Cremaster muscle
| Cremaster muscle | |
|---|---|
 The cremaster muscle appears as a thin layer just superficial to the tunica vaginalis. | |
| Details | |
| Origin | Inguinal ligament |
| Insertion | Tunica vaginalis |
| Artery | Cremasteric artery |
| Nerve | Genital branch of genitofemoral nerve |
| Actions | raise and lower the scrotum |
| Identifiers | |
| Latin | musculus cremaster |
| TA | A04.5.01.018 |
| FMA | 21531 |
The cremaster muscle is a muscle that covers the testis and the spermatic cord.
Structure
In human males, the cremaster muscle is a thin layer of skeletal muscle found in the inguinal canal and scrotum between the external and internal layers of spermatic fascia, surrounding the testis and spermatic cord. The cremaster muscle is a paired structure, there being one on each side of the body.
Anatomically, the lateral cremaster muscle originates from the internal oblique muscle, just superior to the inguinal canal, and the middle of the inguinal ligament. The medial cremaster muscle, which sometimes is absent, originates from the pubic tubercle and sometimes the lateral pubic crest. Both insert into the tunica vaginalis underneath the testis.
Blood supply
The cremaster muscle is supplied by the cremasteric artery which is a branch of inferior epigastric artery.
Innervation
The cremaster muscle is innervated from the genital branch of the genitofemoral nerve. It receives distinctly different innervation and vascular supply in comparison to the internal oblique.
Development
The cremaster develops to its full extent only in males; in females it is represented by only a few muscle loops.
In female humans, the cremaster muscle is smaller and is found on the round ligament.
In rats, it has been shown that cremaster muscles developed from the gubernacular bulb.[1]
Function
Contraction
The cremaster muscle's function is to raise and lower the testes in order to regulate scrotal temperature for optimal spermatogenesis and survival of the resultant spermatozoa. It does this by increasing or decreasing the exposed surface area of the surrounding tissue, allowing faster or slower dissipation of body heat.
The cremaster muscle is an involuntary muscle and contraction can occur during arousal which can prevent injury to the testicles during sex.
Contraction can also occur during moments of extreme fear, possibly to help avoid injuring the testes while dealing with a fight or flight situation.
Clinically, a reflex arc termed the cremasteric reflex can be demonstrated by lightly stroking the skin of the inner thigh downwards from the hip towards the knee. This causes the cremaster muscle on the same side to rapidly contract, raising the testicle.
The cremaster can also be contracted voluntarily, by contracting the pubococcygeus muscle (using Kegels), or by flexing and tightening the abdominal muscles.
Clinical relevance
The cremaster muscle occasionally experiences painful spasms or cramps in adult males which can be chronic and debilitating. Treatment for these spasms ranges from minor surgery to injection with botulinum-a toxin to the regular application of heat to relax the muscle. Surgery, including the excision of the cremaster muscle, has apparently been able to provide complete relief from this condition without significant side effects.[2][3]
History
The word is derived from the transitive Greek verb "I hang" (Greek: κρεμάννυμι).
Additional images
-

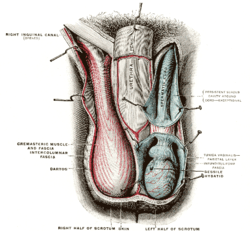
The scrotum.
-
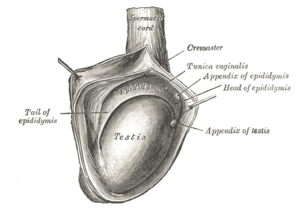
The right testis, exposed by laying open the tunica vaginalis.
References
- ↑ Hrabovszky, Z.; Pilla, N. D.; Yap, T.; Farmer, P. J.; Hutson, J. M.; Carlin, J. B. (2002). "Role of the gubernacular bulb in cremaster muscle development of the rat". The Anatomical Record. 267 (2): 159–165. doi:10.1002/ar.10092. PMID 11997885.
- ↑ Baty, John A. (5 May 1956). "Cremasteric cramp with testicular retraction" (PDF). British Medical Journal. 1 (4974): 1014–1015. doi:10.1136/bmj.1.4974.1014. ISSN 0959-8138. PMC 1979762
 . PMID 13304412. Retrieved 11 March 2012.
. PMID 13304412. Retrieved 11 March 2012. - ↑ Mori, Ryan; Sandip Vasavada; Diana Baker; Edmund Sabanegh Jr (July 2011). "Treatment of debilitating cremasteric synkinesia With intracremasteric botulinum-a toxin injections". Urology. Cleveland, OH: Glickman Urological and Kidney Institute. 78 (1): 214–216. doi:10.1016/j.urology.2011.03.011. ISSN 0090-4295. Retrieved 11 March 2012.
External links
- -731185075 at GPnotebook
- Anatomy photo:36:07-0102 at the SUNY Downstate Medical Center - "Inguinal Region, Scrotum and Testes: Layers of the Spermatic Cord"