prevalence on admission ranged from 10 to 31%.[61] About 5% to 10% of older adults who are admitted to hospital develop a new episode of delirium while in hospital.[60] Estimates of the prevalence of delirium in nursing homes are between 10% [60] to 45%.[62]
Society and culture
Delirium is one of the oldest forms of mental disorder known in medical history.[63]
Sims (1995, p. 31) points out a "superb detailed and lengthy description" of delirium in The Stroller's Tale from Charles Dickens' The Pickwick Papers.[64][65]
Costs
In the USA, the cost of a patient admission with delirium is estimated at between $16k and $64k, suggesting the national burden of delirium may range from $38 bn to $150 bn per year (2008 estimate).[66] In the UK, the cost is estimated as £13k per admission.[67]
See also
References
- ↑ Clegg, A; Young, JB (January 2011). "Which medications to avoid in people at risk of delirium: a systematic review". Age and ageing. 40 (1): 23–9. doi:10.1093/ageing/afq140. PMID 21068014.
- ↑ Gleason OC (March 2003). "Delirium". Am Fam Physician. 67 (5): 1027–34. PMID 12643363.
- 1 2 3 4 5 6 Siddiqi, Najma; Harrison, Jennifer K.; Clegg, Andrew; Teale, Elizabeth A.; Young, John; Taylor, James; Simpkins, Samantha A. (2016-03-11). "Interventions for preventing delirium in hospitalised non-ICU patients". The Cochrane Database of Systematic Reviews. 3: CD005563. doi:10.1002/14651858.CD005563.pub3. ISSN 1469-493X. PMID 26967259.
- ↑ Ely EW; Shintani A; Truman B; et al. (2004). "Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit". JAMA. 291 (14): 1753–62. doi:10.1001/jama.291.14.1753. PMID 15082703.
- 1 2 Neufeld, KJ; Yue, J; Robinson, TN; Inouye, SK; Needham, DM (April 2016). "Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis.". Journal of the American Geriatrics Society. 64 (4): 705–14. doi:10.1111/jgs.14076. PMID 27004732.
- ↑ Attard A, Ranjith G, Taylor D (August 2008). "Delirium and its treatment". CNS Drugs. 22 (8): 631–44. doi:10.2165/00023210-200822080-00002. PMID 18601302.
- 1 2 3 4 5 6 7 8 9 10 Hales E and Yudofsky JA, eds, The American Psychiatric Press Textbook of Psychiatry, Washington, DC: American Psychiatric Publishing, Inc., 2003
- ↑ Gelder, Mayou, Geddes (2005). Psychiatry. (Pg.138) New York, NY: Oxford University Press Inc.
- ↑ "Delirium - Cleveland Clinic". Retrieved 2007-06-11.
- 1 2 Trzepacz, P; Meagher, DJ; Leonard, M. (2011). James L Levenson, eds. Delirium. The American Psychiatric Publishing Textbook of Psychosomatic Medicine: Psychiatric Care of the Medically Ill (2 ed.). Washington, DC: American Psychiatric Pub. ISBN 9781585623792. OCLC 663370391.
- ↑ American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington DC: American Psychiatric Association. ISBN 978-0890420256.
- ↑ de Rooij, SE; Schuurmans, MJ; van der Mast, RC; Levi, M (July 2005). "Clinical subtypes of delirium and their relevance for daily clinical practice: a systematic review.". International journal of geriatric psychiatry. 20 (7): 609–15. doi:10.1002/gps.1343. PMID 16021665.
- ↑ Meagher, D (February 2009). "Motor subtypes of delirium: past, present and future.". International review of psychiatry (Abingdon, England). 21 (1): 59–73. doi:10.1080/09540260802675460. PMID 19219713.
- ↑ Leentjens, AF; Rundell, J; Rummans, T; Shim, JJ; Oldham, R; Peterson, L; Philbrick, K; Soellner, W; Wolcott, D; Freudenreich, O (August 2012). "Delirium: An evidence-based medicine (EBM) monograph for psychosomatic medicine practice, commissioned by the Academy of Psychosomatic Medicine (APM) and the European Association of Consultation Liaison Psychiatry and Psychosomatics (EACLPP).". Journal of psychosomatic research. 73 (2): 149–52. doi:10.1016/j.jpsychores.2012.05.009. PMID 22789420.
- ↑ Cole, MG; Ciampi, A; Belzile, E; Zhong, L (January 2009). "Persistent delirium in older hospital patients: a systematic review of frequency and prognosis.". Age and ageing. 38 (1): 19–26. doi:10.1093/ageing/afn253. PMID 19017678.
- ↑ Jackson, JC; Mitchell, N; Hopkins, RO (July 2009). "Cognitive functioning, mental health, and quality of life in ICU survivors: an overview.". Critical Care Clinics. 25 (3): 615–28, x. doi:10.1016/j.ccc.2009.04.005. PMID 19576534.
- ↑ Hopkins, RO; Jackson, JC (September 2006). "Long-term neurocognitive function after critical illness.". Chest. 130 (3): 869–78. doi:10.1378/chest.130.3.869. PMID 16963688.
- ↑ Inouye, SK; Bogardus Jr., ST; Charpentier, PA; Leo-Summers, L; Acampora, D; Holford, TR; Cooney Jr., LM (Mar 4, 1999). "A multicomponent intervention to prevent delirium in hospitalized older patients.". The New England Journal of Medicine. 340 (9): 669–76. doi:10.1056/NEJM199903043400901. PMID 10053175.
- ↑ Hshieh, TT; Fong, TG; Marcantonio, ER; Inouye, SK (July 2008). "Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence.". The journals of gerontology. Series A, Biological sciences and medical sciences. 63 (7): 764–72. doi:10.1093/gerona/63.7.764. PMC 2917793
 . PMID 18693233.
. PMID 18693233. - 1 2 Cunningham, C; Maclullich, AM (Aug 3, 2012). "At the extreme end of the psychoneuroimmunological spectrum: Delirium as a maladaptive sickness behaviour response.". Brain, behavior, and immunity. 28: 1–13. doi:10.1016/j.bbi.2012.07.012. PMID 22884900.
- ↑ Hall, RJ; Shenkin, SD; Maclullich, AM (2011). "A systematic literature review of cerebrospinal fluid biomarkers in delirium.". Dementia and geriatric cognitive disorders. 32 (2): 79–93. doi:10.1159/000330757. PMID 21876357.
- ↑ Witlox, J; Kalisvaart, KJ; de Jonghe, JF; Verwey, NA; van Stijn, MF; Houdijk, AP; Traast, HS; MacLullich, AM; van Gool, WA; Eikelenboom, P (July 2011). "Cerebrospinal fluid β-amyloid and tau are not associated with risk of delirium: a prospective cohort study in older adults with hip fracture.". Journal of the American Geriatrics Society. 59 (7): 1260–7. doi:10.1111/j.1532-5415.2011.03482.x. PMID 21718268.
- ↑ Soiza, RL; Sharma, V; Ferguson, K; Shenkin, SD; Seymour, DG; Maclullich, AM (September 2008). "Neuroimaging studies of delirium: a systematic review.". Journal of psychosomatic research. 65 (3): 239–48. doi:10.1016/j.jpsychores.2008.05.021. PMID 18707946.
- ↑ Gunther, ML; Morandi, A; Krauskopf, E; Pandharipande, P; Girard, TD; Jackson, JC; Thompson, J; Shintani, AK; Geevarghese, S; Miller III, RR; Canonico, A; Merkle, K; Cannistraci, CJ; Rogers, BP; Gatenby, JC; Heckers, S; Gore, JC; Hopkins, RO; Ely, EW; for the VISIONS Investigation (VISualizing Icu SurvivOrs Neuroradiological Sequelae) (July 2012). "The association between brain volumes, delirium duration, and cognitive outcomes in intensive care unit survivors: the VISIONS cohort magnetic resonance imaging study*". Critical Care Medicine. 40 (7): 2022–32. doi:10.1097/ccm.0b013e318250acc0.
- ↑ Morandi, A; Rogers, BP; Gunther, ML; Merkle, K; Pandharipande, P; Girard, TD; Jackson, JC; Thompson, J; Shintani, AK; Geevarghese, S; Miller III, RR; Canonico, A; Cannistraci, CJ; Gore, JC; Ely, EW; Hopkins, RO; for the VISIONS Investigation (VISualizing Icu SurvivOrs Neuroradiological Sequelae) (July 2012). "The relationship between delirium duration, white matter integrity, and cognitive impairment in intensive care unit survivors as determined by diffusion tensor imaging: the VISIONS prospective cohort magnetic resonance imaging study*.". Critical Care Medicine. 40 (7): 2182–9. doi:10.1097/CCM.0b013e318250acdc. PMID 22584766.
- ↑ Hatano, Y; Narumoto, J; Shibata, K; Matsuoka, T; Taniguchi, S; Hata, Y; Yamada, K; Yaku, H; Fukui, K (Sep 21, 2012). "White-Matter Hyperintensities Predict Delirium After Cardiac Surgery.". The American Journal of Geriatric Psychiatry: 1. doi:10.1097/JGP.0b013e31826d6b10. PMID 23000936.
- ↑ Shioiri, A; Kurumaji, A; Takeuchi, T; Matsuda, H; Arai, H; Nishikawa, T (August 2010). "White matter abnormalities as a risk factor for postoperative delirium revealed by diffusion tensor imaging.". The American Journal of Geriatric Psychiatry. 18 (8): 743–53. doi:10.1097/JGP.0b013e3181d145c5. PMID 20220599.
- ↑ Choi, SH; Lee, H; Chung, TS; Park, KM; Jung, YC; Kim, SI; Kim, JJ (May 2012). "Neural network functional connectivity during and after an episode of delirium.". The American Journal of Psychiatry. 169 (5): 498–507. doi:10.1176/appi.ajp.2012.11060976. PMID 22549209.
- ↑ Engel, GL; Romano, J (Fall 2004). "Delirium, a syndrome of cerebral insufficiency. 1959.". The Journal of neuropsychiatry and clinical neurosciences. 16 (4): 526–38. doi:10.1176/appi.neuropsych.16.4.526. PMID 15616182.
- ↑ van der Kooi, AW; Leijten, FS; van der Wekken, RJ; Slooter, AJ (Fall 2012). "What are the opportunities for EEG-based monitoring of delirium in the ICU?". The Journal of neuropsychiatry and clinical neurosciences. 24 (4): 472–7. doi:10.1176/appi.neuropsych.11110347. PMID 23224454.
- ↑ Janz, DR; Abel, TW; Jackson, JC; Gunther, ML; Heckers, S; Ely, EW (September 2010). "Brain autopsy findings in intensive care unit patients previously suffering from delirium: a pilot study.". Journal of critical care. 25 (3): 538.e7–12. doi:10.1016/j.jcrc.2010.05.004. PMID 20580199.
- ↑ Munster, BC; Aronica, E; Zwinderman, AH; Eikelenboom, P; Cunningham, C; Rooij, SE (December 2011). "Neuroinflammation in delirium: a postmortem case-control study.". Rejuvenation research. 14 (6): 615–22. doi:10.1089/rej.2011.1185. PMID 21978081.
- ↑ Bellelli, G.; Nobili, A.; Annoni, G.; Morandi, A.; Djade, C. D.; Meagher, D. J.; Maclullich, A. M. J.; Davis, D.; Mazzone, A. (2015-08-31). "Under-detection of delirium and impact of neurocognitive deficits on in-hospital mortality among acute geriatric and medical wards". European Journal of Internal Medicine. 26: 696–704. doi:10.1016/j.ejim.2015.08.006. ISSN 1879-0828. PMID 26333532.
- ↑ Schuurmans, Marieke J.; Shortridge-Baggett, Lillie M.; Duursma, Sijmen A. (2003-01-01). "The Delirium Observation Screening Scale: a screening instrument for delirium". Research and Theory for Nursing Practice. 17 (1): 31–50. doi:10.1891/rtnp.17.1.31.53169. ISSN 1541-6577. PMID 12751884.
- ↑ Gaudreau, Jean-David; Gagnon, Pierre; Harel, François; Tremblay, Annie; Roy, Marc-André (2005-04-01). "Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale". Journal of Pain and Symptom Management. 29 (4): 368–375. doi:10.1016/j.jpainsymman.2004.07.009. ISSN 0885-3924. PMID 15857740.
- ↑ Inouye, S. K.; van Dyck, C. H.; Alessi, C. A.; Balkin, S.; Siegal, A. P.; Horwitz, R. I. (1990-12-15). "Clarifying confusion: the confusion assessment method. A new method for detection of delirium". Annals of Internal Medicine. 113 (12): 941–948. doi:10.7326/0003-4819-113-12-941. ISSN 0003-4819. PMID 2240918.
- ↑ Voyer, Philippe; Champoux, Nathalie; Desrosiers, Johanne; Landreville, Philippe; McCusker, Jane; Monette, Johanne; Savoie, Maryse; Richard, Sylvie; Carmichael, Pierre-Hugues (2015-01-01). "Recognizing acute delirium as part of your routine [RADAR]: a validation study". BMC nursing. 14: 19. doi:10.1186/s12912-015-0070-1. ISSN 1472-6955. PMC 4384313
 . PMID 25844067.
. PMID 25844067. - ↑ Bellelli, Giuseppe; Morandi, Alessandro; Davis, Daniel H. J.; Mazzola, Paolo; Turco, Renato; Gentile, Simona; Ryan, Tracy; Cash, Helen; Guerini, Fabio (2014-07-01). "Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people". Age and Ageing. 43 (4): 496–502. doi:10.1093/ageing/afu021. ISSN 1468-2834. PMC 4066613
 . PMID 24590568.
. PMID 24590568. - ↑ Jacobi, J; Fraser, GL; Coursin, DB; Riker, RR; Fontaine, D; Wittbrodt, ET; Chalfin, DB; Masica, MF; Bjerke, HS; Coplin, WM; Crippen, DW; Fuchs, BD; Kelleher, RM; Marik, PE; Nasraway Jr., SA; Murray, MJ; Peruzzi, WT; Lumb, PD; Task Force of the American College of Critical Care Medicine (ACCM) of the Society of Critical Care Medicine (SCCM), American Society of Health-System Pharmacists (ASHP), American College of Chest Physicians (January 2002). "Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult.". Critical Care Medicine. 30 (1): 119–41. doi:10.1097/00003246-200201000-00020. PMID 11902253.
- 1 2 Ely EW; Inouye SK; Bernard GR; et al. (December 2001). "Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU)". JAMA. 286 (21): 2703–10. doi:10.1001/jama.286.21.2703. PMID 11730446.
- 1 2 Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (May 2001). "Intensive Care Delirium Screening Checklist: evaluation of a new screening tool". Intensive Care Med. 27 (5): 859–64. doi:10.1007/s001340100909. PMID 11430542.
- 1 2 3 Ely, E.W.; et al. "ICU Delirium and Cognitive Impairment Study Group". Retrieved 6 December 2012.
- ↑ Jones, SF; Pisani, MA (April 2012). "ICU delirium: an update.". Current opinion in critical care. 18 (2): 146–51. doi:10.1097/MCC.0b013e32835132b9. PMID 22322260.
- ↑ EW Ely (March 2014). "Confusion Assessment Method for the ICU (CAM-ICU): The Complete Training Manual." (PDF). ICU Delirium. pp. 1–32. Retrieved October 25, 2016.
- 1 2 3 4 5 6 7 8 National Institute for Health and Clinical Excellence. Clinical guideline 103: Delirium. London, 2010.
- 1 2 3 4 5 6 7 8 9 Inouye SK (March 2006). "Delirium in older persons". N. Engl. J. Med. 354 (11): 1157–65. doi:10.1056/NEJMra052321. PMID 16540616.
- ↑ Boltz, Marie; Capezuti, Elizabeth; Fulmer, Terry T.; Zwicker, DeAnne, eds. (2011). Evidence-based geriatric nursing protocols for best practice (4th ed.). New York, NY: Springer Publishing Co. ISBN 9780826171283.
- ↑ Martinez, F; Tobar, C; Hill, N (March 2015). "Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature.". Age and ageing. 44 (2): 196–204. doi:10.1093/ageing/afu173. PMID 25424450.
- ↑ "Pharmacologic prevention of postoperative delirium.". Z Gerontol Geriatr. 47: 105–9. Feb 2014. doi:10.1007/s00391-013-0598-1. PMID 24619041.
- 1 2 3 4 5 6 Flaherty, J.; Little, M. (2011). "Matching the Environment to Patients with Delirium: Lessons Learned from the Delirium Room, a Restraint-Free Environment for Older Hospitalized Adults with Delirium". Journal of the American Geriatrics Society. 59: 295–300. doi:10.1111/j.1532-5415.2011.03678.x.
- ↑ Young, J.; Inouye, S. (2007). "Delirium in older people". British Medical Journal. 334 (7598): 842–846. doi:10.1136/bmj.39169.706574.AD. PMC 1853193
 . PMID 17446616.
. PMID 17446616. - ↑ Tyrer, Peter; Silk, Kenneth R., eds. (24 January 2008). "Delirium". Cambridge Textbook of Effective Treatments in Psychiatry (1st ed.). Cambridge University Press. pp. 175–184. ISBN 978-0-521-84228-0.
- ↑ Lonergan E, Luxenberg J, Areosa Sastre A, Wyller TB (2009). Lonergan, Edmund, ed. "Benzodiazepines for delirium". Cochrane Database Syst Rev (1): CD006379. doi:10.1002/14651858.CD006379.pub2. PMID 19160280.
- 1 2 3 4 Witlox, J; Eurelings, LS; de Jonghe, JF; Kalisvaart, KJ; Eikelenboom, P; van Gool, WA (Jul 28, 2010). "Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis.". JAMA: The Journal of the American Medical Association. 304 (4): 443–51. doi:10.1001/jama.2010.1013. PMID 20664045.
- 1 2 3 Davis, DH; Muniz Terrera, G; Keage, H; Rahkonen, T; Oinas, M; Matthews, FE; Cunningham, C; Polvikoski, T; Sulkava, R; MacLullich, AM; Brayne, C (September 2012). "Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study.". Brain : a journal of neurology. 135 (Pt 9): 2809–16. doi:10.1093/brain/aws190. PMC 3437024
 . PMID 22879644.
. PMID 22879644. - ↑ Iwashyna, TJ; Ely, EW; Smith, DM; Langa, KM (Oct 27, 2010). "Long-term cognitive impairment and functional disability among survivors of severe sepsis.". JAMA: The Journal of the American Medical Association. 304 (16): 1787–94. doi:10.1001/jama.2010.1553. PMC 3345288
 . PMID 20978258.
. PMID 20978258. - 1 2 Ehlenbach, WJ; Hough, CL; Crane, PK; Haneuse, SJ; Carson, SS; Curtis, JR; Larson, EB (Feb 24, 2010). "Association between acute care and critical illness hospitalization and cognitive function in older adults.". JAMA: The Journal of the American Medical Association. 303 (8): 763–70. doi:10.1001/jama.2010.167. PMC 2943865
 . PMID 20179286.
. PMID 20179286. - ↑ Wilson, RS; Hebert, LE; Scherr, PA; Dong, X; Leurgens, SE; Evans, DA (Mar 27, 2012). "Cognitive decline after hospitalization in a community population of older persons.". Neurology. 78 (13): 950–6. doi:10.1212/WNL.0b013e31824d5894. PMID 22442434.
- ↑ Fong, TG; Jones, RN; Shi, P; Marcantonio, ER; Yap, L; Rudolph, JL; Yang, FM; Kiely, DK; Inouye, SK (May 5, 2009). "Delirium accelerates cognitive decline in Alzheimer disease.". Neurology. 72 (18): 1570–5. doi:10.1212/WNL.0b013e3181a4129a. PMC 2677515
 . PMID 19414723.
. PMID 19414723. - 1 2 3 Canadian Coalition for Seniors' Mental Health (2006). National Guidelines for Seniors' Mental Health: The Assessment and Treatment of Delirium. Canadian Coalition for Seniors' Mental Health.
- ↑ Siddiqi, N.; House, AO; Holmes, JD (30 June 2006). "Occurrence and outcome of delirium in medical in-patients: a systematic literature review". Age and Ageing. 35 (4): 350–364. doi:10.1093/ageing/afl005. PMID 16648149.
- ↑ Voyer, Philippe; Richard, Sylvie; Doucet, Lise; Carmichael, Pierre-Hugues (2009). "Detecting Delirium and Subsyndromal Delirium Using Different Diagnostic Criteria among Demented Long-Term Care Residents". Journal of the American Medical Directors Association. 10 (3): 181–188. doi:10.1016/j.jamda.2008.09.006.
- ↑ Berrios GE (November 1981). "Delirium and confusion in the 19th century: a conceptual history". Br J Psychiatry. 139 (5): 439–49. doi:10.1192/bjp.139.5.439. PMID 7037094.
- ↑ Sims, Andrew (2002). Symptoms in the mind: an introduction to descriptive psychopathology. Philadelphia: W. B. Saunders. ISBN 0-7020-2627-1.
- ↑ Dickens, C. (1837) The Pickwick Papers. Available for free on Project Gutenberg.
- ↑ Leslie, DL; Marcantonio, ER; Zhang, Y; Leo-Summers, L; Inouye, SK (Jan 14, 2008). "One-year health care costs associated with delirium in the elderly population.". Archives of Internal Medicine. 168 (1): 27–32. doi:10.1001/archinternmed.2007.4. PMID 18195192.
- ↑ Akunne, A; Murthy, L; Young, J (May 2012). "Cost-effectiveness of multi-component interventions to prevent delirium in older people admitted to medical wards.". Age and ageing. 41 (3): 285–91. doi:10.1093/ageing/afr147. PMID 22282171.
Further reading
- Macdonald, Alastair; Lindesay, James; Rockwood, Kenneth (2002). Delirium in old age. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-263275-2.
- Grassi, Luigi; Caraceni, Augusto (2003). Delirium: acute confusional states in palliative medicine. Oxford: Oxford University Press. ISBN 0192631993.
- Newman, James K.; Slater, Christopher T., eds. (2012). Delirium: causes, diagnosis and treatment. Hauppauge, N.Y.: Nova Science Publisher's, Inc. ISBN 978-1613242940.
External links
| Wikisource has the text of the 1911 Encyclopædia Britannica article Delirium . |
- American Delirium Society
- European Delirium Association
- Australasian Delirium Association
- CAM-ICU Training Manual
- CAM-ICU online
- RADAR tool
- Hospital Elder Life Program
- Healthcare Improvement Scotland delirium resources
- The 4AT delirium assessment tool website